Clin Exp Otorhinolaryngol.
2019 Nov;12(4):399-404. 10.21053/ceo.2018.01151.
Nasopharyngeal Width and Its Association With Sleep-Disordered Breathing Symptoms in Children
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. kimemail@snubh.org
- KMID: 2462736
- DOI: http://doi.org/10.21053/ceo.2018.01151
Abstract
OBJECTIVES
Although adenotonsillar hypertrophy is the main cause of sleep-disordered breathing in children, surrounding anatomic factors, such as the width of the nasopharynx, can affect upper airway patency. However, there have been no reports of the association of nasopharyngeal width with sleep-disordered breathing in children. This study was undertaken to measure nasopharyngeal width in children undergoing adenotonsillectomy for sleep-disordered breathing and to investigate the clinical implications of this factor.
METHODS
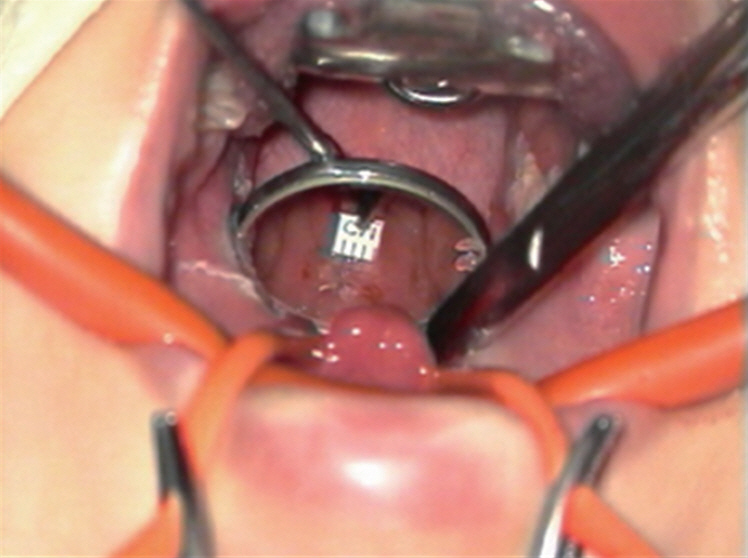
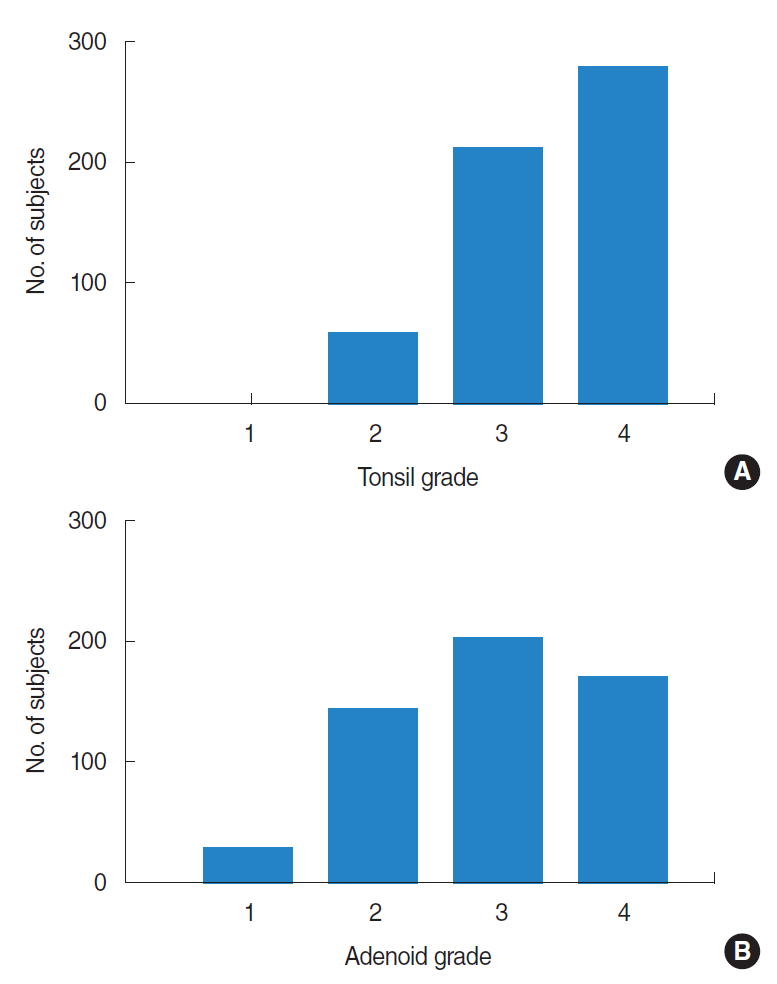
This was a retrospective study with a follow-up period of 1 year, performed at a tertiary referral center. We reviewed the operative records of children who underwent adenotonsillectomy at our center for symptoms of sleep-disordered breathing, such as snoring, apnea, and mouth breathing. The nasopharyngeal width was measured immediately before adenotonsillectomy, which was performed under general anesthesia with a microscopy-assisted mirror view. Adenotonsillar hypertrophy was graded on a four-point scale, and symptoms of sleep-disordered breathing were evaluated by using the Korean version of the Obstructive Sleep Apnea-18 questionnaire before and after surgery. The relationships between the average nasopharyngeal width and patient age and sex, adenotonsillar hypertrophy, and the Korean version of the Obstructive Sleep Apnea-18 score were analyzed.
RESULTS
The study included 549 children (343 boys) with a mean age of 6.0 years (range, 2 to 11 years). The average nasopharyngeal width was 11.9 mm (range, 7.0 to 18.0 mm) and increased with age (range, 11.2 to 13.3; β=0.264; P<0.001). At 1 year after surgery, children with a greater nasopharyngeal width at the time of surgery exhibited additional improvements in symptoms of obstruction relative to those at 1 month after surgery.
