Cancer Res Treat.
2019 Apr;51(2):788-796. 10.4143/crt.2018.120.
Comparative Effectiveness of Abdominal versus Laparoscopic Radical Hysterectomy for Cervical Cancer in the Postdissemination Era
- Affiliations
-
- 1Department of Nursing, Chosun University College of Medicine, Gwangju, Korea.
- 2Department of Public Health, Korea University, Seoul, Korea.
- 3Department of Obstetrics and Gynecology, Institute of Women's Life Medical Science, Yonsei University College of Medicine, Seoul, Korea. jungyunlee@yuhs.ac
- 4Department of Obstetrics and Gynecology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 5Division of Gynecologic Oncology, Obstetrics and Gynecology, Irvine Medical Center, University of California, Orange, CA, USA.
- 6Center for Uterine Cancer and Center for Clinical Trials, Hospital, National Cancer Center, Goyang, Korea.
- 7Cancer Healthcare Research Branch, Precision Medicine Branch, and Common Cancer Branch, Research Institute, National Cancer Center, Goyang, Korea.
- 8Department of Cancer Control & Population Health, Graduate School of Cancer Science and Policy, National Cancer Center, Goyang, Korea.
- 9Department of Obstetrics and Gynecology, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2464424
- DOI: http://doi.org/10.4143/crt.2018.120
Abstract
- PURPOSE
Despite the benefits of minimally invasive surgery for cervical cancer, there are a lack of randomized trials comparing laparoscopic radical hysterectomy and abdominal radical hysterectomy. We compared morbidity, cost of care, and survival between abdominal radical hysterectomy and laparoscopic radical hysterectomy for cervical cancer.
MATERIALS AND METHODS
We used the Korean nationwide database to identify women with cervical cancer who underwent radical hysterectomy from January 1, 2011 to December 31, 2014. Patients who underwent abdominal radical hysterectomy were compared to those who underwent laparoscopic radical hysterectomy. Perioperative morbidity, the use of adjuvant therapy, and survival were evaluated after propensity score balancing.
RESULTS
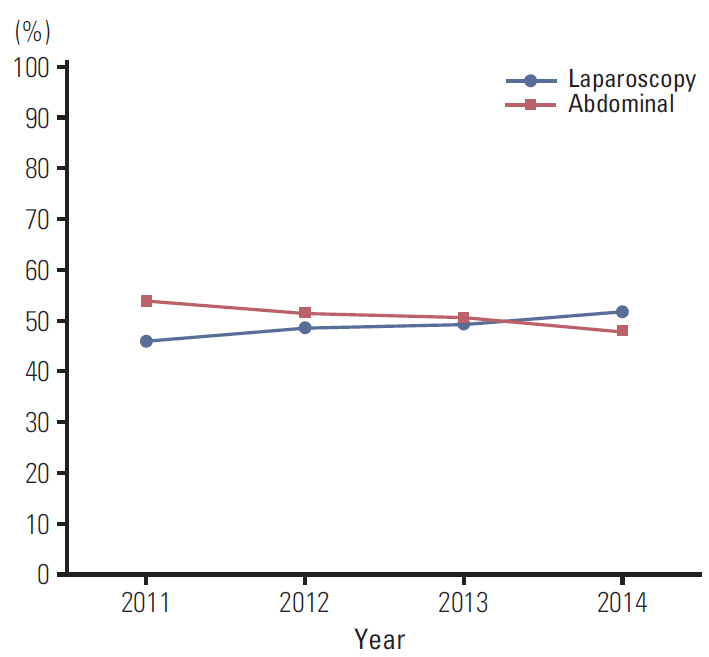
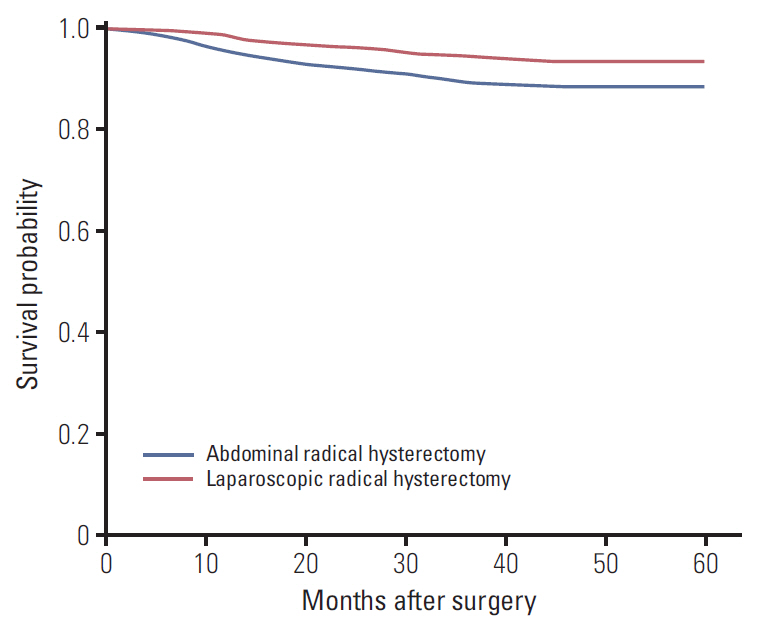
We identified 6,335 patients, including 3,235 who underwent abdominal radical hysterectomy and 3,100 who underwent laparoscopic radical hysterectomy. The use of laparoscopic radical hysterectomy increased from 46.1% in 2011 to 51.8% in 2014. Patients who were younger, had a more recent year of diagnosis, and were treated in the metropolitan area were more likely to undergo a laparoscopic procedure (p < 0.001). Compared to abdominal radical hysterectomy, laparoscopic radical hysterectomy was associated with lower rates of complication, fewertransfusions, a shorter hospital stay, less adjuvant therapy, and reduced total medical costs (p < 0.001). Laparoscopic surgery was associated with a better overall survival than abdominal operation (hazard ratio, 0.74; 95% confidence interval, 0.64 to 0.85).
