Hip Pelvis.
2019 Dec;31(4):190-199. 10.5371/hp.2019.31.4.190.
Characteristics and Surgical Outcomes of Intertrochanteric or Subtrochanteric Fractures Associated with Ipsilateral Femoral Shaft Fractures Treated with Closed Intramedullary Nailing: A Review of 31 Consecutive Cases over Four Years at a Single Institution
- Affiliations
-
- 1Department of Orthopaedic Surgery, Myung Eun Hospital, Busan, Korea.
- 2Department of Orthopaedic Surgery, Bio-Medical Research Institute, Pusan National University Hospital, Busan, Korea. namhoonmoon@gmail.com
- KMID: 2464235
- DOI: http://doi.org/10.5371/hp.2019.31.4.190
Abstract
- PURPOSE
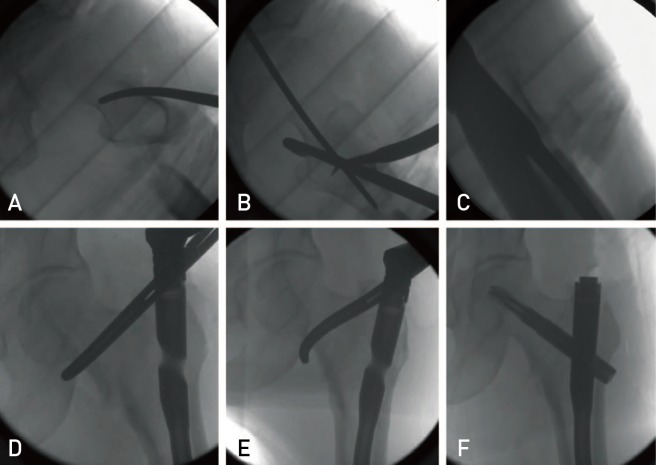
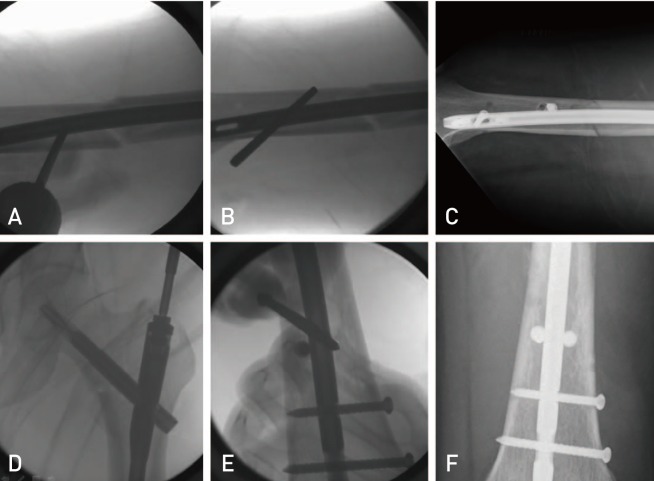
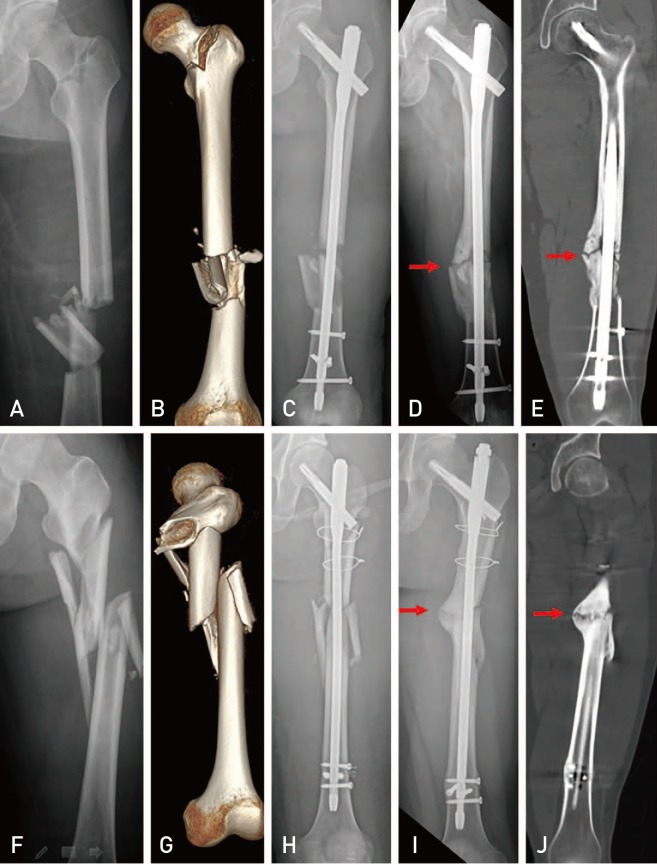
To evaluate the clinical characteristics of intertrochanteric or subtrochanteric fractures associated with ipsilateral femoral shaft fractures and assess the surgical outcomes of a novel, closed intramedullary nailing surgical approach designed to minimize fixation failure.
