Brain Tumor Res Treat.
2019 Oct;7(2):112-121. 10.14791/btrt.2019.7.e35.
Demographic and Socioeconomic Factors for Renouncing Further Active Therapy for Patients with Brain Metastasis of Non-Small Cell Lung Cancer
- Affiliations
-
- 1Division of Neuro-Oncology and Department of Neurosurgery, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea. yzkim@skku.edu
- 2Division of Hematology and Medical Oncology, Department of Internal Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
- 3Department of Radiation Oncology, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
- KMID: 2461184
- DOI: http://doi.org/10.14791/btrt.2019.7.e35
Abstract
- BACKGROUND
As patients with brain metastasis (BM) of non-small cell lung cancer (NSCLC) have dismal prognosis, some of them decide to discontinue further treatment for BM. The objective of this study was to determine factors for renouncing further active therapy in patients with BM of NSCLC, focusing on their demographic and socioeconomic status.
METHODS
Medical records of 105 patients with radiological diagnosis of BM of NSCLC for the recent 11 years at authors' institution were retrospectively reviewed. Clinical features as well as demographic and socioeconomic characteristics such as marriage status, cohabiting family members, religious affiliations, educational background, and economic responsibility were reviewed.
RESULTS
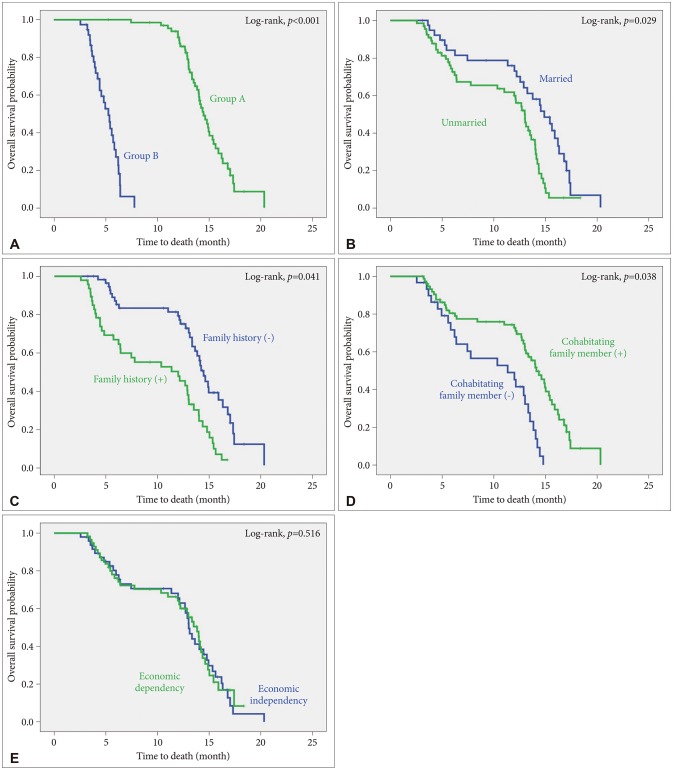
Median overall survival (OS) was 13.84 (95% CI: 10.26-17.42) years in 67 patients (group A) who underwent active treatment (radiotherapy and/or chemotherapy) and 4.76 (95% CI: 3.12-6.41) years in 38 patients (group B) who renounced active treatment. Less patients were unmarried (p=0.046), more cohabitating family members (p=0.008), and economically independent (p=0.014) in group A than those in group B. Similarly, the unmarried, and none cohabitating family members had short OS (5.17 and 7.38 years, respectively). In multivariate analysis for predisposing factors of OS in these patients, the following demographic and socioeconomic factors had independent significance: marriage status and cohabitating family members.
CONCLUSION
This study suggests that demographic and socioeconomic status as well as clinical factors could influence the decision of further active treatment and prognosis of patients with BM of NSCLC.
Keyword
MeSH Terms
Figure
Reference
-
1. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011; 61:69–90. PMID: 21296855.
Article2. Malvezzi M, Bertuccio P, Levi F, La Vecchia C, Negri E. European cancer mortality predictions for the year 2013. Ann Oncol. 2013; 24:792–800. PMID: 23402763.
Article3. International Agency for Research on Cancer, World Health Organization. Cancer fact sheets: estimated cancer incidence, mortality and prevalence worldwide in 2012. Globocan 2012. Accessed November 8, 2018. at: http://gco.iarc.fr/today/data/pdf/fact-sheets/cancers/cancerfact-sheets-11.pdf.4. Jung KW, Won YJ, Kong HJ, Lee ES. Prediction of cancer incidence and mortality in Korea, 2018. Cancer Res Treat. 2018; 50:317–323. PMID: 29566480.
Article5. National Cancer Institute. Cancer stat facts: lung and bronchus cancer. Surveillance, Epidemiology and End Results Program. Accessed November 8, 2018. at: https://seer.cancer.gov.6. Preusser M, Winkler F, Valiente M, et al. Recent advances in the biology and treatment of brain metastases of non-small cell lung cancer: summary of a multidisciplinary roundtable discussion. ESMO Open. 2018; 3:e000262. PMID: 29387475.
Article7. Barnholtz-Sloan JS, Sloan AE, Davis FG, Vigneau FD, Lai P, Sawaya RE. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol. 2004; 22:2865–2872. PMID: 15254054.
