J Dent Anesth Pain Med.
2019 Oct;19(5):277-288. 10.17245/jdapm.2019.19.5.277.
Comparative evaluation of virtual reality distraction and counter-stimulation on dental anxiety and pain perception in children
- Affiliations
-
- 1Department of Paedodontics and Preventive Dentistry, Narayana Dental College, Nellore, India. drmallineni@gmail.com
- 2Department of Paedodontics and Preventive Dentistry, Priyadarshini Dental College and Hospital, Thiruvallur, India.
- 3Pediatric Dentistry, Preventive Dental Science, College of Dentistry, Majmaah University, Kingdom of Saudi Arabia.
- KMID: 2461244
- DOI: http://doi.org/10.17245/jdapm.2019.19.5.277
Abstract
- BACKGROUND
This study evaluated the efficacy of virtual reality (VR) distraction and counter-stimulation (CS) on dental anxiety and pain perception to local anesthesia in children.
METHODS
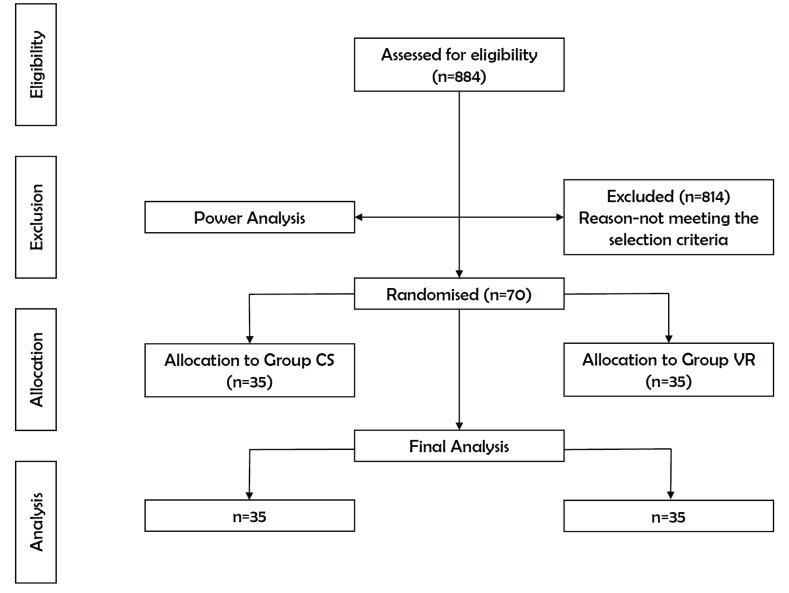
A prospective, randomized, single-blinded interventional clinical trial with a parallel design was used. Seventy children 7-11 years old who required local anesthesia (LA) for pulp therapy or tooth extraction were recruited and allocated to two groups with equal distribution based on the intervention. Group CS (n = 35) received CS and Group VR (n = 35) received VR distraction with ANTVR glasses. Anxiety levels (using pulse rate) were evaluated before, during, and after administration of local anesthesia, while pain perception was assessed immediately after the injection. Wong-Baker faces pain-rating scale (WBFPS), visual analog scale (VAS), and Venham's clinical anxiety rating scale (VCARS) were used for pain evaluation. Student's t-test was used to test the mean difference between groups, and repeated measures ANOVA was used to test the mean difference of pulse rates.
RESULTS
Significant differences in mean pulse rates were observed in both groups, while children in the VR group had a higher reduction (P < 0.05), and the mean VCARS scores were significant in the VR group (P < 0.05). Mean WBFPS scores showed less pain perception to LA needle prick in the CS group while the same change was observed in the VR group with VAS scores.
CONCLUSIONS
VR distraction is better than CS for reducing anxiety to injection in children undergoing extraction and pulpectomy.
MeSH Terms
Figure
Cited by 1 articles
-
Comparative evaluation of the effectiveness of a mobile app (Little Lovely Dentist) and the tell-show-do technique in the management of dental anxiety and fear: a randomized controlled trial
Sainath Reddy Elicherla, Sujatha Bandi, Sivakumar Nuvvula, Rama subbareddy Challa, Kanamarlapudi Venkata Saikiran, Vaka Jeevan Priyanka
J Dent Anesth Pain Med. 2019;19(6):369-378. doi: 10.17245/jdapm.2019.19.6.369.
Reference
-
1. Pain terms: a list with definitions and notes on usage: Recommended by IASP subcommittee on Taxonomy. Pain. 1979; 6:249. PMID: 460932.2. Nomura LH, Bastos JL, Peres MA. Dental pain prevalence and association with dental caries and socioeconomic status in school-children, Southern Brazil, 2002. Braz Oral Res. 2004; 18:134–140. PMID: 15311316.
