Differential Control Rate of Systolic and Diastolic Blood Pressure among Korean Adults with Hypertension: the Sixth Korean National Health and Nutrition Examination Survey, 2013–2015 (KNHANES VI)
- Affiliations
-
- 1Department of Public Health, Yonsei University Graduate School, Seoul, Korea.
- 2Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea. hckim@yuhs.ac
- 3Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 4Division of Cardiology, Ewha Womans University Mokdong Hospital, Seoul, Korea.
- 5Cardiovascular and Metabolic Diseases Etiology Research Center, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2460529
- DOI: http://doi.org/10.4070/kcj.2019.0049
Abstract
- BACKGROUND AND OBJECTIVES
Discrepancy in blood pressure (BP) control rate may be owed to different risk factors associated with elevated systolic and diastolic BP (SBP and DBP).
METHODS
In a nationally representative survey of Korean population with BP measurements, a total of 5,100 participants with hypertension was included in the analyses. Three separate types of control rates were calculated: SBP, DBP, and (combined) S&DBP among all participants with hypertension and participants with treated hypertension, separately. Control rates were compared across sex and age groups. Multivariable logistic regression was used to identify demographic factors associated with SBP, DBP, and S&DBP control rates, separately.
RESULTS
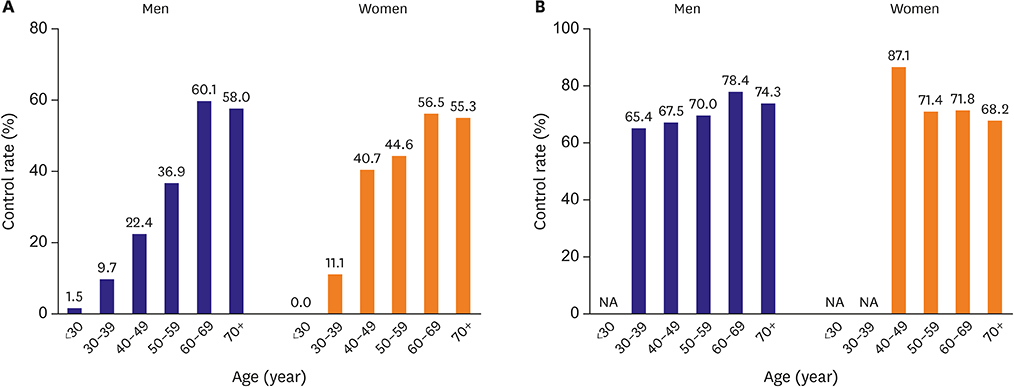
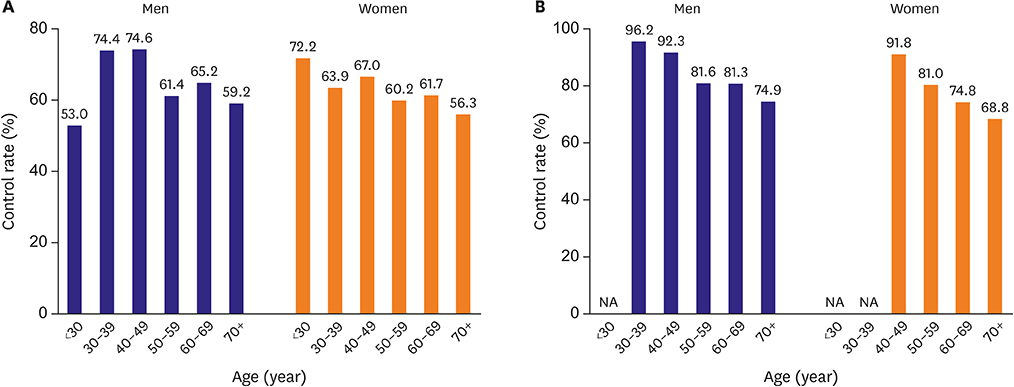
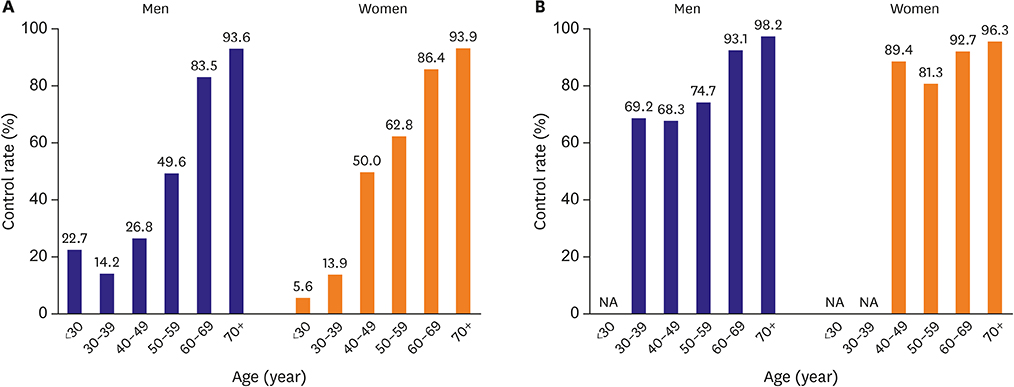
In total, SBP, DBP, and S&DBP control rates were 63.0%, 63.7%, and 42.5% among all hypertension patients, and 77.5%, 87.4%, and 71.6% among treated hypertension patients. Men aged 40-49 years with hypertension and 30-39 years treated for hypertension had the highest SBP control rate (74.6% and 96.2%), which decreased by older age. Inversely, DBP control rate progressively increased with older age. SBP control rate among women with hypertension was the highest in 40-49 years (67.0%) but without linear trend by age group. Interestingly, both combined and DBP control rates were noticeably low among women aged 50-59 years. Women with body mass index ≥25 were at higher odds of having controlled SBP. Lower DBP control rate was observed in men with lower education level, higher household income, and heavy drinkers.
