Pediatr Gastroenterol Hepatol Nutr.
2019 Nov;22(6):588-593. 10.5223/pghn.2019.22.6.588.
Endovascular Closure Resolves Trimethylaminuria Caused by Congenital Portosystemic Shunts
- Affiliations
-
- 1Interventional Radiologist, Hospital General Universitario La Paz, Madrid, Spain. mdponcedorrego@gmail.com
- KMID: 2462100
- DOI: http://doi.org/10.5223/pghn.2019.22.6.588
Abstract
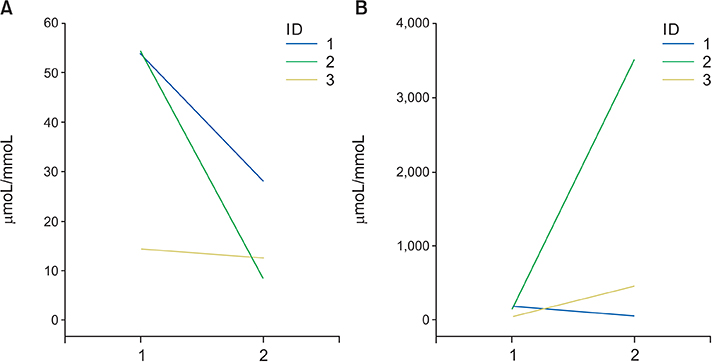
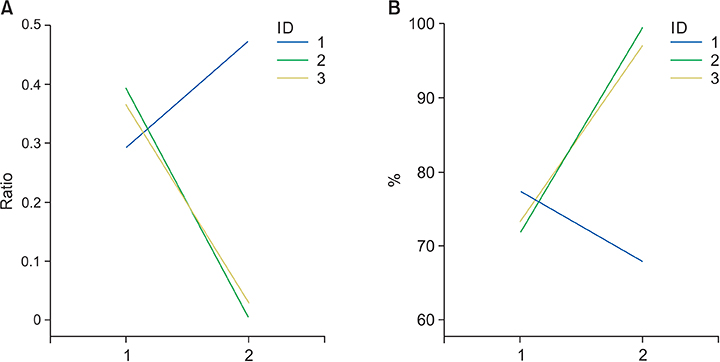
- This study aimed to report three new cases of an association between two rare conditions, congenital portosystemic shunts (CPSS) and trimethylaminuria (TMAU), and the efficacy of endovascular closure of the CPSS for resolving TMAU. Between November 2014 and April 2017, 15 patients with CPSS were enrolled in this prospective study to assess the efficacy of percutaneous endovascular shunt closure. Three patients presented with clinical symptoms of TMAU that were confirmed by urine analysis of trimethylamine (TMA) and TMA n-oxide. One year after endovascular closure of the congenital portosystemic shunt, the same parameters were evaluated were obtained and the values were compared to the pretreatment values. The results indicated the disappearance of clinical symptoms of TMAU and normalization of the urine test parameters in two patients and no changes in one patient, who developed new portosystemic communications.
Figure
Reference
-
1. Wise PM, Eades J, Tjoa S, Fennessey PV, Preti G. Individuals reporting idiopathic malodor production: demographics and incidence of trimethylaminuria. Am J Med. 2011; 124:1058–1063.
Article2. Mackay RJ, McEntyre CJ, Henderson C, Lever M, George PM. Trimethylaminuria: causes and diagnosis of a socially distressing condition. Clin Biochem Rev. 2011; 32:33–43.3. Mountain H, Brisbane JM, Hooper AJ, Burnett JR, Goldblatt J. Trimethylaminuria (fish malodour syndrome): a “benign” genetic condition with major psychosocial sequelae. Med J Aust. 2008; 189:468.
Article4. Messenger J, Clark S, Massick S, Bechtel M. A review of trimethylaminuria: (fish odor syndrome). J Clin Aesthet Dermatol. 2013; 6:45–48.5. Cashman JR. The implications of polymorphisms in mammalian flavin-containing monooxygenases in drug discovery and development. Drug Discov Today. 2004; 9:574–581.