Article3. Bedi R, Sutcliffe P, Donnan PT, McConnachie J. The prevalence of dental anxiety in a group of 13- and 14-year-old Scottish children. Int J Paediatr Dent. 1992; 2:17–24. PMID: 1525127.
Article4. Klingberg G, Broberg AG. Dental fear/anxiety and dental behaviour management problems in children and adolescents: a review of prevalence and concomitant psychological factors. Int J Paediatr Dent. 2007; 17:391–406. PMID: 17935593.
Article5. Kaur R, Jindal R, Dua R, Mahajan S, Sethi K, Garg S. Comparative evaluation of the effectiveness of audio and audiovisual distraction aids in the management of anxious pediatric dental patients. J Indian Soc Pedod Prev Dent. 2015; 33:192–203. PMID: 26156272.
Article6. Folayan MO, Fatusi A. Effect of psychological management techniques on specific item score change during the management of dental fear in children. J Clin Pediatr Dent. 2005; 29:335–340. PMID: 16161400.
Article7. Corah NL, Gale EN, Illig SJ. Psychological stress reduction during dental procedures. J Dent Res. 1979; 58:1347–1351. PMID: 372266.
Article8. Agarwal M, Das UM. Dental anxiety prediction using Venham Picture test: A preliminary cross- sectional study. J Indian Soc Pedod Prev Dent. 2013; 31:22–24. PMID: 23727738.9. Agras S, Sylvester D, Oliveau D. The epidemiology of common fears and phobia. Compr Psychiatry. 1969; 10:151–156. PMID: 5774552.
Article10. Rachman S. The conditioning theory of fear acquisition: a critical examination. Behav Res Ther. 1977; 15:375–387. PMID: 612338.11. Carrillo-Diaz M, Crego A, Armfield JM, Romero-Maroto M. Assessing the relative efficacy of cognitive and non-cognitive factors as predictors of dental anxiety. Eur J Oral Sci. 2012; 120:82–88. PMID: 22288925.
Article12. Hmud R, Walsh LJ. Dental anxiety: causes, complications and management approaches. J Minim Interv Dent. 2009; 2:67–78.13. Kent G. Cognitive processes in dental anxiety. Br J Clin Psychol. 1985; 24:259–264. PMID: 4074986.
Article14. Allen KD, Stanley RT, McPherson K. Evaluation of behaviour management technology dissemination in pediatric dentistry. Pediatr Dent. 1990; 12:79–82. PMID: 2151957.15. Technique for behavior management--a survey. The Association of Pedodontic Diplomates. ASDC J Dent Child. 1972; 39:368–372. PMID: 4263500.16. Chow CH, Van Lieshout RJ, Schmidt LA, Dobson KG, Buckley N. Systematic review: audiovisual interventions for reducing preoperative anxiety in children undergoing elective surgery. J Pediatr Psychol. 2016; 41:182–203. PMID: 26476281.
Article17. Xiaolian J, Xiaolin L, Lan ZH. Effects of visual and audiovisual distraction on pain and anxiety among patients undergoing colonoscopy. Gastroenterol Nurs. 2015; 38:55–61. PMID: 25636013.
Article18. Dedeepya P, Nuvvula S, Kamatham R, Nirmala SV. Behavioural and physiological outcomes of biofeedback therapy on dental anxiety of children undergoing restorations: a randomised controlled trial. Eur Arch Paediatr Dent. 2014; 15:97–103. PMID: 23907736.
Article19. Ingersoll BD, Nash DA, Gamber C. The use of contingent audiotaped material with pediatric dental patients. J Am Dent Assoc. 1984; 109:717–719. PMID: 6208228.
Article20. Stark LJ, Allen KD, Hurst M, Nash DA, Rigney B, Stokes TF. Distraction: its utilization and efficacy with children undergoing dental treatment. J Appl Behav Anal. 1989; 22:297–307. PMID: 2793636.
Article21. Navit S, Johri N, Khan SA, Singh RK, Chandha D, Navit P, et al. Effectiveness and comparison of various audio distraction aids in management of anxious dental Pediatric patients. J Clin Diagn Res. 2015; 9:ZC05–ZC09.22. Williams JA, Hurst MK, Stokes TF. Peer observation in decreasing uncooperative behavior in young dental patients. Behav Modif. 1983; 7:225–242. PMID: 6679298.