CONCLUSIONS
Separate examination of control rates demonstrated different sex- and age-differential trends, which would have been overlooked in combined control rates.
Keyword
MeSH Terms
Figure
Cited by 5 articles
-
Control Rates of Systolic and Diastolic Blood Pressure among Hypertensive Adults in Korea
Takashi Hisamatsu
Korean Circ J. 2019;49(11):1049-1051. doi: 10.4070/kcj.2019.0197.Do We Know the Normal Blood Pressure Level in Korean Children and Adolescents?
Lucy Youngmin Eun
Korean Circ J. 2019;49(12):1181-1182. doi: 10.4070/kcj.2019.0273.Big Challenge in Big Data Research: Continual Dispute on Big Data Analysis
Hae-Young Lee
Korean Circ J. 2020;50(1):69-71. doi: 10.4070/kcj.2019.0349.Implementation of National Health Policy for the Prevention and Control of Cardiovascular Disease in South Korea: Regional-Local Cardio-Cerebrovascular Center and Nationwide Registry
Ju Mee Wang, Byung Ok Kim, Jang-Whan Bae, Dong-Jin Oh
Korean Circ J. 2021;51(5):383-398. doi: 10.4070/kcj.2021.0001.Suboptimal Management Status of Younger Hypertensive Population in Korea
Hae-Young Lee, Gyu Chul Oh, Il Suk Sohn, Sungha Park, Jinho Shin, Wook Bum Pyun, Myeong-Chan Cho
Korean Circ J. 2021;51(7):598-606. doi: 10.4070/kcj.2020.0542.
Reference
-
1. GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018; 392:1923–1994.2. Korean Society Hypertension (KSH). Hypertension Epidemiology Research Working Group. Kim HC, Cho MC. Korea hypertension fact sheet 2018. Clin Hypertens. 2018; 24:13.
Article3. Lee H, Park S, Kim HC. Temporal and geospatial trends of hypertension management in Korea: a nationwide study 2002-2016. Korean Circ J. 2019; 49:e36.
Article4. Shin J, Park JB, Kim KI, et al. 2013 Korean Society of Hypertension guidelines for the management of hypertension: part I-epidemiology and diagnosis of hypertension. Clin Hypertens. 2015; 21:1.
Article5. Shin J, Park JB, Kim KI, et al. 2013 Korean Society of Hypertension guidelines for the management of hypertension. Part II-treatments of hypertension. Clin Hypertens. 2015; 21:2.
