Obstet Gynecol Sci.
2019 Nov;62(6):469-473. 10.5468/ogs.2019.62.6.469.
Fetal autonomic malfunction as a marker of fetal distress in growth-restricted fetuses: three case reports
- Affiliations
-
- 1Kharkiv Medical Academy of Postgraduate Education, Kharkiv, Ukraine. igorlakhno71@gmail.com
- 2Biomagnetic Center, Hans Berger Department of Neurology, Jena University Hospital, Friedrich Schiller University, Jena, Germany.
- KMID: 2462126
- DOI: http://doi.org/10.5468/ogs.2019.62.6.469
Abstract
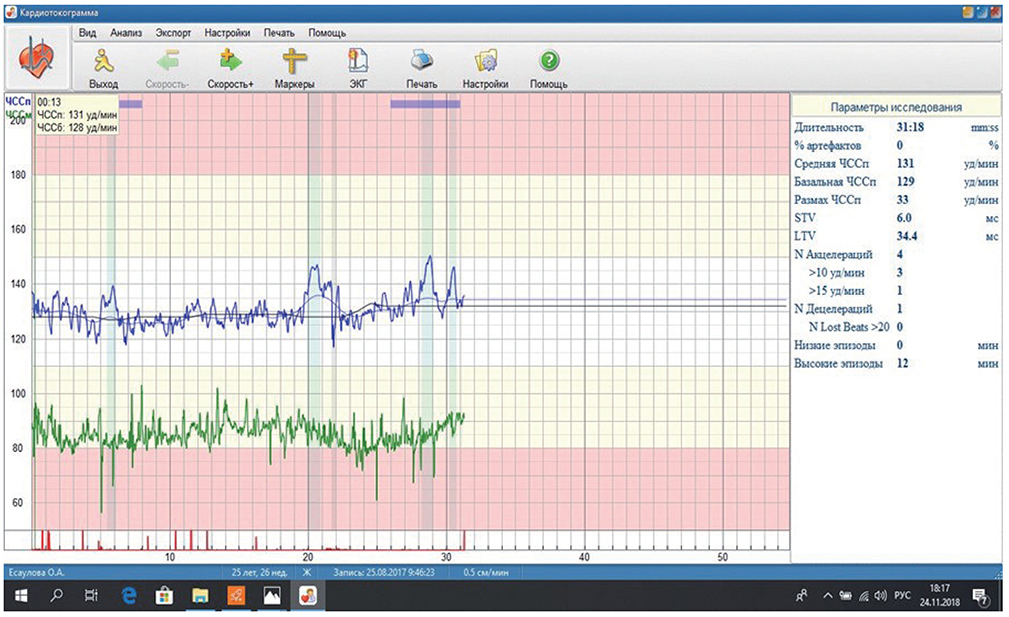
- Fetal growth restriction (FGR) is characterized by fetal compromise and delayed neurological maturation. We report 3 cases of early FGR in the 26th week of gestation, based on hemodynamic Doppler monitoring, conventional cardiotocography, and non-invasive fetal electrocardiography (NI-FECG). Fetal heart rate variability (HRV), beat-to-beat variations, and fetal autonomic brain age scores (fABASs) were normal despite the absence of umbilical diastolic flow in the first case and the pregnancy continued to 30 weeks. NI-FECG helped achieve better fetal maturity. Fetal HRV and fABASs were low in the second and third cases. Fetal demise occurred soon in both cases. We conclude that NI-FECG could be a prospective method for the detection of fetal distress in early FGR.
MeSH Terms
Figure
Cited by 1 articles
-
Fetal programming: could intrauterin life affect health status in adulthood?
Hande Nur Onur Öztürk, Perim Fatma Türker
Obstet Gynecol Sci. 2021;64(6):473-483. doi: 10.5468/ogs.21154.
Reference
-
1. Hoyer D, Żebrowski J, Cysarz D, Gonçalves H, Pytlik A, Amorim-Costa C, et al. Monitoring fetal maturation-objectives, techniques and indices of autonomic function. Physiol Meas. 2017; 38:R61–88.
