J Korean Orthop Assoc.
2019 Oct;54(5):393-401. 10.4055/jkoa.2019.54.5.393.
Ultrasound-Guided Shoulder Injections
- Affiliations
-
- 1Department of Orthopedic Surgery, Chosun University Hospital, Gwangju, Korea. nevereverhuhh@hanmail.net
- 2SunJaeMyeong Orthopedics Clinic, Boseong, Korea.
- KMID: 2461228
- DOI: http://doi.org/10.4055/jkoa.2019.54.5.393
Abstract
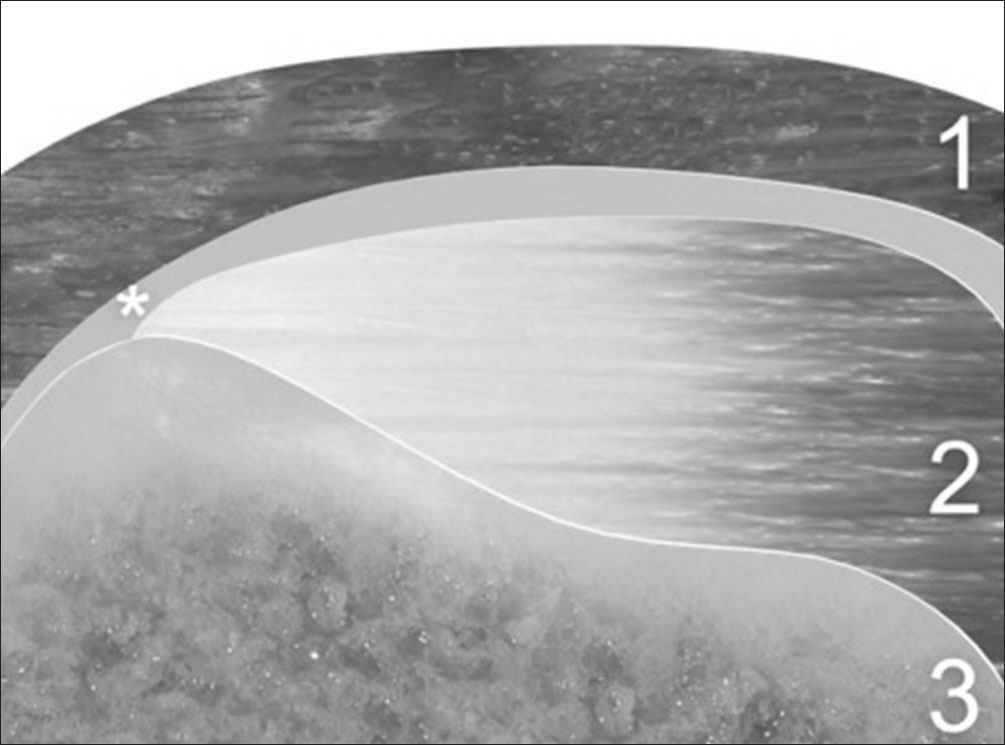
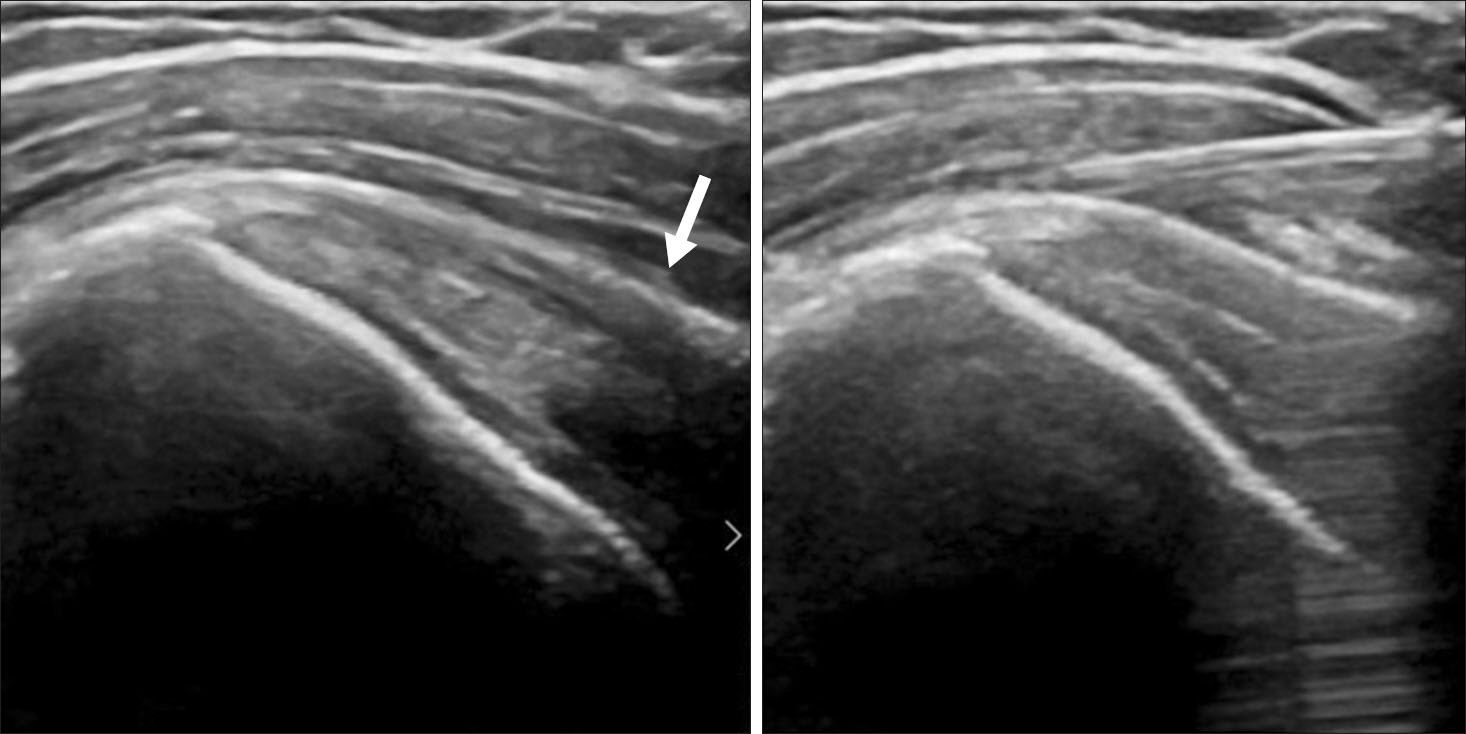
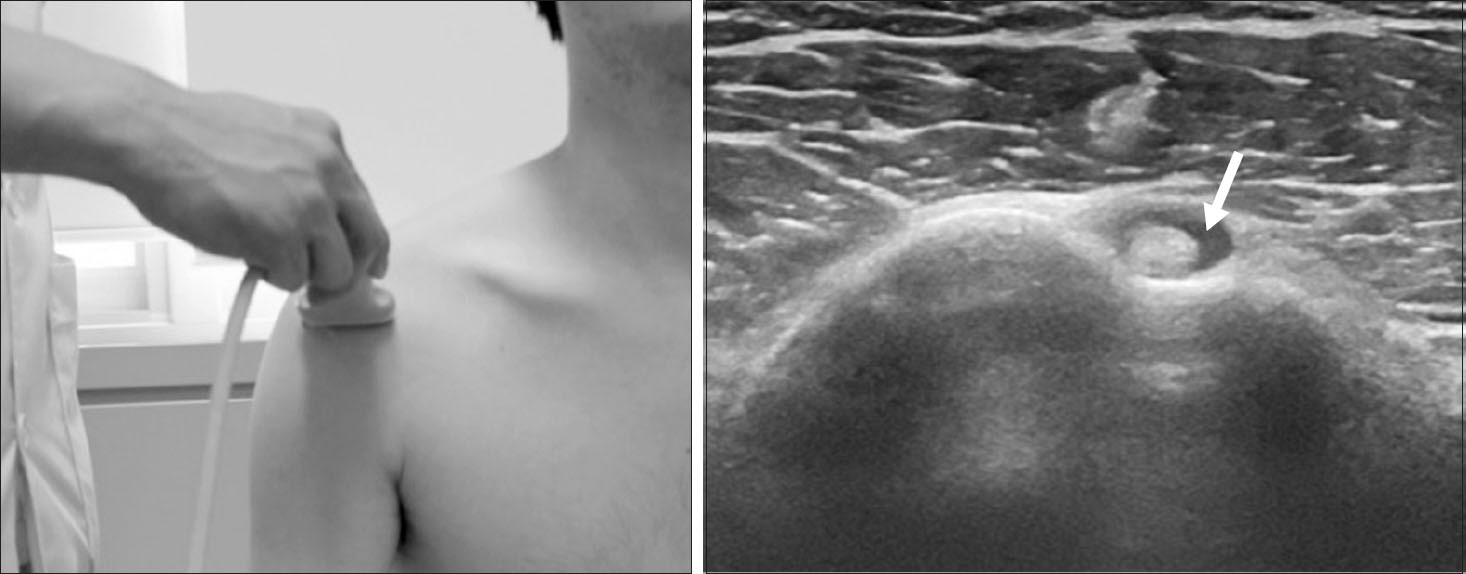
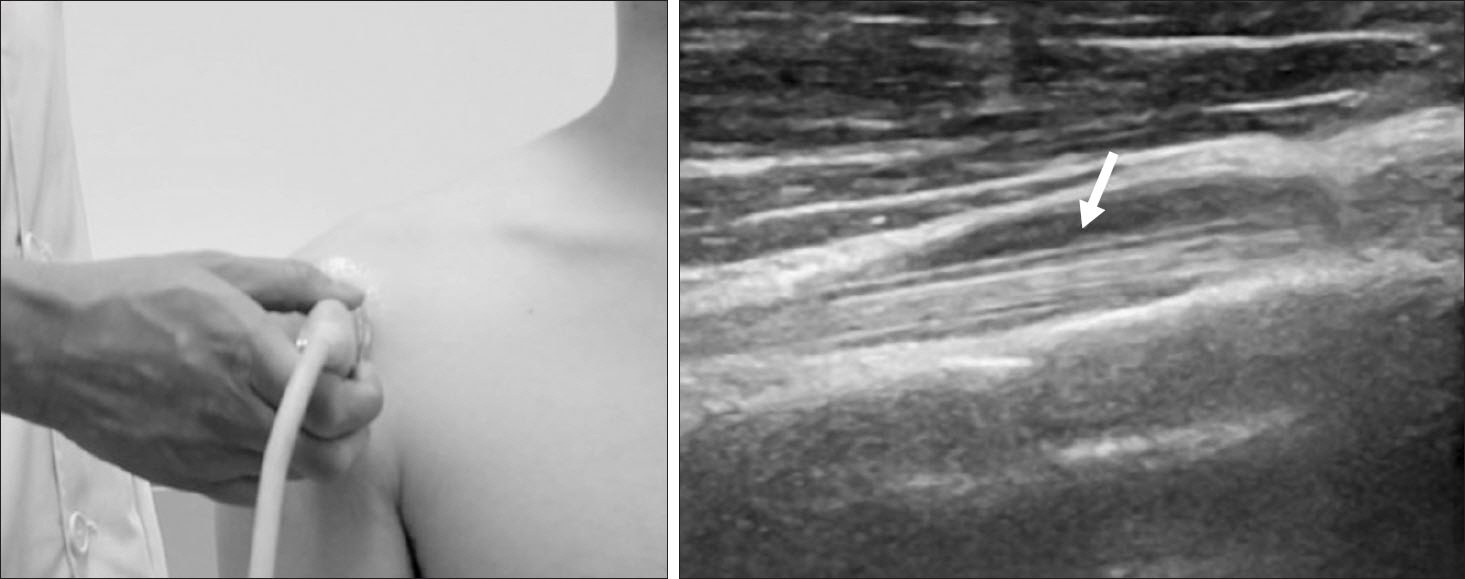
- The shoulder pain is one of the most common problems to orthopaedic surgeons in clinic. Among therapeutic modality used to manage this pain, joint and periarticular injection, as well as suprascapular nerve block, show good clinical outcome. Ultrasound guidance is a safe technique, increasing the safety and accuracy of the procedure and reducing complications. An accurate understanding of the surface anatomy is important in performing the ultrasound-guided shoulder injections. This article aims to describe the surface anatomy and sono anatomy of both the shoulder and the surrounding structures and also summarize different infiltration techniques and peripheral nerve blocks.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Hackett GS, Hemwall GA, Montgomery GA. Ligament and tendon relaxation (skeletal disability) treated by prolotherapy (fibro-osseous proliferation). Springfield;Charles C. Thomas: 1993. 139–295. 25–51.2. Hauser RA, Hauser MA, Pottinger K. Prolo your pain away!: curing chronic pain with prolotherapy. Oak Park: Beulah Land Press;1998. 71–194. 31–40. 1–8. 35–40. 25–26.3. Martinoli C, Bianchi S, Prato N. . US of the shoulder: non-rotator cuff disorders. Radiographics. 2003. 23:381–401; quiz 534.
