Diabetes Metab J.
2019 Oct;43(5):615-626. 10.4093/dmj.2018.0128.
Association between Change in Alcohol Consumption and Metabolic Syndrome: Analysis from the Health Examinees Study
- Affiliations
-
- 1Department of Biomedical Sciences, Seoul National University Graduate School, Seoul, Korea. fmpark1@snu.ac.kr
- 2Department of Family Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 3JW Lee Center for Global Medicine, Seoul, Korea.
- 4Department of Preventive Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 5Department of Environmental Medicine, Seoul National University Medical Research Center, Seoul, Korea.
- KMID: 2460955
- DOI: http://doi.org/10.4093/dmj.2018.0128
Abstract
- BACKGROUND
The association between change in alcohol intake and metabolic syndrome is unclear.
METHODS
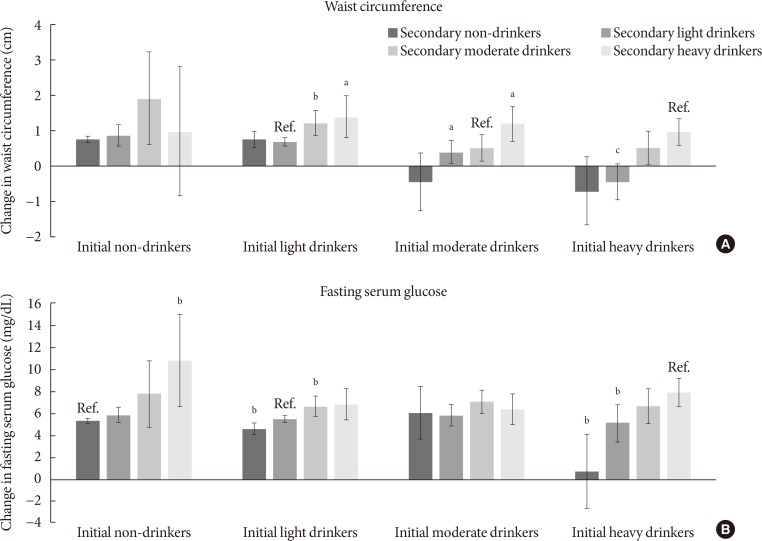
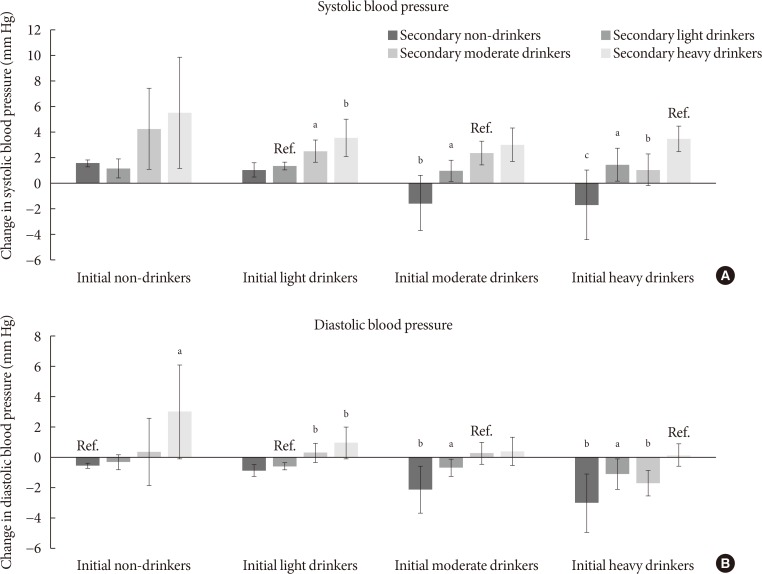
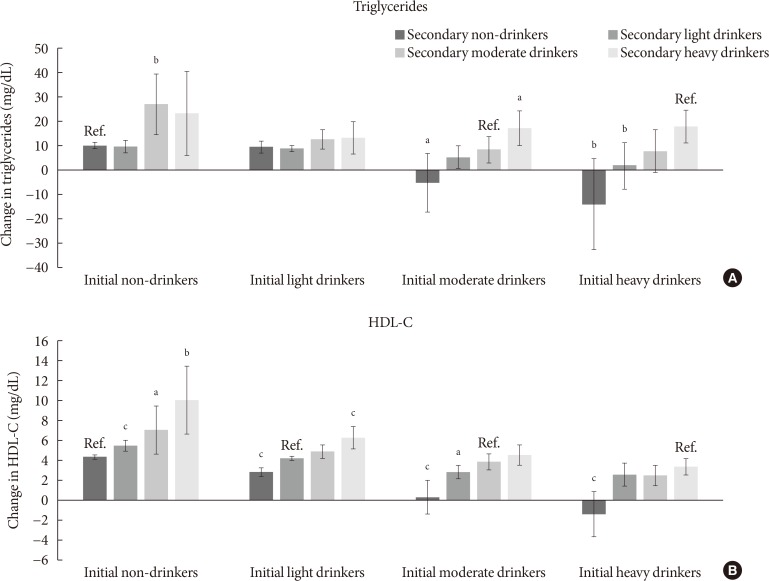
This retrospective cohort consisted of 41,368 males and females from the Health Examinees-GEM study. Participants were divided into non-drinkers (0.0 g/day), light drinkers (male: 0.1 to 19.9 g/day; female: 0.1 to 9.9 g/day), moderate drinkers (male: 20.0 to 39.9 g/day; female: 10.0 to 19.9 g/day), and heavy drinkers (male: ≥40.0 g/day; female: ≥20.0 g/day) for each of the initial and follow-up health examinations. Logistic regression analysis was used to determine the adjusted odds ratios (aORs) and 95% confidence intervals (CIs) for developing metabolic syndrome according to the change in alcohol consumption between the initial and follow-up health examinations. Adjusted mean values for the change in waist circumference, fasting serum glucose (FSG), blood pressure, triglycerides, and high density lipoprotein cholesterol (HDL-C) levels were determined according to the change in alcohol consumption by linear regression analysis.
RESULTS