CONCLUSION
In the postdissemination era, laparoscopic radical hysterectomy was associated with more favorable morbidity profiles, a lower cost of care, and comparable survival than abdominal radical hysterectomy.
MeSH Terms
Figure
Cited by 1 articles
-
After the Laparoscopic Approach to Cervical Cancer (LACC) trial: Korean Society of Gynecologic Oncology (KSGO) survey
Miseon Kim, Yong Beom Kim, Jae-Weon Kim
J Gynecol Oncol. 2019;30(5):. doi: 10.3802/jgo.2019.30.e108.
Reference
-
References
1. Dursun P, Gultekin M, Ayhan A. The history of radical hysterectomy. J Low Genit Tract Dis. 2011; 15:235–45.
Article2. Conrad LB, Ramirez PT, Burke W, Naumann RW, Ring KL, Munsell MF, et al. Role of minimally invasive surgery in gynecologic oncology: an updated survey of members of the Society of Gynecologic Oncology. Int J Gynecol Cancer. 2015; 25:1121–7.
Article3. Lee JY, Kim K, Lee TS, Kang S, Seong SJ, Kim JW, et al. Controversies in the management of endometrial cancer: a survey of the Korean Gynecologic Oncology Group. J Gynecol Oncol. 2015; 26:277–83.
Article4. Jung KW, Won YJ, Kong HJ, Oh CM, Shin A, Lee JS. Survival of korean adult cancer patients by stage at diagnosis, 2006-2010: national cancer registry study. Cancer Res Treat. 2013; 45:162–71.
Article5. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012; 62:10–29.
Article6. Bergmark K, Avall-Lundqvist E, Dickman PW, Henningsohn L, Steineck G. Vaginal changes and sexuality in women with a history of cervical cancer. N Engl J Med. 1999; 340:1383–9.
Article7. Scotti RJ, Bergman A, Bhatia NN, Ostergard DR. Urodynamic changes in urethrovesical function after radical hysterectomy. Obstet Gynecol. 1986; 68:111–20.8. Sood AK, Nygaard I, Shahin MS, Sorosky JI, Lutgendorf SK, Rao SS. Anorectal dysfunction after surgical treatment for cervical cancer. J Am Coll Surg. 2002; 195:513–9.
Article9. Nam JH, Park JY, Kim DY, Kim JH, Kim YM, Kim YT. Laparoscopic versus open radical hysterectomy in early-stage cervical cancer: long-term survival outcomes in a matched cohort study. Ann Oncol. 2012; 23:903–11.
Article10. Park JY, Kim DY, Kim JH, Kim YM, Kim YT, Nam JH. Laparoscopic versus open radical hysterectomy in patients with stage IB2 and IIA2 cervical cancer. J Surg Oncol. 2013; 108:63–9.
Article11. Abu-Rustum NR, Gemignani ML, Moore K, Sonoda Y, Venkatraman E, Brown C, et al. Total laparoscopic radical hysterectomy with pelvic lymphadenectomy using the argon-beam coagulator: pilot data and comparison to laparotomy. Gynecol Oncol. 2003; 91:402–9.
Article12. Bogani G, Cromi A, Uccella S, Serati M, Casarin J, Pinelli C, et al. Laparoscopic versus open abdominal management of cervical cancer: long-term results from a propensity-matched analysis. J Minim Invasive Gynecol. 2014; 21:857–62.
Article13. Frumovitz M, dos Reis R, Sun CC, Milam MR, Bevers MW, Brown J, et al. Comparison of total laparoscopic and abdominal radical hysterectomy for patients with early-stage cervical cancer. Obstet Gynecol. 2007; 110:96–102.
