Clin Orthop Surg.
2019 Sep;11(3):325-331. 10.4055/cios.2019.11.3.325.
The Innervated Distally Based First Dorsal Metatarsal Artery Flap with a Wide Pedicle for Reconstruction of a Great Toe Defect
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul National University Hospital, Seoul, Korea. orthoyhl@snu.ac.kr
- KMID: 2462562
- DOI: http://doi.org/10.4055/cios.2019.11.3.325
Abstract
- BACKGROUND
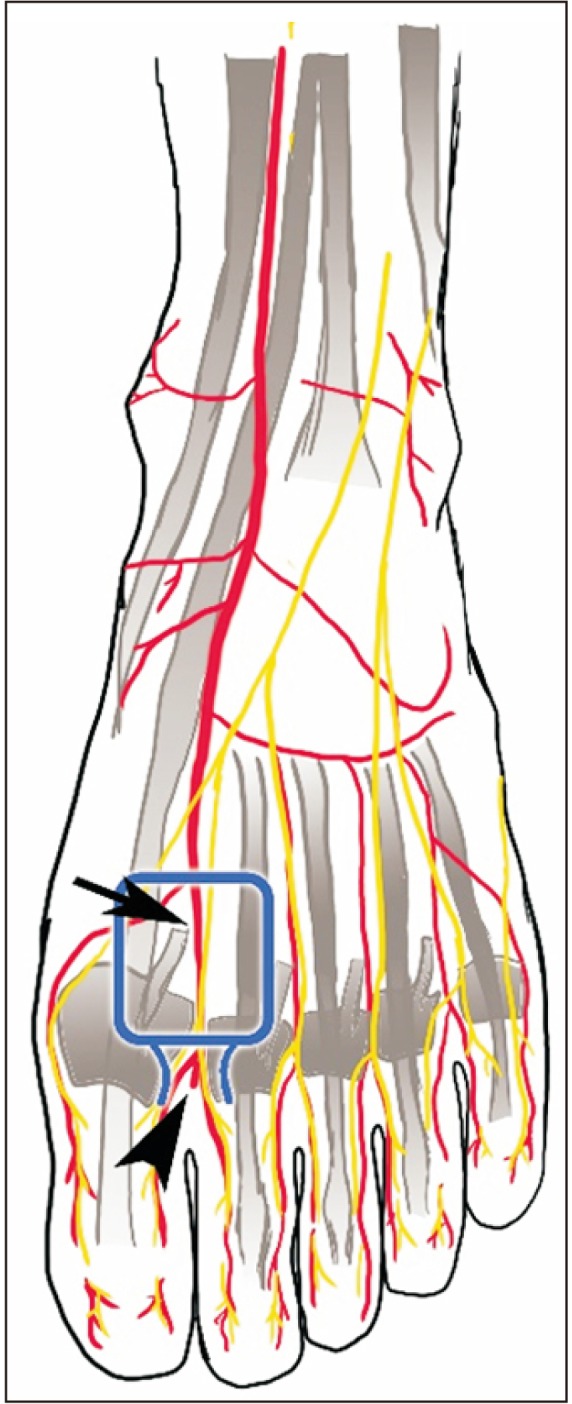
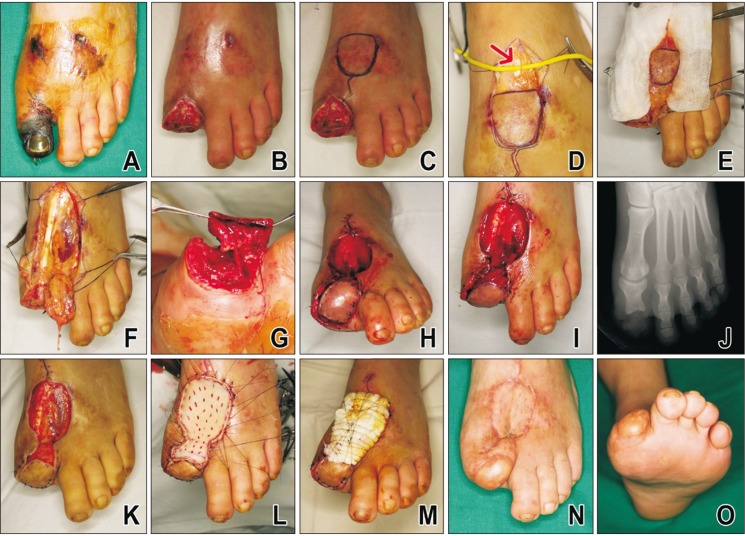
It is difficult for surgeons to reconstruct soft tissue defects of the great toe. This report aims to evaluate the utility and efficacy of innervated distally based first dorsal metatarsal artery (FDMA) flap with a wide pedicle for reconstruction of soft tissue defects of the great toe.