Article6. Kweon S, Kim Y, Jang MJ, et al. Data resource profile: the Korea national Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014; 43:69–77.
Article7. Kim Y. The Korea National Health and Nutrition Examination Survey (KNHANES): current status and challenges. Epidemiol Health. 2014; 36:e2014002.
Article8. Oh JY, Yang YJ, Kim BS, Kang JH. Validity and reliability of Korean version of International Physical Activity Questionnaire (IPAQ) short form. J Korean Acad Fam Med. 2007; 28:532–541.9. World Health Organization. The Asia-Pacific perspective: redefining obesity and its treatment. Geneva: World Health Organization;2000.10. Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013; 310:959–968.
Article11. Bavishi C, Goel S, Messerli FH. Isolated systolic hypertension: an update after SPRINT. Am J Med. 2016; 129:1251–1258.
Article12. Fang J, Madhavan S, Cohen H, Alderman MH. Isolated diastolic hypertension. A favorable finding among young and middle-aged hypertensive subjects. Hypertension. 1995; 26:377–382.13. Nielsen WB, Lindenstrøm E, Vestbo J, Jensen GB. Is diastolic hypertension an independent risk factor for stroke in the presence of normal systolic blood pressure in the middle-aged and elderly? Am J Hypertens. 1997; 10:634–639.
Article14. Leonetti G, Cuspidi C, Facchini M, Stramba-Badiale M. Is systolic pressure a better target for antihypertensive treatment than diastolic pressure? J Hypertens Suppl. 2000; 18:S13–20.15. Böhm M, Schumacher H, Teo KK, et al. Achieved blood pressure and cardiovascular outcomes in high-risk patients: results from ONTARGET and TRANSCEND trials. Lancet. 2017; 389:2226–2237.
Article16. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2018; 71:e127–248.17. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014; 311:507–520.18. Hense HW, Maziak W, Heidrich J. Why is blood pressure control unsatisfactory--or is it? Nephrol Dial Transplant. 2002; 17:1547–1550.
Article19. Izumi Y, Matsumoto K, Ozawa Y, et al. Effect of age at menopause on blood pressure in postmenopausal women. Am J Hypertens. 2007; 20:1045–1050.
Article20. Maas AH, Franke HR. Women's health in menopause with a focus on hypertension. Neth Heart J. 2009; 17:68–72.
Article21. Lloyd-Jones DM, Evans JC, Larson MG, O'Donnell CJ, Roccella EJ, Levy D. Differential control of systolic and diastolic blood pressure: factors associated with lack of blood pressure control in the community. Hypertension. 2000; 36:594–599.22. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002; 106:3143–3421.23. Adab P, Pallan M, Whincup PH. Is BMI the best measure of obesity? BMJ. 2018; 360:k1274.
Article24. Hamer M, Stamatakis E. Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J Clin Endocrinol Metab. 2012; 97:2482–2488.
Article25. Chirinos JA, Franklin SS, Townsend RR, Raij L. Body mass index and hypertension hemodynamic subtypes in the adult US population. Arch Intern Med. 2009; 169:580–586.
Article26. Grotto I, Huerta M, Sharabi Y. Hypertension and socioeconomic status. Curr Opin Cardiol. 2008; 23:335–339.
Article27. Lee CJ, Ryu J, Kim HC, et al. Clinical benefit of treatment of stage-1, low-risk hypertension. Hypertension. 2018; 72:1285–1293.
Article28. Kim W, Kim S. Women's alcohol use and alcoholism in Korea. Subst Use Misuse. 2008; 43:1078–1087.
Article29. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010; 303:2043–2050.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Moderate Alcohol Consumption Does Not Prevent the Hypertension among Korean: the 2001 Korean National Health and Nutrition Examination Survey
- Prevalence and Trends of Isolated Systolic Hypertension among Korean Adults: the Korea National Health and Nutrition Examination Survey, 1998-2012
- Factors Related to Blood Pressure Control in Korean Adults with Hypertension: The Seventh Korea National Health and Nutrition Examination Survey, 2018
- Association between Parity and Blood Pressure in Korean Women: Korean National Health and Nutrition Examination Survey, 2010-2012
- Decision-Tree Analysis to Predict Blood Pressure Control Status Among Hypertension Patients Taking Antihypertensive Medications