Healthc Inform Res.
2019 Oct;25(4):313-323. 10.4258/hir.2019.25.4.313.
Follow-Up Decision Support Tool for Public Healthcare: A Design Research Perspective
- Affiliations
-
- 1Victoria University Business School, Victoria University - Footscray Park Campus, Melbourne, Australia. shah.miah@vu.edu.au
- 2Center for Modern Information Management, Huazhong University of Science and Technology, Wuhan, China.
- 3School of Management, Zayed University - Abu Dhabi Campus, Abu Dhabi, UAE.
- KMID: 2462230
- DOI: http://doi.org/10.4258/hir.2019.25.4.313
Abstract
OBJECTIVES
Mobile health (m-Health) technologies may provide an appropriate follow-up support service for patient groups with post-treatment conditions. While previous studies have introduced m-Health methods for patient care, a smart system that may provide follow-up communication and decision support remains limited to the management of a few specific types of diseases. This paper introduces an m-Health solution in the current climate of increased demand for electronic information exchange.
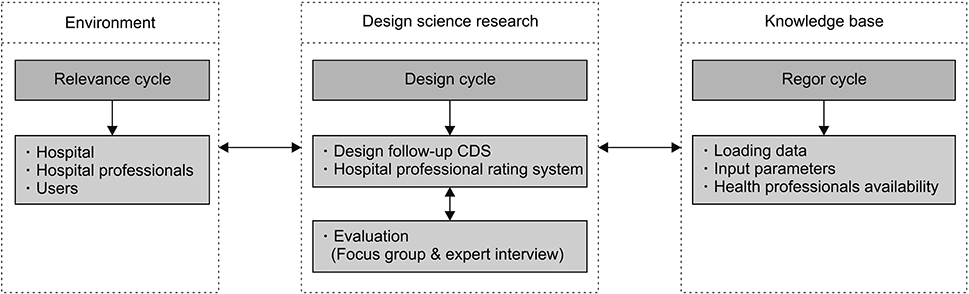
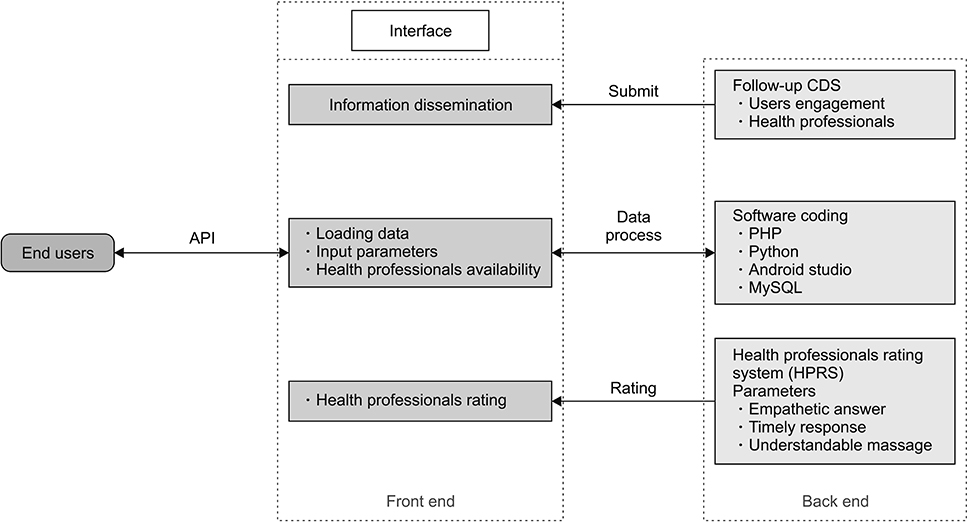
METHODS
Adopting a novel design science research approach, we developed an innovative solution model for post-treatment follow-up decision support interaction for use by patients and physicians and then evaluated it by using convergent interviewing and focus group methods.
RESULTS
The cloud-based solution was positively evaluated as supporting physicians and service providers in providing post-treatment follow-up services. Our framework provides a model as an artifact for extending care service systems to inform better follow-up interaction and decision-making.
CONCLUSIONS
The study confirmed the perceived value and utility of the proposed Clinical Decision Support artifact indicating that it is promising and has potential to contribute and facilitate appropriate interactions and support for healthcare professionals for future follow-up operationalization. While the prototype was developed and tested in a developing country context, where the availability of doctors is limited for public healthcare, it was anticipated that the prototype would be user-friendly, easy to use, and suitable for post-treatment follow-up through mobility in remote locations.