Article6. Mitchell SC, Smith RL. Trimethylaminuria: the fish malodor syndrome. Drug Metab Dispos. 2001; 29(4 Pt 2):517–521.7. Christodoulou J. Trimethylaminuria: an under-recognised and socially debilitating metabolic disorder. J Paediatr Child Health. 2012; 48:E153–E155.
Article8. Ono H, Mawatari H, Mizoguchi N, Eguchi T, Sakura N. Clinical features and outcome of eight infants with intrahepatic porto-venous shunts detected in neonatal screening for galactosaemia. Acta Paediatr. 1998; 87:631–634.
Article9. Gitzelmann R, Forster I, Willi UV. Hypergalactosaemia in a newborn: self-limiting intrahepatic portosystemic venous shunt. Eur J Pediatr. 1997; 156:719–722.
Article10. Kanazawa H, Nosaka S, Miyazaki O, Sakamoto S, Fukuda A, Shigeta T, et al. The classification based on intrahepatic portal system for congenital portosystemic shunts. J Pediatr Surg. 2015; 50:688–695.
Article11. Hao Y, Hong X, Zhao X. Congenital absence of the portal vein associated with focal nodular hyperplasia of the liver and congenital heart disease (Abernethy malformation): a case report and literature review. Oncol Lett. 2015; 9:695–700.
Article12. Lautz TB, Shah SA, Superina RA. Hepatoblastoma in children with congenital portosystemic shunts. J Pediatr Gastroenterol Nutr. 2016; 62:542–545.
Article13. Osorio MJ, Bonow A, Bond GJ, Rivera MR, Vaughan KG, Shah A, et al. Abernethy malformation complicated by hepatopulmonary syndrome and a liver mass successfully treated by liver transplantation. Pediatr Transplant. 2011; 15:E149–E151.
Article14. Sato H, Miura M, Yaoita N, Yamamoto S, Tatebe S, Aoki T, et al. Pulmonary arterial hypertension associated with congenital portosystemic shunts treated with transcatheter embolization and pulmonary vasodilators. Intern Med. 2016; 55:2429–2432.
Article15. Franchi-Abella S, Branchereau S, Lambert V, Fabre M, Steimberg C, Losay J, et al. Complications of congenital portosystemic shunts in children: therapeutic options and outcomes. J Pediatr Gastroenterol Nutr. 2010; 51:322–330.
Article16. Bas S, Guran T, Atay Z, Haliloglu B, Abalı S, Turan S, et al. Premature pubarche, hyperinsulinemia and hypothyroxinemia: novel manifestations of congenital portosystemic shunts (Abernethy malformation) in children. Horm Res Paediatr. 2015; 83:282–287.
Article17. Gong Y, Zhu H, Chen J, Chen Q, Ji M, Pa M, et al. Congenital portosystemic shunts with and without gastrointestinal bleeding - case series. Pediatr Radiol. 2015; 45:1964–1971.
Article18. Schaeffer DF, Laiq S, Jang HJ, John R, Adeyi OA. Abernethy malformation type II with nephrotic syndrome and other multisystemic presentation: an illustrative case for understanding pathogenesis of extrahepatic complication of congenital portosystemic shunt. Hum Pathol. 2013; 44:432–437.
Article19. Bernard O, Franchi-Abella S, Branchereau S, Pariente D, Gauthier F, Jacquemin E. Congenital portosystemic shunts in children: recognition, evaluation, and management. Semin Liver Dis. 2012; 32:273–287.
Article20. Fernández MS, Gutiérrez C, Vila JJ, López A, Ibáñez V, Sangüesa C, et al. Congenital intrahepatic portocaval shunt associated with trimethylaminuria. Pediatr Surg Int. 1997; 12(2-3):196–197.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Treatment of Congenital Portosystemic Shunt: A Single-Center Prospective Study
- Congenital Intrahepatic Portosystemic Shunts
- RE: Endovascular Treatment of Congenital Intrahepatic Portosystemic Shunts with Amplatzer Plugs
- A Clinical Study of Congenital Intrahepatic Portosystemic Shunt Diagnosed in Neonatal Period
- Congenital Intrahepatic Portosystemic Venous Shunt and Liver Mass in a Child Patient: Successful Endovascular Treatment with an Amplatzer Vascular Plug (AVP)