Pediatr Gastroenterol Hepatol Nutr.
2019 Nov;22(6):571-575. 10.5223/pghn.2019.22.6.571.
Anaplastic Large Cell Lymphoma of the Duodenum in a Teenage Girl: Misdiagnosed as an Intramural Duodenal Hematoma
- Affiliations
-
- 1Department of Pediatrics, Ramathibodi Hospital, Faculty of Medicine, Mahidol University, Bangkok, Thailand. pornthep.tan@mahidol.ac.th
- 2Department of Diagnostic and Therapeutic Radiology, Ramathibodi Hospital, Faculty of Medicine, Mahidol University, Bangkok, Thailand.
- 3Division of Pediatric Surgery, Department of Surgery, Ramathibodi Hospital, Faculty of Medicine, Mahidol University, Bangkok, Thailand.
- 4Department of Pediatrics, Faculty of Medicine, Prince of Songkla University, Songkhla, Thailand.
- KMID: 2462097
- DOI: http://doi.org/10.5223/pghn.2019.22.6.571
Abstract
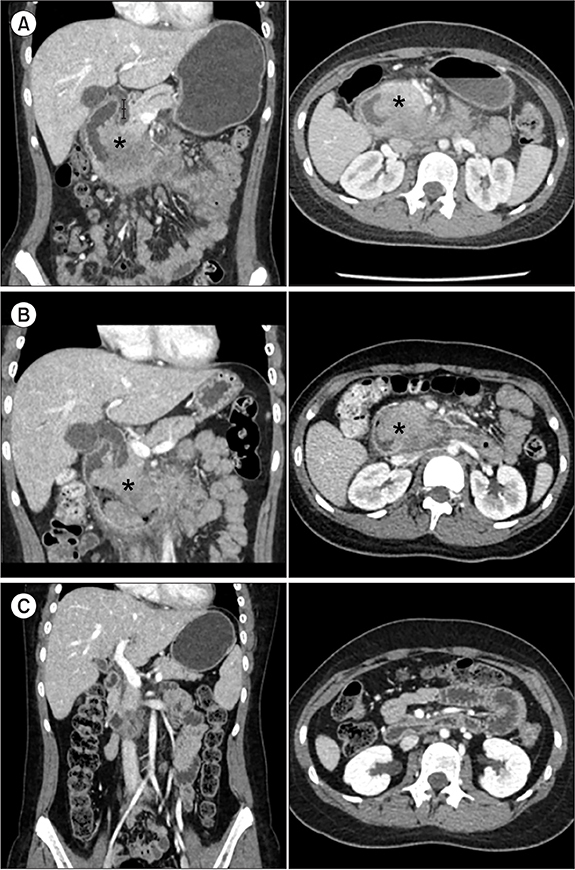
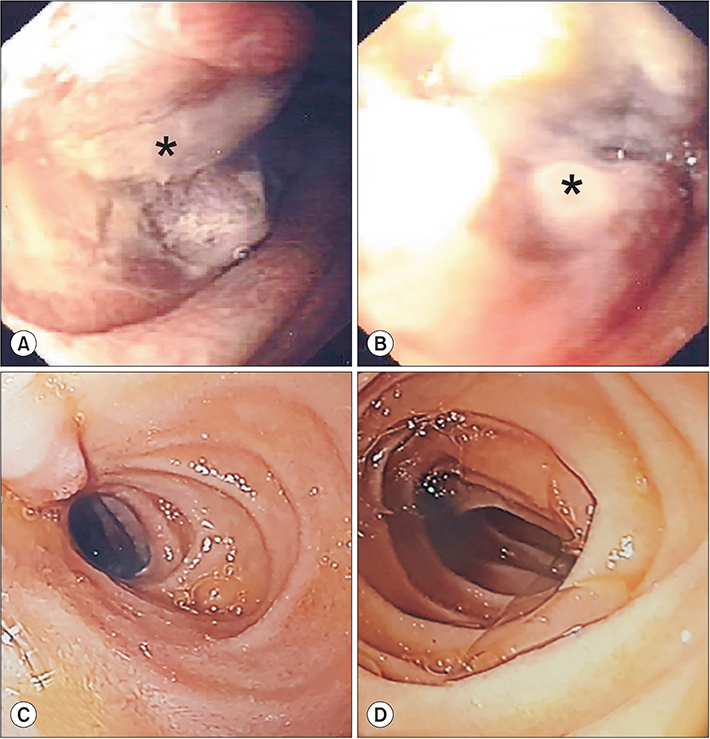
- We report a case of a 13-year-old girl who presented with a 2-month history of intermittent abdominal pain. Laboratory examination showed hepatitis and pancreatitis. Because of persistent vomiting, computed tomography (CT) was performed, which revealed a circumferential soft tissue density in the duodenal wall, causing partial obstruction. Supportive therapy failed. Repeat CT showed no significant change from the initial study. The patient underwent upper endoscopy, which revealed a mass in the second portion of the duodenum, which occluded most parts of the lumen. The histopathological finding was consistent with an anaplastic large cell lymphoma, a rare form of small bowel neoplasm. After the third course of chemotherapy, complete resolution of the mass was noted, and her symptoms were relieved.
Keyword
MeSH Terms
Figure
Reference
-
1. North JH, Pack MS. Malignant tumors of the small intestine: a review of 144 cases. Am Surg. 2000; 66:46–51.2. Farhat MH, Shamseddine AI, Barada KA. Small bowel tumors: clinical presentation, prognosis, and outcome in 33 patients in a tertiary care center. J Oncol. 2008; 2008:212067.
Article3. Ma JK, Ng KK, Poon RT, Fan ST. Pancreatic-induced intramural duodenal haematoma. Asian J Surg. 2008; 31:83–86.
Article4. Fernandes T, Oliveira MI, Castro R, Araújo B, Viamonte B, Cunha R. Bowel wall thickening at CT: simplifying the diagnosis. Insights Imaging. 2014; 5:195–208.
Article5. Ghimire P, Wu GY, Zhu L. Primary gastrointestinal lymphoma. World J Gastroenterol. 2011; 17:697–707.
Article6. Savage KJ, Harris NL, Vose JM, Ullrich F, Jaffe ES, Connors JM, et al. International Peripheral T-Cell Lymphoma Project. ALK- anaplastic large-cell lymphoma is clinically and immunophenotypically different from both ALK+ ALCL and peripheral T-cell lymphoma, not otherwise specified: report from the International Peripheral T-Cell Lymphoma Project. Blood. 2008; 111:5496–5504.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intramural Hematoma of the Duodenum following Endoscopic Biopsy in a Child with Henoch-Schonlein Purpura
- Delayed manifestation of Isolated Intramural Hematoma of the duodenum resulting from Blunt abdominal Trauma
- Successful Endoscopic Decompression for Intramural Duodenal Hematoma with Gastric Outlet Obstruction Complicating Acute Pancreatitis
- Dermatofibroma in Patient with Relapsing Primary Cutaneous Anaplastic Large Cell Lymphoma
- Intramural Duodenal Hematoma following Endoscopic Epinephrine and Thrombin Injection for Bleeding Duodenal Ulcer in a Geriatric Patient with a History of Anticoagulant Drug Use