MeSH Terms
Figure
Cited by 2 articles
-
Real-Time Monitoring System to Manage Mental Healthcare Emergency Unit
Samy Housbane, Adil Khoubila, Khaoula Ajbal, Mohamed Agoub, Omar Battas, Mohamed Bennani Othmani
Healthc Inform Res. 2020;26(4):344-350. doi: 10.4258/hir.2020.26.4.344.Dynamic Demand-Centered Process-Oriented Data Model for Inventory Management of Hemovigilance Systems
Mahnaz Sohrabi, Mostafa Zandieh, Behrouz Afshar Nadjafi
Healthc Inform Res. 2021;27(1):73-81. doi: 10.4258/hir.2021.27.1.73.
Reference
-
1. Dugdale DC, Epstein R, Pantilat SZ. Time and the patient-physician relationship. J Gen Intern Med. 1999; 14 Suppl 1:S34–S40.
Article2. Hinton L, Franz CE, Reddy G, Flores Y, Kravitz RL, Barker JC. Practice constraints, behavioral problems, and dementia care: primary care physicians' perspectives. J Gen Intern Med. 2007; 22(11):1487–1492.
Article3. Clarke JL, Bourn S, Skoufalos A, Beck EH, Castillo DJ. An innovative approach to health care delivery for patients with chronic conditions. Popul Health Manag. 2017; 20(1):23–30.
Article4. Qaseem A. High Value Care Task Force of the American College of Physicians. Appropriate use of therapeutic interventions to foster high-value care. Ann Intern Med. 2016; 165(11):831–832.
Article5. Chen HS, Su MJ, Shyu FM, Luh JJ, Hwang SL, Su S, et al. Mobile hospital: healthcare for anybody in anytime and anywhere. In : Proceedings of 7th International Workshop on Enterprise networking and Computing in Healthcare Industry; 2005 Jun 23–25; Busan, Korea. p. 144–149.6. Sadegh SS, Khakshour Saadat P, Sepehri MM, Assadi V. A framework for m-health service development and success evaluation. Int J Med Inform. 2018; 112:123–130.
Article7. Desai D, Upadhyay H. Security and privacy consideration for internet of things in smart home environments. Int J Eng Res Dev. 2014; 10(11):73–83.8. Varshney U. A model for improving quality of decisions in mobile health. Decision Support Systems. 2014; 62:66–77.
Article9. Thomas SK, Coleman JJ. The impact of computerised physician order entry with integrated clinical decision support on pharmacist–physician communication in the hospital setting: a systematic review of the literature. Eur J Hosp Pharm. 2012; 19(4):349–354.
Article10. DeVault D, Artstein R, Benn G, Dey T, Fast E, Gainer A, et al. SimSensei Kiosk: a virtual human interviewer for healthcare decision support. In : Proceedings of the 2014 International Conference on Autonomous Agents and Multi-agent Systems; 2014 May 5–9; Paris, France. p. 1061–1068.11. Abidi SR, Abidi SS, Hussain S, Shepherd M. Ontology-based modeling of clinical practice guidelines: a clinical decision support system for breast cancer follow-up interventions at primary care settings. Stud Health Technol Inform. 2007; 129(Pt 2):845–849.12. Fraser HS, Allen C, Bailey C, Douglas G, Shin S, Blaya J. Information systems for patient follow-up and chronic management of HIV and tuberculosis: a life-saving technology in resource-poor areas. J Med Internet Res. 2007; 9(4):e29.
Article13. Piette JD, Weinberger M, Kraemer FB, McPhee SJ. Impact of automated calls with nurse follow-up on diabetes treatment outcomes in a Department of Veterans Affairs Health Care System: a randomized controlled trial. Diabetes Care. 2001; 24(2):202–208.
Article14. Singh H, Wilson L, Petersen LA, Sawhney MK, Reis B, Espadas D, et al. Improving follow-up of abnormal cancer screens using electronic health records: trust but verify test result communication. BMC Med Inform Decis Mak. 2009; 9:49.
Article15. Green BB, Wang CY, Horner K, Catz S, Meenan RT, Vernon SW, et al. Systems of support to increase colorectal cancer screening and follow-up rates (SOS): design, challenges, and baseline characteristics of trial participants. Contemp Clin Trials. 2010; 31(6):589–603.
Article16. Bjorkhem-Bergman L, Andersen-Karlsson E, Laing R, Diogene E, Melien O, Jirlow M, et al. Interface management of pharmacotherapy: joint hospital and primary care drug recommendations. Eur J Clin Pharmacol. 2013; 69 Suppl 1:73–78.
