Arch Hand Microsurg.
2019 Dec;24(4):303-310. 10.12790/ahm.2019.24.4.303.
Dorsal Translation of Ulnar Head after the Arthroscopic Wafer Procedure for Ulnar Impaction Syndrome
- Affiliations
-
- 1Department of Orthopedic Surgery, Soonchunhyang University Bucheon Hospital, Bucheon, Korea. kbsos@schmc.ac.kr
- 2Department of Orthopedic Surgery, Soonchunhyang University Cheonan Hospital, Cheonan, Korea.
- 3Department of Orthopedic Surgery, Soonchunhyang University Seoul Hospital, Seoul, Korea.
- KMID: 2464465
- DOI: http://doi.org/10.12790/ahm.2019.24.4.303
Abstract
- PURPOSE
The purpose of this study was to evaluate the results of the arthroscopic wafer procedure (AWP) for ulnar impaction syndrome (UIS) and identify preoperative factors and degree of distal radioulnar joint (DRUJ) translation that could assist in predicting outcomes.
METHODS
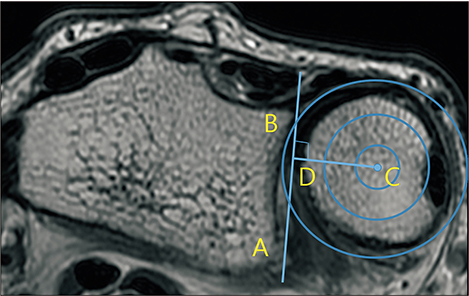
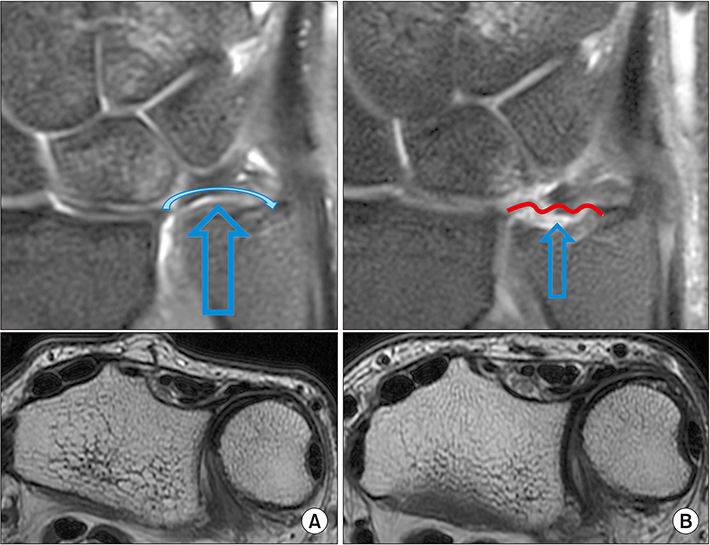
We retrospectively reviewed the medical records of 9 patients (11 wrists) who underwent AWP for UIS. Among these, 5 cases were converted to secondary ulnar shortening osteotomy and were categorized to group A and the remaining 6 cases were categorized to group B. The ulnar variance (UV), radioulnar ratio (RUR) by computed tomography or magnetic resonance imaging (MRI), MRI evidence of mechanical impaction in the ulnar or lunate, grip power, Disability of Shoulder, Arm and Hand (DASH) score, and Mayo wrist score were examined before and after AWP.
RESULTS
The MRI evidence did not differ significantly between groups A and B (p>0.05). The average UV and RUR changed from 1.6±0.7 mm and 0.68±0.17 before AWP to −1.5±0.9 mm and 0.54±0.10 after AWP, respectively. The difference between the preoperative RUR (0.65) and postoperative RUR in group B (0.49) was significant (p=0.027, Pearson correlation coefficient=0.862). The grip strength, DASH score, and Mayo wrist score improved from 77.1%, 47.6, and 69.1 to 85.2%, 16.8, and 85.5, respectively.
CONCLUSION
If patients have persisting pain and DRUJ dorsal translation is not reduced after wafer procedure, secondary ulnar shortening osteotom may be required.
Keyword
MeSH Terms
Figure
Reference
-
1. Constantine KJ, Tomaino MM, Herndon JH, Sotereanos DG. Comparison of ulnar shortening osteotomy and the wafer resection procedure as treatment for ulnar impaction syndrome. J Hand Surg Am. 2000; 25:55–60.