CONCLUSION
The average nasopharyngeal width in children is approximately 11.9 mm and exhibits a slight increase with age. The width of the nasopharynx may be a factor associated with the degree of improvement in symptoms of sleep-disordered breathing after adenotonsillectomy.
Keyword
MeSH Terms
Figure
Reference
-
1. Simsek G, Karacayli C, Ozel A, Arslan B, Muluk NB, Kilic R. Blood parameters as indicators of upper airway obstruction in children with adenoid or adenotonsillar hypertrophy. J Craniofac Surg. 2015; May. 26(3):e213–6.
Article2. Jeans WD, Fernando DC, Maw AR, Leighton BC. A longitudinal study of the growth of the nasopharynx and its contents in normal children. Br J Radiol. 1981; Feb. 54(638):117–21.
Article3. Papaioannou G, Kambas I, Tsaoussoglou M, Panaghiotopoulou-Gartagani P, Chrousos G, Kaditis AG. Age-dependent changes in the size of adenotonsillar tissue in childhood: implications for sleep-disordered breathing. J Pediatr. 2013; Feb. 162(2):269–74. e4.
Article4. Merati AL, Rieder AA. Normal endoscopic anatomy of the pharynx and larynx. Am J Med. 2003; Aug. 115 Suppl 3A:10S–14S.5. Handelman CS, Osborne G. Growth of the nasopharynx and adenoid development from one to eighteeen years. Angle Orthod. 1976; Jul. 46(3):243–59.6. Brodsky L. Modern assessment of tonsils and adenoids. Pediatr Clin North Am. 1989; Dec. 36(6):1551–69.
Article7. Josephson GD, Duckworth L, Hossain J. Proposed definitive grading system tool for the assessment of adenoid hyperplasia. Laryngoscope. 2011; Jan. 121(1):187–93.
Article8. Franco RA Jr, Rosenfeld RM, Rao M. First place: resident clinical science award 1999. Quality of life for children with obstructive sleep apnea. Otolaryngol Head Neck Surg. 2000; Jul. 123(1 Pt 1):9–16.9. Kumar DS, Valenzuela D, Kozak FK, Ludemann JP, Moxham JP, Lea J, et al. The reliability of clinical tonsil size grading in children. JAMA Otolaryngol Head Neck Surg. 2014; Nov. 140(11):1034–7.