METHODS
This is a retrospective report. Between January 2015 and December 2017, six cases of skin defect of the great toe were reconstructed with an innervated distally based FDMA flap with a wide pedicle. One case was excluded in this report because of chronic pain on the metatarsophalangeal joint due to osteoarthritis before the injury. A total of five cases were evaluated for flap survival and sensory recovery. The sensory recovery was investigated by two-point discrimination and Semmes-Weinstein monofilament tests. The average age of the selected patients was 40 years (range, 36 to 56 years), and the average size of the defect in the toe was 8.3 cm2 (range, 4 to 13.8 cm2). The average follow-up period was 29.4 months (range, 18 to 38 months).
RESULTS
All patients survived without any complications. The average two-point discrimination test value was 8.0 ± 0.89 mm (range, 7 to 9 mm), and the average value obtained from the Semmes-Weinstein monofilament test was 4.53 ± 0.33 (range, 4.17 to 4.93). The average residual pain score evaluated with a visual analog scale was 1 (range, 0 to 2). Two patients complained of stiffness in the great toe below 30° of total range of motion during the early stages after surgery, but this stiffness gradually improved after rehabilitation. The average range of motion of three patients with a remaining metatarsophalangeal joint after surgery was 80° (range, 70° to 90°). All five cases could walk regularly without any unique footwear at the final follow-up.
CONCLUSIONS
The innervated distally based FDMA flap with a wide pedicle could be a good alternative method for repair of soft tissue defects of the great toe.
MeSH Terms
Figure
Cited by 1 articles
-
당뇨발 절단 치료에서 Fillet Flap의 사용
Jung Woo Lee, Hwan Ryu, Jae Yong Park
J Korean Foot Ankle Soc. 2020;24(4):148-155. doi: 10.14193/jkfas.2020.24.4.148.
Reference
-
1. Hughes J, Clark P, Klenerman L. The importance of the toes in walking. J Bone Joint Surg Br. 1990; 72(2):245–251. PMID: 2312564.
Article2. Quebedeaux TL, Lavery LA, Lavery DC. The development of foot deformities and ulcers after great toe amputation in diabetes. Diabetes Care. 1996; 19(2):165–167. PMID: 8718439.
Article3. Limthongthang R, Eamsobhana P. First dorsal metatarsal artery perforator flap to cover great toe defect. J Orthop Surg (Hong Kong). 2017; 25(3):2309499017739497. PMID: 29137568.
Article4. Reiffel RS, McCarthy JG. Coverage of heel and sole defects: a new subfascial arterialized flap. Plast Reconstr Surg. 1980; 66(2):250–260. PMID: 6996010.5. McCraw JB, Furlow LT Jr. The dorsalis pedis arterialized flap: a clinical study. Plast Reconstr Surg. 1975; 55(2):177–185. PMID: 1090947.6. Ishikawa K, Isshiki N, Suzuki S, Shimamura S. Distally based dorsalis pedis island flap for coverage of the distal portion of the foot. Br J Plast Surg. 1987; 40(5):521–525. PMID: 3676584.
Article7. Bharathwaj VS, Quaba AA. The distally based islanded dorsal foot flap. Br J Plast Surg. 1997; 50(4):284–287. PMID: 9215073.
Article8. Governa M, Barisoni D. Distally based dorsalis pedis island flap for a distal lateral electric burn of the big toe. Burns. 1996; 22(8):641–643. PMID: 8982547.
Article9. Russo A, Delia G, Casoli V, Colonna MR, Stagno d'Alcontres F. Dorsalis Pedis Adipofascial Perforator flap for great toe reconstruction: anatomical study and clinical applications. J Plast Reconstr Aesthet Surg. 2014; 67(4):550–554. PMID: 24513560.
Article10. Earley MJ, Milner RH. A distally based first web flap in the foot. Br J Plast Surg. 1989; 42(5):507–511. PMID: 2804512.
Article11. Kim JW, Choi YJ, Lee HJ, Yi KH, Kim HJ, Hu KS. Anatomic study of the dorsalis pedis artery, first metatarsal artery, and second metatarsal bone for mandibular reconstruction. J Oral Maxillofac Surg. 2015; 73(8):1627–1636. PMID: 25930957.