Article8. Kohler BA, Ward E, McCarthy BJ, et al. Annual report to the nation on the status of cancer, 1975-2007, featuring tumors of the brain and other nervous system. J Natl Cancer Inst. 2011; 103:714–736. PMID: 21454908.
Article9. DeAngelis LM, Posner JB. Intracranial metastases. In : DeAngelis LM, Posner JB, editors. Neurologic complications of cancer. New York: Oxford University Press;2009. p. 141–193.10. Toyokawa G, Seto T, Takenoyama M, Ichinose Y. Insights into brain metastasis in patients with ALK+ lung cancer: is the brain truly a sanctuary? Cancer Metastasis Rev. 2015; 34:797–805. PMID: 26342831.
Article11. Mamon HJ, Yeap BY, Jänne PA, et al. High risk of brain metastases in surgically staged IIIA non-small-cell lung cancer patients treated with surgery, chemotherapy, and radiation. J Clin Oncol. 2005; 23:1530–1537. PMID: 15735128.
Article12. Sperduto PW, Kased N, Roberge D, et al. Summary report on the graded prognostic assessment: an accurate and facile diagnosis-specific tool to estimate survival for patients with brain metastases. J Clin Oncol. 2012; 30:419–425. PMID: 22203767.
Article13. Tsao MN, Xu W, Wong RK, et al. Whole brain radiotherapy for the treatment of newly diagnosed multiple brain metastases. Cochrane Database Syst Rev. 2018; 1:CD003869. PMID: 29365347.
Article14. Reck M, Popat S, Reinmuth N, De Ruysscher D, Kerr KM, Peters S. ESMO Guidelines Working Group. Metastatic non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014; 25 Suppl 3:iii27–iii39. PMID: 25115305.
Article15. Chang WS, Kim HY, Chang JW, Park YG, Chang JH. Analysis of radiosurgical results in patients with brain metastases according to the number of brain lesions: is stereotactic radiosurgery effective for multiple brain metastases? J Neurosurg. 2010; 113 Suppl:73–78. PMID: 21121789.
Article16. Rosen LS, Gordon D, Tchekmedyian NS, et al. Long-term efficacy and safety of zoledronic acid in the treatment of skeletal metastases in patients with nonsmall cell lung carcinoma and other solid tumors: a randomized, Phase III, double-blind, placebo-controlled trial. Cancer. 2004; 100:2613–2621. PMID: 15197804.17. Dayan A, Koca D, Akman T, Oztop I, Ellidokuz H, Yilmaz U. The factors that have an impact on the development of brain metastasis in the patients with breast cancer. J Cancer Res Ther. 2012; 8:542–548. PMID: 23361272.18. Karnofsky DA, Abelmann WH, Craver LF, Burchenal JH. The use of the nitrogen mustards in the palliative treatment of carcinoma. With particular reference to bronchogenic carcinoma. Cancer. 1948; 1:634–656.19. Li J, Wang M, Won M, et al. Validation and simplification of the Radiation Therapy Oncology Group recursive partitioning analysis classification for glioblastoma. Int J Radiat Oncol Biol Phys. 2011; 81:623–630. PMID: 20888136.
Article20. Sperduto PW, Chao ST, Sneed PK, et al. Diagnosis-specific prognostic factors, indexes, and treatment outcomes for patients with newly diagnosed brain metastases: a multi-institutional analysis of 4,259 patients. Int J Radiat Oncol Biol Phys. 2010; 77:655–661. PMID: 19942357.
Article21. Cardoso G, Graca J, Klut C, Trancas B, Papoila A. Depression and anxiety symptoms following cancer diagnosis: a cross-sectional study. Psychol Health Med. 2016; 21:562–570. PMID: 26683266.
Article22. Zhang MF, Wen YS, Liu WY, Peng LF, Wu XD, Liu QW. Effectiveness of mindfulness-based therapy for reducing anxiety and depression in patients with cancer: a meta-analysis. Medicine (Baltimore). 2015; 94:e0897. PMID: 26559246.23. Opie RS, Itsiopoulos C, Parletta N, et al. Dietary recommendations for the prevention of depression. Nutr Neurosci. 2017; 20:161–171. PMID: 26317148.
Article24. Gokal K, Wallis D, Ahmed S, Boiangiu I, Kancherla K, Munir F. Effects of a self-managed home-based walking intervention on psychosocial health outcomes for breast cancer patients receiving chemotherapy: a randomised controlled trial. Support Care Cancer. 2016; 24:1139–1166. PMID: 26275768.
Article25. Savard J, Morin CM. Insomnia in the context of cancer: a review of a neglected problem. J Clin Oncol. 2001; 19:895–908. PMID: 11157043.
Article26. Ganguli A, Henk H, Teitelbaum A, Ray S. PCN39 Burden of brain metastasis in an metastatic non-small cell lung cancer (NSCLC) population. Value Health. 2011; 14:A440–A441.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Cutaneous Metastasis from Small Cell Lung Cancer
- A case of leptomeningeal metastasis from adenocarcinoma of the lung improved by treatment with Gefitinib
- A Case of Iris Metastasis from Non-small Cell Lung Cancer
- Ovarian Metastasis from Non-Small Cell Lung Cancer Responding to Erlotinib
- Radiotherapy of Brain Metastases from Lung Cancer