Article23. Klesges RC, Malott JM, Ugland M. The effects of graded exposure and parental modeling on the dental phobias of a four year old girl and her mother. J Behav Ther Exp Psychiatry. 1984; 15:161–164. PMID: 6148360.24. Allen KD, Stokes TF. The use of escape and reward in the management of young children during dental treatment. J Appl Behav Anal. 1987; 20:381–390. PMID: 3429360.25. Willis WD, Coggeshall RE. Sensory mechanism of the spinal cord. 2nd ed. New York: Plenum Press;1991.26. Aminabadi NA, Farahani RM, Balayi Gajan E. The efficacy of distraction and counterstimulation in the reduction of pain reaction to intraoral injection by pediatric patients. J Contemp Dent Pract. 2008; 9:33–40.
Article27. Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965; 150:971–979. PMID: 5320816.
Article28. Filcheck HA, Allen KD, Ogren H, Darby JB, Holstein B, Hupp S. The use of choice-based distraction to decrease the distress of children at the dentist. Child Fam Behav Ther. 2004; 26:59–68.
Article29. Ram D, Shapira J, Holan G, Magora F, Cohen S, Davidoch E. Audiovisual video eyeglass distraction during dental treatment in children. Quintessence Int. 2010; 41:673–679. PMID: 20657857.30. Patel A, Schieble T, Davidson M, Tran MC, Schoenberg C, Delphin E, et al. Distraction with a handheld video game reduces pediatric preoperative anxiety. Paediatr Anaesth. 2006; 16:1019–1027. PMID: 16972829.
Article31. Wismeijer AA, Vingerhoets AJ. The use of virtual reality and audiovisual eyeglasses system as adjunct analgesic techniques: a review of the literature. Ann Behav Med. 2005; 30:268–278. PMID: 16336078.32. Slifer KJ, Tucker CL, Dahlquist LM. Helping children and caregivers cope with repeated invasive procedures: how are we doing? J Clin Psychol. 2002; 9:131–152.33. Niharika P, Reddy NV, Srujana P, Srikanth K, Daneswari V, Geetha KS. Effects of distraction using virtual reality technology on pain perception and anxiety levels in children during pulp therapy of primary molars. J Indian Soc Pedod Prev Dent. 2018; 36:364–369. PMID: 30324926.
Article34. Panda A. Effect of virtual reality distraction on pain perception during dental treatment in children. Int J Oral Res. 2017; 5:278–281.
Article35. Agarwal N, Dhawan J, Kumar D, Anand A, Tangri K. Effectiveness of two topical anaesthetic agents used along with audio visual aids in pediatric dental patients. J Clin Diagn Res. 2017; 11:ZC80–ZC83. PMID: 28274051.36. American Academy Pediatric Dentistry. Reference manual guideline on behavior guidance for the pediatric dental patient. Pediatr Dent. 2015; 37:182–193.37. ANTVR. http://antvr.com/en/ANTVR_PhoneGlassE.html.38. Bare LC, Dundes L. Strategies for combating dental anxiety. J Dent Educ. 2004; 68:1172–1177. PMID: 15520236.
Article39. Aartman IH, van Everdingen T, Hoogstraten J, Schuurs AH. Self-report measurements of dental anxiety and fear in children: a critical assessment. ASDC J Dent Child. 1998; 65:252–258. PMID: 9740944.40. Wong DL, Baker CM. Pain in children: comparison of assessment scales. Pediatric Nursing. 1988; 14:9–17. PMID: 3344163.41. Powell CV, Kelly AM, Williams A. Determining the minimum clinically significant difference in visual analog pain score for children. Ann Emerg Med. 2001; 37:28–31. PMID: 11145767.
Article42. Venham LL, Gaulin-Kremer E, Munster E, Bengston-Audia D, Cohan J. Interval rating scales for children's dental anxiety and uncooperative behavior. Pediatr Dent. 1980; 2:195–202. PMID: 6938934.43. Aitken RC. A growing edge of measurement of feelings measurement of feelings using visual analogue scales. Proc Roy Soc Med. 1969; 62:989–993. PMID: 4899510.44. Khatri A, Kalra N. A comparison of two pain scales in the assessment of dental pain in East Delhi children. ISRN Dent. 2012; 2012:247351. PMID: 22461986.
Article45. Ohnhaus EE. Methodological problems in the measurement of pain. A comparison between the verbal rating scale and the visual analogue scale. Pain. 1975; 1:379–384. PMID: 800639.
Article46. Luyk NH, Beck FM, Weaver JM. A visual analogue scale in the assessment of dental anxiety. Anesth Prog. 1988; 35:121–123. PMID: 3166350.47. Yelderman M, New W Jr. Evaluation of pulse oximetry. Anesthesiology. 1983; 59:349–352. PMID: 6614545.