Article12. van Alphen NA, Laungani AT, Christner JA, Lachman N, Carlsen BT, Saint-Cyr M. The distally based dorsal metatarsal artery perforator flap: vascular study and clinical implications. J Reconstr Microsurg. 2016; 32(4):245–250. PMID: 26165886.
Article13. Fares A, Kusnezov N, Dunn JC, et al. Predictability of lower extremity peripheral nervous anatomy. J Surg Orthop Adv. 2017; 26(4):206–210. PMID: 29461191.14. Candan B, Albay S. Determination and classification of cutaneous innervation of the dorsum of the foot in foetal cadavers. Folia Morphol (Warsz). 2018; 77(4):698–702. PMID: 29500895.15. Wahee P, Aggarwal A, Harjeet , Sahni D. Variable patterns of cutaneous innervation on the dorsum of foot in fetuses. Surg Radiol Anat. 2010; 32(5):469–475. PMID: 19911110.
Article16. Josty IC, Ramaswamy R, Laing JH. Vaccum assisted closure: an alternative strategy in the management of degloving injuries of the foot. Br J Plast Surg. 2001; 54(4):363–365. PMID: 11355997.
Article17. Aerden D, Vanmierlo B, Denecker N, Brasseur L, Keymeulen B, Van den Brande P. Primary closure with a filleted hallux flap after transmetatarsal amputation of the big toe for osteomyelitis in the diabetic foot: a short series of four cases. Int J Low Extrem Wounds. 2012; 11(2):80–84. PMID: 22561521.18. Downs DM, Jacobs RL. Treatment of resistant ulcers on the plantar surface of the great toe in diabetics. J Bone Joint Surg Am. 1982; 64(6):930–933. PMID: 7045132.
Article19. Akita S, Mitsukawa N, Rikihisa N, et al. Reconstruction of the great toe using a pedicled medial plantar flap with anterograde venous drainage. Microsurgery. 2014; 34(5):398–403. PMID: 24510392.
Article20. Dong JS, Peng YP, Zhang YX, Lim BH, Pho RW. Reverse anterior tibial artery flap for reconstruction of foot donor site. Plast Reconstr Surg. 2003; 112(6):1604–1612. PMID: 14578791.
Article21. Sidon E, Shemesh S, Rosenthal Y, Heller S, Velkes S, Burg A. Medial forefoot fillet flap for primary closure of transmetatarsal amputation: a series of four cases. Foot (Edinb). 2017; 33:53–56. PMID: 29126044.
Article22. Lee JH, Dauber W. Anatomic study of the dorsalis pedis-first dorsal metatarsal artery. Ann Plast Surg. 1997; 38(1):50–55. PMID: 9015540.
Article23. Kawamura K, Yajima H, Kobata Y, Shigematsu K, Maegawa N, Takakura Y. Coverage of big toe defects after wrap-around flap transfer with a free soleus perforator flap. J Reconstr Microsurg. 2005; 21(4):225–229. PMID: 15971138.
Article24. Kim YH, Kim KH, Sung KY, Kim JT, Kim SW. Toe resurfacing with a thin thoracodorsal artery perforator flap. Microsurgery. 2017; 37(4):312–318. PMID: 26612346.
Article25. Myerson M. Split-thickness skin excision: its use for immediate wound care in crush injuries of the foot. Foot Ankle. 1989; 10(2):54–60. PMID: 2572522.
Article26. Attinger C. Use of skin grafting in the foot. J Am Podiatr Med Assoc. 1995; 85(1):49–56. PMID: 7861325.
Article27. Attinger C. Soft-tissue coverage for lower-extremity trauma. Orthop Clin North Am. 1995; 26(2):295–334. PMID: 7724195.
Article28. Kuntscher MV, Erdmann D, Homann HH, Steinau HU, Levin SL, Germann G. The concept of fillet flaps: classification, indications, and analysis of their clinical value. Plast Reconstr Surg. 2001; 108(4):885–896. PMID: 11547143.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Homodigital Reverse Pedicle Island Flap for Reconstruction of the Great Toe: A Case Report
- Neurovascular Free Toe Pulp Flap Using Dorsal Digital Artery In Finger Reconstruction
- Reconstruction of Foot and Ankle Soft Tissue Defecty by Lateral Supramalleolar Flap
- Reconstruction of Soft Tissue Defect of the Finger with Second Dorsal Metatarsal Arterial Flap
- Proximal Tibia Opening Wedge Osteotomy for Treatment of Genu Recurvatum after Ipsilateral Femoral Shaft Fracture