Clin Exp Otorhinolaryngol.
2019 Nov;12(4):385-391. 10.21053/ceo.2018.01900.
Management of Acquired Cholesteatoma Associated With Patulous Eustachian Tube and Habitual Sniffing
- Affiliations
-
- 1Department of Otorhinolaryngology and Biomedical Research Institute, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea. entkong@gmail.com
- KMID: 2462734
- DOI: http://doi.org/10.21053/ceo.2018.01900
Abstract
OBJECTIVES
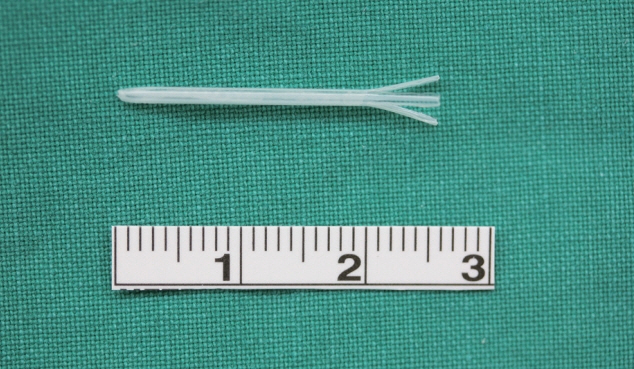
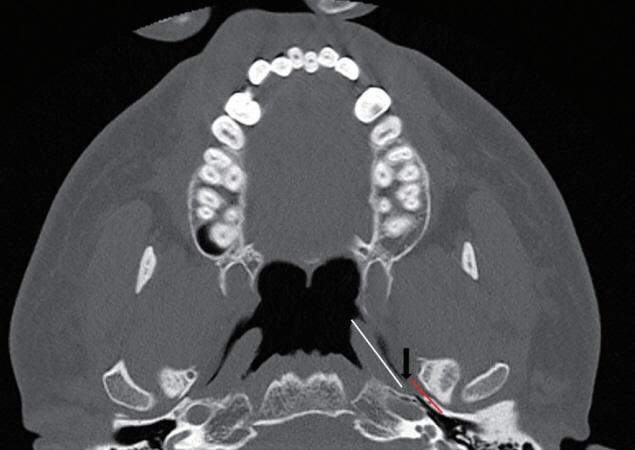
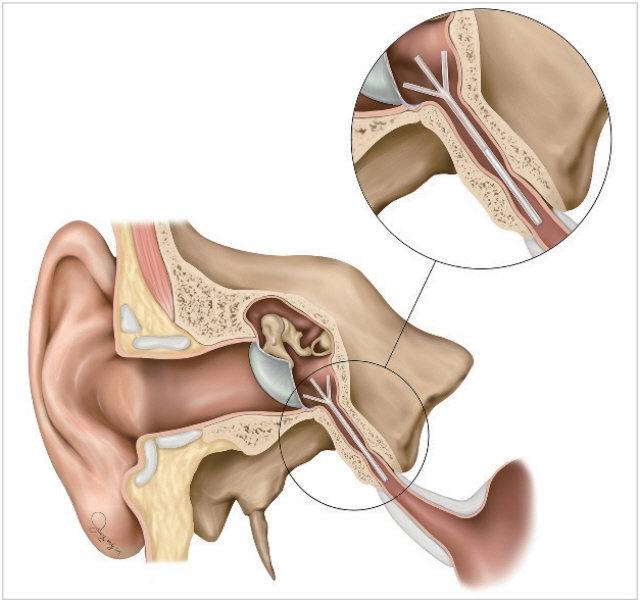
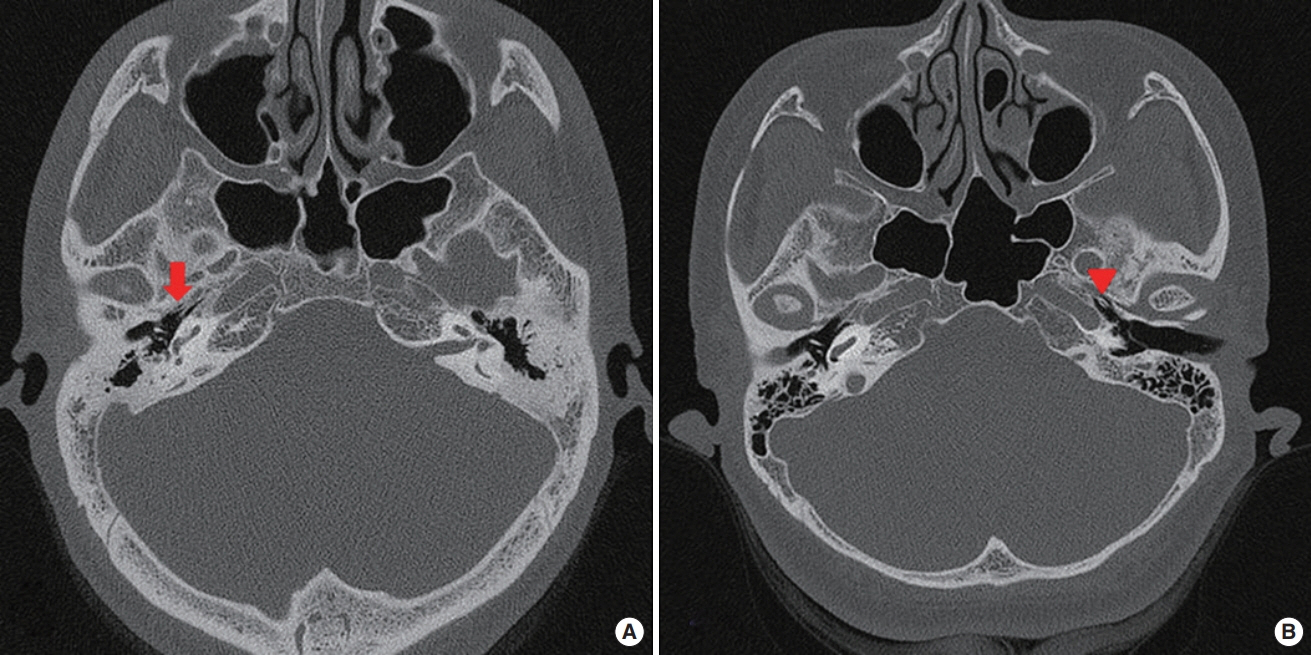
To investigate the effect of surgical treatment with eustachian tube (ET) catheter insertion in patients with acquired cholesteatoma associated with patulous eustachian tube (PET) and habitual sniffing.
METHODS
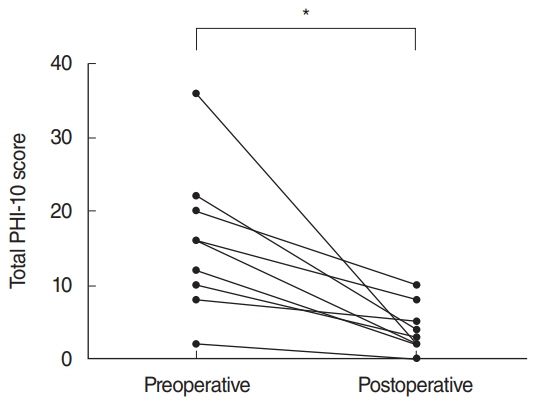
Nine ears of nine patients (two men and seven women; age, 20 to 65 years; average, 37.9±12.0 years) of acquired cholesteatoma associated with PET and habitual sniffing who underwent cholesteatoma surgery with simultaneous additional ET catheter insertion were examined in this study. Successful treatment was defined as stoppage of sniffing, a relief of a PET handicap inventory-10 (PHI-10), an improvement of autophony grade and no cholesteatoma recurrence.
RESULTS
ET catheter insertion was performed in all ears. Follow-up duration ranged from 16 to 37 months (average, 25.4 months). Cases consisted of nine pars flaccida type (100%). All patients obtained relief from aural symptoms and stopped sniffing. Postoperative PHI-10 scores were significantly lower than preoperative scores (P<0.001). During