Article17. Voth EC, Oelke ND, Jung ME. A theory-based exercise app to enhance exercise adherence: a pilot study. JMIR Mhealth Uhealth. 2016; 4(2):e62.
Article18. Lyles CR, Ratanawongsa N, Bolen SD, Samal L. mHealth and health information technology tools for diverse patients with diabetes. J Diabetes Res. 2017; 2017:1704917.
Article19. Mumford E. Effective requirements analysis and systems design: the ETHICS method. Cambridge (MA): MIT Press;1995.20. Carlsson SA. Developing knowledge through IS design science research. Scand J Inf Syst. 2007; 19(2):2.21. Orlikowski WJ, Iacono CS. Desperately seeking the “IT” in IT research: a call to theorizing the IT artifact. Inf Syst Res. 2001; 12(2):121–134.
Article22. Hevner AR, March ST, Park J, Ram S. Design science in information systems research. MIS Q. 2004; 28(1):75–105.
Article23. Gregor S, Jones D. The anatomy of a design theory. J Assoc Inf Syst. 2007; 8(5):312–335.
Article24. Jha AK. Health care providers should publish physician ratings [Internet]. Brighton (MA): Harvard Business Review;2015. cited at 2019 Oct 15. Available from: https://hbr.org/2015/10/health-care-providers-should-publish-physician-ratings.25. California Healthcare Performance Information System [Internet]. [place unknown]: California Healthcare Performance Information System;c2017. cited at 2019 Oct 15. Available from: https://caqualityratings.org/.26. Power DJ. Decision support systems: concepts and resources for managers. Westport (CN): Quorum Books;2002.27. Becker S, Miron-Shatz T, Schumacher N, Krocza J, Diamantidis C, Albrecht UV. mHealth 2.0: experiences, Possibilities, and Perspectives. JMIR Mhealth Uhealth. 2014; 2(2):e24.
Article28. Sigler BE. Investigating the perceptions of care coordinators on using behavior theory-based mobile health technology with medicaid populations: a grounded theory study. JMIR Mhealth Uhealth. 2017; 5(3):e36.
Article29. Kaushal R, Shojania KG, Bates DW. Effects of computerized physician order entry and clinical decision support systems on medication safety: a systematic review. Arch Intern Med. 2003; 163(12):1409–1416.
Article30. Miah SJ, Hasan J, Gammack JG. On-cloud healthcare clinic: an e-health consultancy approach for remote communities in a developing country. Telemat Inform. 2017; 34(1):311–322.
Article31. Miah SJ, Gammack J, Hasan N. Extending the framework for mobile health information systems research: a content analysis. Inf Syst. 2017; 69:1–24.
Article32. Miah SJ, Hasan N, Hasan R, Gammack J. Healthcare support for underserved communities using a mobile social media platform. Inf Syst. 2017; 66:1–12.
Article33. Hu Y, Bai G. A systematic literature review of cloud computing in eHealth. Health Inform. 2014; 3(4):11–20.
Article34. Pries-Heje J, Baskerville R, Venable JR. Strategies for design science research evaluation. In : Proceedings of the European Conference on Information System (ECIS); 2008 Jun 9–11; Galway, Ireland. p. 255–266.35. Venable J, Pries-Heje J, Baskerville R. FEDS: a framework for evaluation in design science research. Eur J Inf Syst. 2016; 25(1):77–89.
Article36. Gregor S, Hevner AR. Positioning and presenting design science research for maximum impact. MIS Q. 2013; 37(2):337–355.
Article37. Jepsen DM, Rodwell JJ. Convergent interviewing: a qualitative diagnostic technique for researchers. Manag Res News. 2008; 31(9):650–658.
Article38. Tremblay MC, Hevner AR, Berndt DJ. Focus groups for artifact refinement and evaluation in design research. Commun Assoc Inf Syst. 2010; 26:599–618.
Article39. Osterle H, Becker J, Frank U, Hess T, Karagiannis D, Krcmar H, et al. Memorandum on design-oriented information systems research. Eur J Inf Syst. 2011; 20(1):7–10.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The future of artificial intelligence for physicians
- Book Review: Healthcare Analytics for Quality and Performance Improvement
- The clinical decision analysis using decision tree
- A Study on Participation in Clinical Decision Making by Home Healthcare Nurses
- A Clinical Decision Support System for Diagnosis of Hearing Loss