MATERIALS AND METHODS
Between May 2013 and April 2017, 31 patients with intertrochanteric or subtrochanteric fractures associated with ipsilateral femoral shaft fractures treated with closed intramedullary nailing or long proximal femoral nail antirotation (PFNA) were enrolled in this study. Preoperative data included age, sex, injury severity score, body mass index, location of shaft fracture, injury mechanism, accompanying traumatic injury, walking ability before injury, and surgical timing. Perioperative outcomes, including follow-up period, types of intramedullary nails, number of blocking screws used, operation time, and blood loss were assessed. Radiologic outcomes, including union rate, time from surgery to union, and femoral shortening, and clinical outcomes, including hip flexion, walking ability, and Harris hip score were also evaluated.
RESULTS
A total of 29 unions (93.5%) were achieved. The time to union was 16.8 months (range, 11-25 months) for hip fractures (15.7 weeks for intertrochanteric fractures and 21.7 weeks for subtrochanteric fractures) and 22.8 months for femoral shaft fractures. There were no significant differences in surgical outcomes between the two groups except for type of intramedullary nail.
CONCLUSION
Closed intramedullary nailing in the treatment of intertrochanteric or subtrochanteric fractures associated with ipsilateral femoral shaft fractures may be a good surgical option. However, fixation of femoral shaft fractures might not be sufficient depending on the implant design.
Keyword
MeSH Terms
Figure
Reference
-
1. Bali K, Gahlot N, Aggarwal S, Goni V. Cephalomedullary fixation for femoral neck/intertrochanteric and ipsilateral shaft fractures: surgical tips and pitfalls. Chin J Traumatol. 2013; 16:40–45. PMID: 23384870.2. Peskun C, McKee M, Kreder H, Stephen D, McConnell A, Schemitsch EH. Functional outcome of ipsilateral intertrochanteric and femoral shaft fractures. J Orthop Trauma. 2008; 22:102–106. PMID: 18349777.
Article3. Casey MJ, Chapman MW. Ipsilateral concomitant fractures of the hip and femoral shaft. J Bone Joint Surg Am. 1979; 61:503–509. PMID: 438236.
Article4. Olsen M, Goshulak P, Crookshank MC, et al. Biomechanical testing of a 3-hole versus a 4-hole sliding hip screw in the presence of a retrograde intramedullary nail for ipsilateral intertrochanteric and femur shaft fractures. J Orthop Trauma. 2018; 32:419–424. PMID: 29664884.
Article5. McConnell A, Zdero R, Syed K, Peskun C, Schemitsch E. The biomechanics of ipsilateral intertrochanteric and femoral shaft fractures: a comparison of 5 fracture fixation techniques. J Orthop Trauma. 2008; 22:517–524. PMID: 18758281.
Article6. Alho A. Concurrent ipsilateral fractures of the hip and shaft of the femur. A systematic review of 722 cases. Ann Chir Gynaecol. 1997; 86:326–336. PMID: 9474427.7. Alho A. Concurrent ipsilateral fractures of the hip and femoral shaft: a meta-analysis of 659 cases. Acta Orthop Scand. 1996; 67:19–28. PMID: 8615096.8. Kammerlander C, Doshi H, Gebhard F, et al. Long-term results of the augmented PFNA: a prospective multicenter trial. Arch Orthop Trauma Surg. 2014; 134:343–349. PMID: 24297215.