Article2. Bernstein MA, Nagle DJ, Martinez A, Stogin JM Jr, Wiedrich TA. A comparison of combined arthroscopic triangular fibrocartilage complex debridement and arthroscopic wafer distal ulna resection versus arthroscopic triangular fibrocartilage complex debridement and ulnar shortening osteotomy for ulnocarpal abutment syndrome. Arthroscopy. 2004; 20:392–401.
Article3. Markolf KL, Tejwani SG, Benhaim P. Effects of wafer resection and hemiresection from the distal ulna on load-sharing at the wrist: a cadaveric study. J Hand Surg Am. 2005; 30:351–358.
Article4. Bickel KD. Arthroscopic treatment of ulnar impaction syndrome. J Hand Surg Am. 2008; 33:1420–1423.
Article5. Griska A, Feldon P. Wafer resection of the distal ulna. J Hand Surg Am. 2015; 40:2283–2288.
Article6. Lapner PC, Poitras P, Backman D, Giachino AA, Conway AF. The effect of the wafer procedure on pressure in the distal radioulnar joint. J Hand Surg Am. 2004; 29:80–84.
Article7. Nishiwaki M, Nakamura T, Nakao Y, Nagura T, Toyama Y. Ulnar shortening effect on distal radioulnar joint stability: a biomechanical study. J Hand Surg Am. 2005; 30:719–726.
Article8. Nakamura R, Horii E, Imaeda T, Nakao E, Kato H, Watanabe K. The ulnocarpal stress test in the diagnosis of ulnar-sided wrist pain. J Hand Surg Br. 1997; 22:719–723.
Article9. Rhee PC, Sauvé PS, Lindau T, Shin AY. Examination of the wrist: ulnar-sided wrist pain due to ligamentous injury. J Hand Surg Am. 2014; 39:1859–1862.
Article10. Ruland RT, Hogan CJ. The ECU synergy test: an aid to diagnose ECU tendonitis. J Hand Surg Am. 2008; 33:1777–1782.
Article11. Cooney WP, Linscheid RL, Dobyns JH. Triangular fibrocartilage tears. J Hand Surg Am. 1994; 19:143–154.
Article12. Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996; 29:602–608.13. Steyers CM, Blair WF. Measuring ulnar variance: a comparison of techniques. J Hand Surg Am. 1989; 14:607–612.
Article14. Levis CM, Yang Z, Gilula LA. Validation of the extensor carpi ulnaris groove as a predictor for the recognition of standard posteroanterior radiographs of the wrist. J Hand Surg Am. 2002; 27:252–257.
Article15. Lo IK, MacDermid JC, Bennett JD, Bogoch E, King GJ. The radioulnar ratio: a new method of quantifying distal radioulnar joint subluxation. J Hand Surg Am. 2001; 26:236–243.
Article16. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174.
Article17. Canham CD, Schreck MJ, Maqsoodi N, Messing S, Olles M, Elfar JC. Distal radioulnar joint reaction force following ulnar shortening: diaphyseal osteotomy versus wafer resection. J Hand Surg Am. 2015; 40:2206–2212.
Article18. Meftah M, Keefer EP, Panagopoulos G, Yang SS. Arthroscopic wafer resection for ulnar impaction syndrome: prediction of outcomes. Hand Surg. 2010; 15:89–93.
Article19. Gartland JJ Jr, Werley CW. Evaluation of healed Colles' fractures. J Bone Joint Surg Am. 1951; 33:895–907.
Article20. Park MJ, Kim JP. Reliability and normal values of various computed tomography methods for quantifying distal radioulnar joint translation. J Bone Joint Surg Am. 2008; 90:145–153.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Updates on Ulnar Impaction Syndrome
- Arthroscopy of the Wrist and Ulnar Shortening Osteotomy for the Treatment of the Ulnar Impaction Syndrome
- Intraoperative Arthroscopic Findings of Ulnar Impaction Syndrome
- Treatment of Ulnar Impaction Syndrome using Arthroscopy and Ulnar Shortening Osteotomy
- Ulnar Shortening Osteotomy for the Treatment of Ulnar Impaction Syndrome