Compared to persistent light drinkers, those who increased alcohol intake to heavy levels had elevated risk of metabolic syndrome (aOR, 1.45; 95% CI, 1.09 to 1.92). In contrast, heavy drinkers who became light drinkers had reduced risk of metabolic syndrome (aOR, 0.61; 95% CI, 0.44 to 0.84) compared to persistent heavy drinkers. Increased alcohol consumption was associated with elevated adjusted mean values for waist circumference, FSG, blood pressure, triglycerides, and HDL-C levels (all P<0.05). Reduction in alcohol intake was associated with decreased waist circumference, FSG, blood pressure, triglycerides, and HDL-C levels among initial heavy drinkers (all P<0.05).
CONCLUSION
Heavy drinkers who reduce alcohol consumption could benefit from reduced risk of metabolic syndrome.
MeSH Terms
Figure
Reference
-
1. Eckel RH, Alberti KG, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2010; 375:181–183. PMID: 20109902.
Article2. Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, Montori VM. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007; 49:403–414. PMID: 17258085.3. Cornier MA, Dabelea D, Hernandez TL, Lindstrom RC, Steig AJ, Stob NR, Van Pelt RE, Wang H, Eckel RH. The metabolic syndrome. Endocr Rev. 2008; 29:777–822. PMID: 18971485.
Article4. Stoutenberg M, Lee DC, Sui X, Hooker S, Horigian V, Perrino T, Blair S. Prospective study of alcohol consumption and the incidence of the metabolic syndrome in US men. Br J Nutr. 2013; 110:901–910. PMID: 23340203.
Article5. Gigleux I, Gagnon J, St-Pierre A, Cantin B, Dagenais GR, Meyer F, Despres JP, Lamarche B. Moderate alcohol consumption is more cardioprotective in men with the metabolic syndrome. J Nutr. 2006; 136:3027–3032. PMID: 17116715.
Article6. Sun K, Ren M, Liu D, Wang C, Yang C, Yan L. Alcohol consumption and risk of metabolic syndrome: a meta-analysis of prospective studies. Clin Nutr. 2014; 33:596–602. PMID: 24315622.