Article2. Frusca T, Todros T, Lees C, Bilardo CM. TRUFFLE Investigators. Outcome in early-onset fetal growth restriction is best combining computerized fetal heart rate analysis with ductus venosus Doppler: insights from the trial of umbilical and fetal flow in Europe. Am J Obstet Gynecol. 2018; 218:S783–S789.3. Fuchs T. Values of T/QRS ratio in pregnancies complicated by intrauterine growth restriction. J Perinat Med. 2016; 44:751–757.
Article4. Nelson KB, Sartwelle TP, Rouse DJ. Electronic fetal monitoring, cerebral palsy, and caesarean section: assumptions versus evidence. BMJ. 2016; 355:i6405.
Article5. David M, Hirsch M, Karin J, Toledo E, Akselrod S. An estimate of fetal autonomic state by time-frequency analysis of fetal heart rate variability. J Appl Physiol (1985). 2007; 102:1057–1064.
Article6. Fanelli A, Magenes G, Campanile M, Signorini MG. Quantitative assessment of fetal well-being through CTG recordings: a new parameter based on phase-rectified signal average. IEEE J Biomed Health Inform. 2013; 17:959–966.
Article7. Olofsson P, Ayres-de-Campos D, Kessler J, Tendal B, Yli BM, Devoe L. A critical appraisal of the evidence for using cardiotocography plus ECG ST interval analysis for fetal surveillance in labor. Part I: the randomized controlled trials. Acta Obstet Gynecol Scand. 2014; 93:556–568.8. Lakhno I. Fetal non-invasive electrocardiography contributes to better diagnostics of fetal distress: a cross-sectional study among patients with preeclampsia. Ann Acad Med Singapore. 2015; 44:519–523.9. Guzman-Velazquez BP, Lakhno IV, Diaz-Mendez A. In : Arabnia HR, Deligiannidis L, Tinetti FG, Tran QN, editors. HRV descriptors for fetal distress assessment in pregnancy with fetal growth restriction. Proceedings of the 2018 International Conference on Biomedical Engineering & Science BIOENG'18; 2018 Jul 30–Aug 2; Las Vegas, NV. [place unknown]: CSREA Press;2018. p. 13–17.10. Hoyer D, Kowalski EM, Schmidt A, Tetschke F, Nowack S, Rudolph A, et al. Fetal autonomic brain age scores, segmented heart rate variability analysis, and traditional short term variability. Front Hum Neurosci. 2014; 8:948.
Article11. Hoyer D, Tetschke F, Jaekel S, Nowack S, Witte OW, Schleußner E, et al. Fetal functional brain age assessed from universal developmental indices obtained from neuro-vegetative activity patterns. PLoS One. 2013; 8:e74431.
Article12. Behar J, Andreotti F, Zaunseder S, Oster J, Clifford GD. A practical guide to non-invasive foetal electrocardiogram extraction and analysis. Physiol Meas. 2016; 37:R1–R35.
Article13. Reinhard J, Hayes-Gill BR, Yi Q, Hatzmann H, Schiermeier S. Comparison of non-invasive fetal electrocardiogram to Doppler cardiotocogram during the 1st stage of labor. J Perinat Med. 2010; 38:179–185.
Article14. Fuchs T, Grobelak K, Pomorski M, Zimmer M. Fetal heart rate monitoring using maternal abdominal surface electrodes in third trimester: can we obtain additional information other than CTG trace? Adv Clin Exp Med. 2016; 25:309–316.
Article15. Velayo CL, Funamoto K, Silao JNI, Kimura Y, Nicolaides K. Evaluation of abdominal fetal electrocardiography in early intrauterine growth restriction. Front Physiol. 2017; 8:437.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Evaluation and Management of Fetal Growth Restriction
- Renal Artery Pulsatility Index and Renal Volume: Normal Fetuses versus Growth-Retarded Fetuses
- Complete Hydatidiform Mole Coexisting Two Live Fetuses in Triplet Pregnancy
- Approximate Entropy: Analysis of Fetal Heart Rate Variability in Normal and Growth Retarded Fetuses
- The BRCA1 Expression in Placenta of Normal and Fetal Growth Restriction