an average follow-up of 25.4 months, no cholesteatoma recurrence has occurred to date. One patient developed otitis media with effusion (OME) post-catheterization; OME resolved spontaneously without treatment. Four patients had a consecutive ET catheter insertion on the other side to resolve PET-related aural symptoms.
CONCLUSION
In case of acquired cholesteatoma with PET and habitual sniffing, ET catheter insertion performed simultaneously with cholesteatoma surgery could help reduce aural symptoms and stop sniffing. Moreover, the procedure might help in preventing cholesteatoma recurrence.
MeSH Terms
Figure
Reference
-
1. Ikeda R, Oshima T, Oshima H, Miyazaki M, Kikuchi T, Kawase T, et al. Management of patulous eustachian tube with habitual sniffing. Otol Neurotol. 2011; Jul. 32(5):790–3.
Article2. Magnuson B. Tubal closing failure in retraction type cholesteatoma and adhesive middle ear lesions. Acta Otolaryngol. 1978; Nov-Dec. 86(5-6):408–17.
Article3. Magnuson B. On the origin of the high negative pressure in the middle ear space. Am J Otolaryngol. 1981; Feb. 2(1):1–12.
Article4. Magnuson B. Tympanoplasty and recurrent disease: sniff-induced high negative pressure in the middle ear space. Am J Otolaryngol. 1981; Nov. 2(4):277–83.
Article5. Falk B, Magnuson B. Evacuation of the middle ear by sniffing: a cause of high negative pressure and development of middle ear disease. Otolaryngol Head Neck Surg. 1984; Jun. 92(3):312–8.
Article6. Falk B. Sniff-induced negative middle ear pressure: study of a consecutive series of children with otitis media with effusion. Am J Otolaryngol. 1982; May-Jun. 3(3):155–62.