Article7. Shin S, Lee HW, Kim CE, Lim J, Lee JK, Lee SA, Kang D. Egg consumption and risk of metabolic syndrome in Korean adults: results from the health examinees study. Nutrients. 2017; 9:E687. PMID: 28671590.
Article8. Ahn Y, Kwon E, Shim JE, Park MK, Joo Y, Kimm K, Park C, Kim DH. Validation and reproducibility of food frequency questionnaire for Korean genome epidemiologic study. Eur J Clin Nutr. 2007; 61:1435–1441. PMID: 17299477.
Article9. Yang JJ, Song M, Yoon HS, Lee HW, Lee Y, Lee SA, Choi JY, Lee JK, Kang D. What are the major determinants in the success of smoking cessation: results from the health examinees study. PLoS One. 2015; 10:e0143303. PMID: 26633704.
Article10. Jung SJ, Park SK, Shin A, Lee SA, Choi JY, Hong YC, Yoo KY, Lee JK, Kang D. Body mass index at age 18-20 and later risk of spontaneous abortion in the Health Examinees Study (HEXA). BMC Pregnancy Childbirth. 2015; 15:228. PMID: 26403183.
Article11. Health Examinees Study Group. The Health Examinees (HEXA) study: rationale, study design and baseline characteristics. Asian Pac J Cancer Prev. 2015; 16:1591–1597. PMID: 25743837.12. Choi J, Choi JY, Shin A, Lee SA, Lee KM, Oh J, Park JY, Lee JK, Kang D. Trends and correlates of high-risk alcohol consumption and types of alcoholic beverages in middle-aged Korean adults: results from the HEXA-G study. J Epidemiol. 2019; 29:125–132. PMID: 30146528.
Article13. Cho Y, Choi S, Kim K, Lee G, Park SM. Association between alcohol consumption and bone mineral density in elderly Korean men and women. Arch Osteoporos. 2018; 13:46. PMID: 29696513.
Article14. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002; 106:3143–3421. PMID: 12485966.15. Kim BJ, Kim BS, Kang JH. Alcohol consumption and incidence of metabolic syndrome in Korean men. A 3-year follow-up study. Circ J. 2012; 76:2363–2371. PMID: 22785081.16. Baik I, Shin C. Prospective study of alcohol consumption and metabolic syndrome. Am J Clin Nutr. 2008; 87:1455–1463. PMID: 18469271.
Article17. Yeomans MR, Caton S, Hetherington MM. Alcohol and food intake. Curr Opin Clin Nutr Metab Care. 2003; 6:639–644. PMID: 14557794.
Article18. Kim JY, Lee DY, Lee YJ, Park KJ, Kim KH, Kim JW, Kim WH. Chronic alcohol consumption potentiates the development of diabetes through pancreatic β-cell dysfunction. World J Biol Chem. 2015; 6:1–15. PMID: 25717351.
Article19. Rupp H, Brilla CG, Maisch B. Hypertension and alcohol: central and peripheral mechanisms. Herz. 1996; 21:258–264. PMID: 8805006.20. Potter JF, Watson RD, Skan W, Beevers DG. The pressor and metabolic effects of alcohol in normotensive subjects. Hypertension. 1986; 8:625–631. PMID: 3522422.
Article21. Arkwright PD, Beilin LJ, Vandongen R, Rouse IA, Lalor C. The pressor effect of moderate alcohol consumption in man: a search for mechanisms. Circulation. 1982; 66:515–519. PMID: 7094262.
Article22. Altura BM, Altura BT. Microvascular and vascular smooth muscle actions of ethanol, acetaldehyde, and acetate. Fed Proc. 1982; 41:2447–2451. PMID: 7044829.23. Husain K, Ansari RA, Ferder L. Alcohol-induced hypertension: mechanism and prevention. World J Cardiol. 2014; 6:245–252. PMID: 24891935.