Article10. Friedman M, Tanyeri H, La Rosa M, Landsberg R, Vaidyanathan K, Pieri S, et al. Clinical predictors of obstructive sleep apnea. Laryngoscope. 1999; Dec. 109(12):1901–7.
Article11. Clemens J, McMurray JS, Willging JP. Electrocautery versus curette adenoidectomy: comparison of postoperative results. Int J Pediatr Otorhinolaryngol. 1998; Mar. 43(2):115–22.
Article12. Fregosi RF, Quan SF, Kaemingk KL, Morgan WJ, Goodwin JL, Cabrera R, et al. Sleep-disordered breathing, pharyngeal size and soft tissue anatomy in children. J Appl Physiol (1985). 2003; Nov. 95(5):2030–8.
Article13. Brodsky L, Adler E, Stanievich JF. Naso- and oropharyngeal dimensions in children with obstructive sleep apnea. Int J Pediatr Otorhinolaryngol. 1989; Feb. 17(1):1–11.
Article14. Arens R, McDonough JM, Corbin AM, Rubin NK, Carroll ME, Pack AI, et al. Upper airway size analysis by magnetic resonance imaging of children with obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2003; Jan. 167(1):65–70.
Article15. Schwab RJ, Pasirstein M, Pierson R, Mackley A, Hachadoorian R, Arens R, et al. Identification of upper airway anatomic risk factors for obstructive sleep apnea with volumetric magnetic resonance imaging. Am J Respir Crit Care Med. 2003; Sep. 168(5):522–30.
Article16. Korhan I, Gode S, Midilli R, Basoglu OK. The influence of the lateral pharyngeal wall anatomy on snoring and sleep apnoea. J Pak Med Assoc. 2015; Feb. 65(2):125–30.17. Tauman R, Gulliver TE, Krishna J, Montgomery-Downs HE, O’Brien LM, Ivanenko A, et al. Persistence of obstructive sleep apnea syndrome in children after adenotonsillectomy. J Pediatr. 2006; Dec. 149(6):803–8.
Article18. Ye J, Liu H, Zhang GH, Li P, Yang QT, Liu X, et al. Outcome of adenotonsillectomy for obstructive sleep apnea syndrome in children. Ann Otol Rhinol Laryngol. 2010; Aug. 119(8):506–13.
Article19. Tagaya M, Nakata S, Yasuma F, Mitchell RB, Sasaki F, Miyazaki S, et al. Children with severe or moderate obstructive sleep apnoea syndrome show a high incidence of persistence after adenotonsillectomy. Acta Otolaryngol. 2012; Nov. 132(11):1208–14.
Article20. Shintani T, Asakura K, Kataura A. The effect of adenotonsillectomy in children with OSA. Int J Pediatr Otorhinolaryngol. 1998; Jun. 44(1):51–8.
Article21. Abdel-Aziz M, Ibrahim N, Ahmed A, El-Hamamsy M, Abdel-Khalik MI, El-Hoshy H. Lingual tonsils hypertrophy; a cause of obstructive sleep apnea in children after adenotonsillectomy: operative problems and management. Int J Pediatr Otorhinolaryngol. 2011; Sep. 75(9):1127–31.
Article22. Schwengel DA, Sterni LM, Tunkel DE, Heitmiller ES. Perioperative management of children with obstructive sleep apnea. Anesth Analg. 2009; Jul. 109(1):60–75.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship between Upper Airway and Sleep-Disordered Breathing in Children with Mouth Breathing
- Sleep-disordered breathing in children
- Allergic Rhinitis and Sleep-disordered Breathing
- Diagnosis and Effect of Maxillary Expansion in Pediatric Sleep-Disordered Breathing
- Associations among High Risk for Sleep-disordered Breathing, Related Risk Factors, and Attention Deficit/Hyperactivity Symptoms in Elementary School Children