Article9. Jiamton C, Boernert K, Babst R, Beeres FJP, Link BC. The nail-shaft-axis of the of proximal femoral nail antirotation (PFNA) is an important prognostic factor in the operative treatment of intertrochanteric fractures. Arch Orthop Trauma Surg. 2018; 138:339–349. PMID: 29256184.
Article10. Mereddy P, Kamath S, Ramakrishnan M, Malik H, Donnachie N. The AO/ASIF proximal femoral nail antirotation (PFNA): a new design for the treatment of unstable proximal femoral fractures. Injury. 2009; 40:428–432. PMID: 19230885.
Article11. Robinson CM, Houshian S, Khan LA. Trochanteric-entry long cephalomedullary nailing of subtrochanteric fractures caused by low-energy trauma. J Bone Joint Surg Am. 2005; 87:2217–2226. PMID: 16203886.
Article12. Wu CC, Shih CH. Distal femoral nonunion treated with interlocking nailing. J Trauma. 1991; 31:1659–1662. PMID: 1749039.
Article13. Wu CC, Lee ZL. One-stage lengthening using a locked nailing technique for distal femoral shaft nonunions associated with shortening. J Orthop Trauma. 2004; 18:75–80. PMID: 14743025.
Article14. Shin WC, Moon NH, Jang JH, Lee HJ, Suh KT. Comparative study between biologic plating and intramedullary nailing for the treatment of subtrochanteric fractures: is biologic plating using LCP-DF superior to intramedullary nailing? Injury. 2017; 48:2207–2213. PMID: 28847590.
Article15. Shin WC, Moon NH, Jang JH, Jeong JY, Suh KT. Technical note and surgical outcomes of percutaneous cable fixation in subtrochanteric fracture: a review of 51 consecutive cases over 4 years in two institutions. Injury. 2019; 50:409–414. PMID: 30391068.
Article16. Delaney WM, Street DM. Fracture of femoral shaft with fracture of neck of same femur; treatment with medullary nail for shaft and Knowles pins for neck. J Int Coll Surg. 1953; 19:303–312. PMID: 13044949.17. Wang WY, Yang TF, Liu L, Pei FX, Xie LM. A comparative study of ipsilateral intertrochanteric and femoral shaft fractures treated with long proximal femoral nail antirotation or plate combinations. Orthop Surg. 2012; 4:41–46. PMID: 22290818.
Article18. Lin YB, Li RB, Xiong GS, et al. Treatment of middle-up part long-segment femoral fracture with long proximal femoral nail antirotation. Orthop Surg. 2015; 7:138–145. PMID: 26033995.
Article19. Jang JH, Ahn JM, Lee HJ, Moon NH. Surgical outcomes of biologic fixation for subtrochanteric fracture using locking compression plates. Hip Pelvis. 2017; 29:68–76. PMID: 28316965.
Article20. Eom TW, Kim JJ, Oh HK, Kim JW. Challenge to treat hypertrophic nonunion of the femoral shaft: the Poller screw augmentation technique. Eur J Orthop Surg Traumatol. 2016; 26:559–563. PMID: 27384959.
Article21. Hannah A, Aboelmagd T, Yip G, Hull P. A novel technique for accurate Poller (blocking) screw placement. Injury. 2014; 45:1011–1014. PMID: 24629702.
Article22. Özmeriç A, Alemdaroğlu KB. A more practical way to place a correct Poller (blocking) screw. Injury. 2016; 47:510–511.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Treatment of Ipsilateral Multi-Level Femoral Fracture Treated Using Antegrade Intramedullary Nail
- Treatment of the Fractures of the Shaft of the Femur with Intramedullary Nailing
- Subtrochanteric Fracture: Emphasis on Surgical Techniques in Nailing
- Subtrochanteric Femoral Fracture during Trochanteric Nailing for the Treatment of Femoral Shaft Fracture
- Flexible Intramedullary Nailing for Femoral Fractures