Article24. Mudrakova E, Poledne R, Kovar J. Postprandial triglyceridemia after single dose of alcohol in healthy young men. Nutr Metab Cardiovasc Dis. 2013; 23:183–188. PMID: 21917433.25. Schneider J, Liesenfeld A, Mordasini R, Schubotz R, Zofel P, Kubel F, Vandre-Plozzitzka C, Kaffarnik H. Lipoprotein fractions, lipoprotein lipase and hepatic triglyceride lipase during short-term and long-term uptake of ethanol in healthy subjects. Atherosclerosis. 1985; 57:281–291. PMID: 4084359.
Article26. Klop B, do Rego AT, Cabezas MC. Alcohol and plasma triglycerides. Curr Opin Lipidol. 2013; 24:321–326. PMID: 23511381.
Article27. Fraser GE, Anderson JT, Foster N, Goldberg R, Jacobs D, Blackburn H. The effect of alcohol on serum high density lipoprotein (HDL). A controlled experiment. Atherosclerosis. 1983; 46:275–286. PMID: 6405757.28. Haskell WL, Camargo C Jr, Williams PT, Vranizan KM, Krauss RM, Lindgren FT, Wood PD. The effect of cessation and resumption of moderate alcohol intake on serum high-density-lipoprotein subfractions. A controlled study. N Engl J Med. 1984; 310:805–810. PMID: 6366553.29. Crouse JR, Grundy SM. Effects of alcohol on plasma lipoproteins and cholesterol and triglyceride metabolism in man. J Lipid Res. 1984; 25:486–496. PMID: 6736783.
Article30. Taskinen MR, Nikkila EA, Valimaki M, Sane T, Kuusi T, Kesaniemi A, Ylikahri R. Alcohol-induced changes in serum lipoproteins and in their metabolism. Am Heart J. 1987; 113:458–464. PMID: 3544760.
Article31. Clevidence BA, Reichman ME, Judd JT, Muesing RA, Schatzkin A, Schaefer EJ, Li Z, Jenner J, Brown CC, Sunkin M, Campbell WS, Taylor PR. Effects of alcohol consumption on lipoproteins of premenopausal women. A controlled diet study. Arterioscler Thromb Vasc Biol. 1995; 15:179–184. PMID: 7749823.32. De Oliveira E Silva ER, Foster D, McGee Harper M, Seidman CE, Smith JD, Breslow JL, Brinton EA. Alcohol consumption raises HDL cholesterol levels by increasing the transport rate of apolipoproteins A-I and A-II. Circulation. 2000; 102:2347–2352. PMID: 11067787.
Article33. Chartier K, Caetano R. Ethnicity and health disparities in alcohol research. Alcohol Res Health. 2010; 33:152–160. PMID: 21209793.34. Williams GD, Aitken SS, Malin H. Reliability of self-reported alcohol consumption in a general population survey. J Stud Alcohol. 1985; 46:223–227. PMID: 4010299.
Article35. Giovannucci E, Colditz G, Stampfer MJ, Rimm EB, Litin L, Sampson L, Willett WC. The assessment of alcohol consumption by a simple self-administered questionnaire. Am J Epidemiol. 1991; 133:810–817. PMID: 2021148.36. Hines LM, Stampfer MJ, Ma J, Gaziano JM, Ridker PM, Hankinson SE, Sacks F, Rimm EB, Hunter DJ. Genetic variation in alcohol dehydrogenase and the beneficial effect of moderate alcohol consumption on myocardial infarction. N Engl J Med. 2001; 344:549–555. PMID: 11207350.
Article37. Beulens JW, Rimm EB, Hendriks HF, Hu FB, Manson JE, Hunter DJ, Mukamal KJ. Alcohol consumption and type 2 diabetes: influence of genetic variation in alcohol dehydrogenase. Diabetes. 2007; 56:2388–2394. PMID: 17563066.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Alcohol Consumption, Liver Enzymes, and Prevalence of Metabolic Syndrome in Korean Adult Men
- Association between green tea consumption and metabolic syndrome among Korean adults: results from the Health Examinees study
- The effect of moderate alcohol drinking in nonalcoholic fatty liver disease
- Association between Alcohol Consumption and Metabolic Syndrome Determined by Facial Flushing in Korean Women
- Alcohol Consumption and Diabetes Mellitus