Article14. Magrina JF, Kho RM, Weaver AL, Montero RP, Magtibay PM. Robotic radical hysterectomy: comparison with laparoscopy and laparotomy. Gynecol Oncol. 2008; 109:86–91.
Article15. Wang W, Chu HJ, Shang CL, Gong X, Liu TY, Zhao YH, et al. Long-term oncological outcomes after laparoscopic versus abdominal radical hysterectomy in stage IA2 to IIA2 cervical cancer: a matched cohort study. Int J Gynecol Cancer. 2016; 26:1264–73.
Article16. Soliman PT, Frumovitz M, Sun CC, Dos Reis R, Schmeler KM, Nick AM, et al. Radical hysterectomy: a comparison of surgical approaches after adoption of robotic surgery in gynecologic oncology. Gynecol Oncol. 2011; 123:333–6.
Article17. Wright JD, Herzog TJ, Neugut AI, Burke WM, Lu YS, Lewin SN, et al. Comparative effectiveness of minimally invasive and abdominal radical hysterectomy for cervical cancer. Gynecol Oncol. 2012; 127:11–7.
Article18. Laparoscopic approach to cervical cancer (LACC) [Internet]. Bethesda, MD: U.S. National Library of Medicine;2018. [cited 2018 May 20]. Available from: https://clinicaltrials.gov/.19. World Health Organization. International statistical classification of diseases and related health problems. 10th rev. ed. Geneva: World Health Organization;1994.20. Korean Health Insurance Review and Assessment Service. Cost of health insurance medical care benefits. Seoul: Korean Health Insurance Review and Assessment Service;2016.21. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998; 36:8–27.
Article22. Sohn S, Kim J, Chung CK, Lee NR, Park E, Chang UK, et al. A nationwide epidemiological study of newly diagnosed spine metastasis in the adult Korean population. Spine J. 2016; 16:937–45.
Article23. Sohn S, Kim J, Chung CK, Lee NR, Sohn MJ, Kim SH. A nation-wide epidemiological study of newly diagnosed primary spine tumor in the adult Korean population, 2009-2011. J Korean Neurosurg Soc. 2017; 60:195–204.
Article24. Robins JM, Hernan MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000; 11:550–60.
Article25. Stukel TA, Fisher ES, Wennberg DE, Alter DA, Gottlieb DJ, Vermeulen MJ. Analysis of observational studies in the presence of treatment selection bias: effects of invasive cardiac management on AMI survival using propensity score and instrumental variable methods. JAMA. 2007; 297:278–85.26. Wright JD, Burke WM, Tergas AI, Hou JY, Huang Y, Hu JC, et al. Comparative effectiveness of minimally invasive hysterectomy for endometrial cancer. J Clin Oncol. 2016; 34:1087–96.
Article27. Barnett JC, Judd JP, Wu JM, Scales CD Jr, Myers ER, Havrilesky LJ. Cost comparison among robotic, laparoscopic, and open hysterectomy for endometrial cancer. Obstet Gynecol. 2010; 116:685–93.
Article28. Rauh-Hain JA. Comparative effectiveness of minimally invasive staging surgery in women with early stage cervical cancer. In : Proceedings of the Society of Gynecologic Oncologists; 2018 Mar 24-27; New Orleans, LA.29. Ramirez PT, Frumovitz M, Pareja R, Lopez A, Vieira MA, Ribeiro R. Phase III randomized trial of laparoscopic or robotic versus abdominal radical hysterectomy in patients with early-stage cervical cancer: LACC Trial. In : Proceedings of the 49th Annual Meeting of the Society of Gynecologic Oncologists; 2018 Mar 24-27; New Orleans, LA. Chicago, IL: Society of Gynecologic Oncology;2018.
Article30. Park JY, Nam JH. How should gynecologic oncologists react to the unexpected results of LACC trial? J Gynecol Oncol. 2018; 29:e74.
Article31. Kimmig R, Ind T. Minimally invasive surgery for cervical cancer: consequences for treatment after LACC Study. J Gynecol Oncol. 2018; 29:e75.
Article32. Kanao H, Aoki Y, Takeshima N. Unexpected result of minimally invasive surgery for cervical cancer. J Gynecol Oncol. 2018; 29:e73.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The twenty-first century role of Piver-Rutledge type III radical hysterectomy and FIGO stage IA, IB1, and IB2 cervical cancer in the era of robotic surgery: a personal perspective
- Vaginal evisceration after radical hysterectomy and adjuvant radiation
- Minimally invasive radical hysterectomy and the importance of avoiding cancer cell spillage for early-stage cervical cancer: a narrative review
- A comparison of robot assisted and abdominal radical hysterectomy (RH) for early stage cervical and endometrial cancer
- Novel vaginoplasty technique involving the use of peritoneal flaps during laparoscopic radical hysterectomy for early-stage cervical cancer