Article4. O’Neill J. Musculoskeletal ultrasound: anatomy and technique. New York: Springer New York;2008. 21–54.5. Bach HG, Goldberg BA. Posterior capsular contracture of the shoulder. J Am Acad Orthop Surg. 2006. 14:265–77.
Article6. ElShewy MT. Calcific tendinitis of the rotator cuff. World J Orthop. 2016. 7:55–60.
Article7. Farin PU. Sonography of the biceps tendon of the shoulder: normal and pathologic findings. J Clin Ultrasound. 1996. 24:309–16.
Article8. Neviaser AS, Neviaser RJ. Adhesive capsulitis of the shoulder. J Am Acad Orthop Surg. 2011. 19:536–42.
Article9. Lee DH, Hong JY, Lee MY, Kwack KS, Yoon SH. Relation between subacromial bursitis on ultrasonography and efficacy of subacromial corticosteroid injection in rotator cuff disease: a prospective comparison study. Arch Phys Med Rehabil. 2017. 98:881–7.
Article10. Chen MJ, Lew HL, Hsu TC. . Ultrasound-guided shoulder injections in the treatment of subacromial bursitis. Am J Phys Med Rehabil. 2006. 85:31–5.
Article11. Laktasić-Zerjavić N. [Standardised ultrasound scanning of the elbow]. Reumatizam. 2010. 57::62-7. Croatian..12. Radunovic G, Vlad V, Micu MC. . Ultrasound assessment of the elbow. Med Ultrason. 2012. 14:141–6.13. Lee SM, Park SE, Nam YS. . Analgesic effectiveness of nerve block in shoulder arthroscopy: comparison between interscalene, suprascapular and axillary nerve blocks. Knee Surg Sports Traumatol Arthrosc. 2012. 20:2573–8.
Article14. Checcucci G, Allegra A, Bigazzi P, Gianesello L, Ceruso M, Gritti G. A new technique for regional anesthesia for ar-throscopic shoulder surgery based on a suprascapular nerve block and an axillary nerve block: an evaluation of the first results. Arthroscopy. 2008. 24:689–96.
Article15. Lee JJ, Kim DY, Hwang JT. . Effect of ultrasonographical-ly guided axillary nerve block combined with suprascapular nerve block in arthroscopic rotator cuff repair: a randomized controlled trial. Arthroscopy. 2014. 30:906–14.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound Guidance for Intra-Articular Shoulder Injections for Frozen Shoulder
- Ultrasound-Guided Injection in the Management of Shoulder Pain
- A Comparison between the Anterior and Posterior Approach to US-guided Shoulder Articular Injections for MR Arthrography
- Accuracy of Ultrasound-Guided and Non-guided Botulinum Toxin Injection Into Neck Muscles Involved in Cervical Dystonia: A Cadaveric Study
- Feasibility of Ultrasound-Guided Intraarticular Contrast Injection for MR Arthrography