Clin Orthop Surg.
2019 Sep;11(3):258-264. 10.4055/cios.2019.11.3.258.
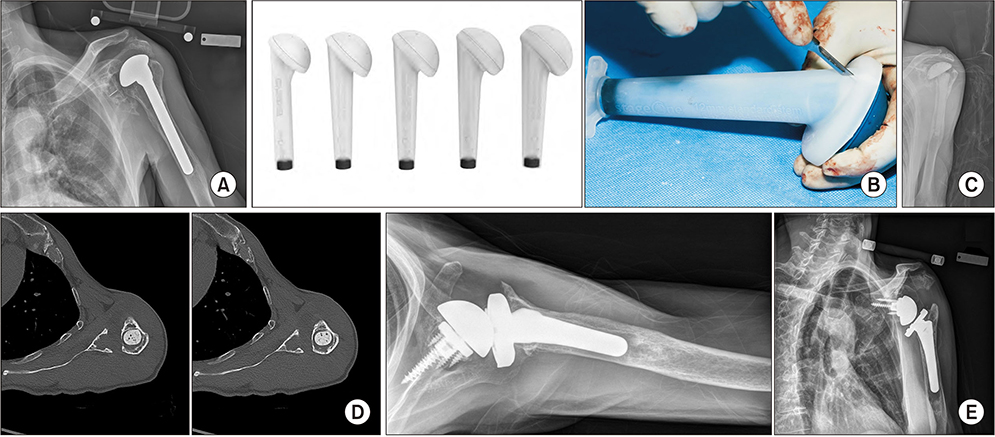
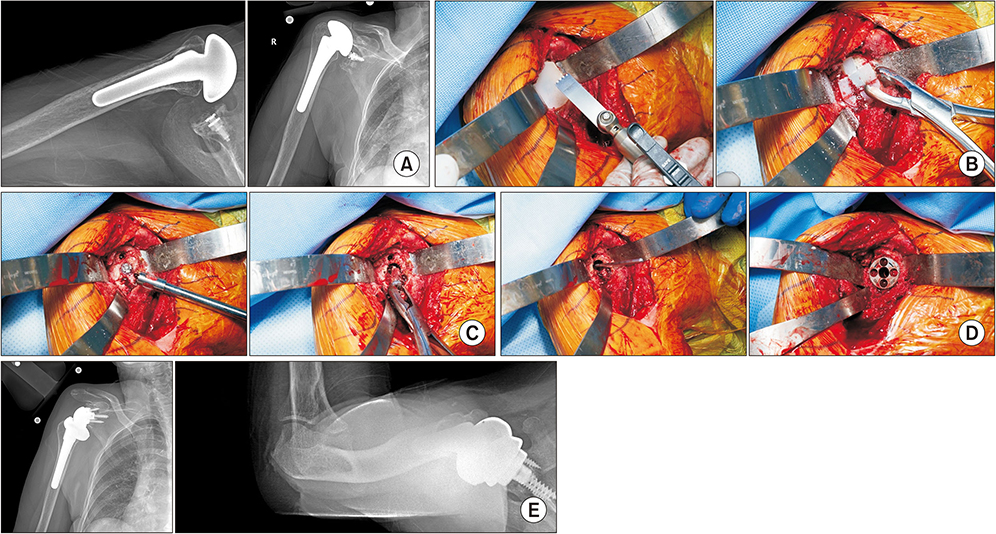
Pearls and Tips in Shoulder Arthroplasty
- Affiliations
-
- 1Department of Orthopedic Surgery, Mayo Clinic, Rochester, MN, USA. sperling.john@mayo.edu
- KMID: 2462552
- DOI: http://doi.org/10.4055/cios.2019.11.3.258
Abstract
- There has been rapid evolution in new techniques and technology in shoulder arthroplasty. This has improved the efficiency of the procedures as well as expanded our ability to manage some of the most challenging cases. This article will review key aspects of patient evaluation, discuss key technical steps in primary anatomic and reverse arthroplasty, and lastly provide tips to facilitate revision surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Amini MH, Ricchetti ET, Iannotti JP. Three-dimensional templating and use of standard instrumentation in primary anatomic total shoulder arthroplasty. JBJS Essent Surg Tech. 2017; 7(3):e28.
Article2. Ricchetti ET, Jun BJ, Cain RA, et al. Sequential 3-dimensional computed tomography analysis of implant position following total shoulder arthroplasty. J Shoulder Elbow Surg. 2018; 27(6):983–992.
Article3. Iannotti JP, Weiner S, Rodriguez E, et al. Three-dimensional imaging and templating improve glenoid implant positioning. J Bone Joint Surg Am. 2015; 97(8):651–658.
Article4. Lapner PL, Wood KS, Zhang T, Athwal GS. The return of subscapularis strength after shoulder arthroplasty. J Shoulder Elbow Surg. 2015; 24(2):223–228.
Article5. Sacevich N, Athwal GS, Lapner P. Subscapularis management in total shoulder arthroplasty. J Hand Surg Am. 2015; 40(5):1009–1011.
Article6. Gutierrez S, Greiwe RM, Frankle MA, Siegal S, Lee WE 3rd. Biomechanical comparison of component position and hardware failure in the reverse shoulder prosthesis. J Shoulder Elbow Surg. 2007; 16:3 Suppl. S9–S12.7. Alentorn-Geli E, Clark NJ, Assenmacher AT, et al. What are the complications, survival, and outcomes after revision to reverse shoulder arthroplasty in patients older than 80 years? Clin Orthop Relat Res. 2017; 475(11):2744–2751.
Article8. Wagner ER, Statz JM, Houdek MT, Cofield RH, Sanchez-Sotelo J, Sperling JW. Use of a shorter humeral stem in revision reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2017; 26(8):1454–1461.
Article9. Wagner ER, Houdek MT, Hernandez NM, Cofield RH, Sanchez-Sotelo J, Sperling JW. Cement-within-cement technique in revision reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2017; 26(8):1448–1453.
Article10. Merolla G, Wagner E, Sperling JW, Paladini P, Fabbri E, Porcellini G. Revision of failed shoulder hemiarthroplasty to reverse total arthroplasty: analysis of 157 revision implants. J Shoulder Elbow Surg. 2018; 27(1):75–81.
Article11. Baghdadi YMK, Maradit-Kremers H, Dennison T, et al. The hospital cost of two-stage reimplantation for deep infection after shoulder arthroplasty. JSES Open Access. 2017; 1(1):15–18.
Article12. Assenmacher AT, Alentorn-Geli E, Dennison T, et al. Two-stage reimplantation for the treatment of deep infection after shoulder arthroplasty. J Shoulder Elbow Surg. 2017; 26(11):1978–1983.
Article13. Hernandez NM, Chalmers BP, Wagner ER, Sperling JW, Cofield RH, Sanchez-Sotelo J. Revision to reverse total shoulder arthroplasty restores stability for patients with unstable shoulder prostheses. Clin Orthop Relat Res. 2017; 475(11):2716–2722.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Isolated Musculocutaneous Nerve Palsy after the Reverse Total Shoulder Arthroplasty
- The Current State of Total Shoulder Arthroplasty
- Reverse Total Shoulder Arthroplasty: Techniques and Pitfalls
- Acromion Fracture after Reverse Total Shoulder Arthroplasty
- The Internal Rotation Deficit in Reverse Shoulder Arthroplasty: Can Humeral Rotation Make Difference?