Article48. Martin MD, Ramsay DS, Whitney C, Fiset L, Weinstein P. Topical anesthesia: Differentiating the pharmacological and psychological contributions to efficacy. Anesth Prog. 1994; 41:40–47. PMID: 8638859.49. Bankole OO, Aderinokun GA, Denloye OO, Jeboda SO. Maternal and child's anxiety-effect on child's behaviour at dental appointments and treatments. Afr J Med Med Sci. 2002; 31:349–352. PMID: 15027778.50. Cianetti S, Paglia L, Gatto R, Montedori A, Lupatelli E. Evidence of pharmacological and non-pharmacological interventions for the management of dental fear in Pediatric dentistry: a systematic review protocol. BMJ Open. 2017; 7:e016043.51. McCaul KD, Malott JM. Distraction and coping with pain. Psychol Bull. 1984; 95:516–533. PMID: 6399756.
Article52. Caffery Mc, Pasero C. Pain: Clinical Manual. 2nd ed. St. Louis, MO: Mosby;1999. p. 399–427.53. Khandelwal D, Kalra N, Tyagi R, Khatri A, Gupta K. Control of anxiety in pediatric patients using “Tell Show Do” method and audiovisual distraction. J Contemp Dent Pract. 2018; 19:1058–1064. PMID: 30287704.54. Al-Khotani A, Bello LA, Christidis N. Effects of audiovisual distraction on children's behaviour during dental treatment: a randomised controlled clinical trial. Acta Odontol Scand. 2016; 74:494–501. PMID: 27409593.55. Fakhruddin KS, El Batawi HY. Effectiveness of audiovisual distraction in behavior modification during dental caries assessment and sealant placement in children with autism spectrum disorder. Dent Res J (Isfahan). 2017; 14:177–182. PMID: 28702058.
Article56. Shah HA, Nanjunda Swamy KV, Kulkarni S, Choubey S. Evaluation of dental anxiety and hemodynamic changes (Sympatho-Adrenal Response) during various dental procedures using smartphone applications v/s traditional behaviour management techniques in pediatric patients. Int J Adv Res. 2017; 3:429–433.57. Nuvvula S, Alahari S, Kamatham R, Challa RR. Effect of audiovisual distraction with 3D video glasses on dental anxiety of children experiencing administration of local analgesia: a randomised clinical trial. Eur Arch Paediatr Dent. 2015; 16:43–50. PMID: 25256207.
Article58. Asl Aminabadi N, Erfanparast L, Sohrabi A, Ghertasi Oskouei S, Naghili A. The impact of virtual reality distraction on pain and anxiety during dental treatment in 4-6 year-old children: a randomised controlled clinical trial. J Dent Res Dent Clin Dent Prospects. 2012; 6:117–124. PMID: 23277857.59. El-Sharkawi HF, EI-Housseiny AA, Aly AM. Effectiveness of new distraction technique on pain associated with injection of local anesthesia for children. Pediatr Dent. 2012; 34:e35–e38.60. Mitrakul K, Asvanund Y, Arunakul M, Paka-akaekaphat S. Effect of audiovisual eyeglasses during dental treatment in 5-8 year-old children. Eur J Paediatr Dent. 2015; 16:239–245. PMID: 26418930.61. Fakhruddin KS, El Batawi H, Gorduysus MO. Effectiveness of audiovisual distraction eyewear and computerized delivery of anesthesia during pulp therapy of primary molars in phobic child patients. Eur J Dent. 2015; 9:470–475. PMID: 26929683.
Article62. Hoge MA, Howard MR, Wallace DP, Allen KD. Use of video eyewear to manage distress in children during restorative dental treatment. Pediatr Dent. 2012; 34:378–382. PMID: 23211912.63. Sullivan C, Schneider PE, Musselman RJ, Dummett CO, Gardiner D. The effect of virtual reality during dental treatment on child anxiety and behavior. ASDC J Dent Child. 2000; 67:193–196. 160–161. PMID: 10902078.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of kaleidoscope, virtual reality, and video games to alleviate dental anxiety during local anesthesia in children: a randomized clinical trial
- Effect of Virtual Reality Distraction on Pain and Anxiety in Children during Local Anesthesia
- Effect of audio distraction with thermomechanical stimulation on pain perception for inferior alveolar nerve block in children: a randomized clinical trial
- The effect of vibratory stimulus on pain perception during intraoral local anesthesia administration in children: a systematic review and meta-analysis
- Comparative evaluation of the effectiveness of two innovative methods in the management of anxiety in a dental office: a randomized controlled trial