Article7. Kobayashi T, Takasaka T. Voluntarily retractable tympanic membranes: case report. Am J Otol. 1991; May. 12(3):215–7.8. Yaginuma Y, Kobayashi T, Takasaka T. The habit of sniffing in nasal diseases as a cause of secretory otitis media. Am J Otol. 1996; Jan. 17(1):108–10.9. Kobayashi T, Yaginuma Y, Takahashi Y, Takasaka T. Incidence of sniffrelated cholesteatomas. Acta Otolaryngol. 1996; Jan. 116(1):74–6.
Article10. Ohta S, Sakagami M, Suzuki M, Mishiro Y. Eustachian tube function and habitual sniffing in middle ear cholesteatoma. Otol Neurotol. 2009; Jan. 30(1):48–53.
Article11. Asawapittayanont P, Ikeda R, Oshima H, Kikuchi T, Miyazaki H, Kawase T, et al. Tubal function tests with optional myringotomy detect eustachian tube closing failure in acquired pars flaccida retraction cholesteatoma. Auris Nasus Larynx. 2017; Feb. 44(1):65–9.
Article12. Tsuji K, Sone M, Kakibuchi M, Sakagami M. Bilateral cholesteatoma and habitual sniffing. Auris Nasus Larynx. 2002; Apr. 29(2):111–4.
Article13. Oh SJ, Lee IW, Goh EK, Kong SK. Trans-tympanic catheter insertion for treatment of patulous eustachian tube. Am J Otolaryngol. 2015; Nov-Dec. 36(6):748–52.
Article14. Sato T, Kawase T, Yano H, Suetake M, Kobayashi T. Trans-tympanic silicone plug insertion for chronic patulous eustachian tube. Acta Otolaryngol. 2005; Nov. 125(11):1158–63.
Article15. Kikuchi T, Ikeda R, Oshima H, Takata I, Kawase T, Oshima T, et al. Effectiveness of Kobayashi plug for 252 ears with chronic patulous eustachian tube. Acta Otolaryngol. 2017; Mar. 137:253–8.
Article16. Ikeda R, Kikuchi T, Oshima H, Miyazaki H, Hidaka H, Kawase T, et al. Relationship between clinical test results and morphologic severity demonstrated by sitting 3-D CT in patients with patulous eustachian tube. Otol Neurotol. 2016; Aug. 37(7):908–13.
Article17. Kobayashi T, Morita M, Yoshioka S, Mizuta K, Ohta S, Kikuchi T, et al. Diagnostic criteria for patulous eustachian tube: a proposal by the Japan Otological Society. Auris Nasus Larynx. 2018; Feb. 45(1):1–5.
Article18. Poe DS. Diagnosis and management of the patulous eustachian tube. Otol Neurotol. 2007; Aug. 28(5):668–77.
Article19. Ikeda R, Kikuchi T, Oshima H, Miyazaki H, Hidaka H, Kawase T, et al. New scoring system for evaluating patulous eustachian tube patients. Otol Neurotol. 2017; Jun. 38(5):708–13.
Article20. Tarabichi M, Najmi M. Visualization of the eustachian tube lumen with Valsalva computed tomography. Laryngoscope. 2015; Mar. 125(3):724–9.
Article21. Harris AT, Mettias B, Lesser TH. Pooled analysis of the evidence for open cavity, combined approach and reconstruction of the mastoid cavity in primary cholesteatoma surgery. J Laryngol Otol. 2016; Mar. 130(3):235–41.
Article22. Kawase T, Yuasa Y, Oshima T, Kobayashi T. Habitual sniffing and postoperative configuration of the posterior meatal wall reconstructed with soft tissue. Acta Otolaryngol. 2007; Nov. 127(11):1132–5.
Article23. Yamamoto-Fukuda T, Takasaki K, Takahashi H. Effect of the tympanostomy tube on postoperative retraction of the soft posterior meatal wall caused by habitual sniffing. Laryngoscope. 2009; Oct. 119(10):2037–41.
Article24. Hasegawa J, Kawase T, Yuasa Y, Hori Y, Sato T, Kobayashi T. Effects of hearing level on habitual sniffing in patients with cholesteatoma. Acta Otolaryngol. 2006; Jun. 126(6):577–80.
Article25. Kobayashi T, Hasegawa J, Kikuchi T, Suzuki T, Oshima T, Kawase T. Masked patulous eustachian tube: an important diagnostic precaution before middle ear surgery. Tohoku J Exp Med. 2009; Aug. 218(4):317–24.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Free Fat Autograft with Topical Anticholinergic for Patulous Eustachian Tube
- Therapeutic Efficacy of Angiocatheter Insertion Surgery in the Bony Orifice of Patulous Eustachian Tube
- Two Cases of Free Fat Graft at Patulous Eustachian Tube
- A Case of Collagen Graft for Patulous Eustachian Tube
- Objective Tinnitus