Yeungnam Univ J Med.
2019 Sep;36(3):273-280. 10.12701/yujm.2019.00339.
Massive cerebral venous sinus thrombosis secondary to Graves' disease
- Affiliations
-
- 1Department of Radiology, Keimyung University Dongsan Hospital, Daegu, Korea. shmm11111@gmail.com
- KMID: 2460199
- DOI: http://doi.org/10.12701/yujm.2019.00339
Abstract
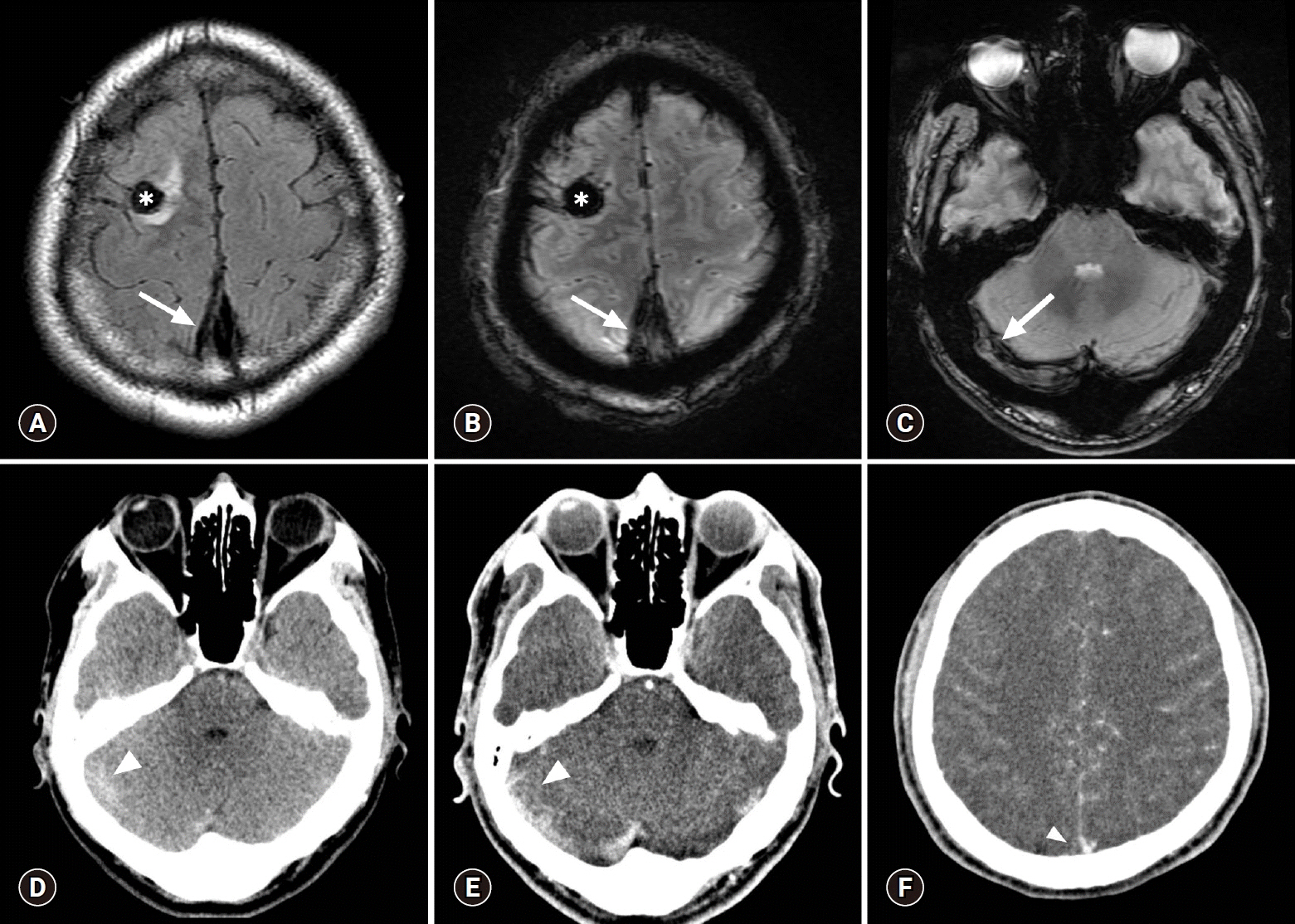
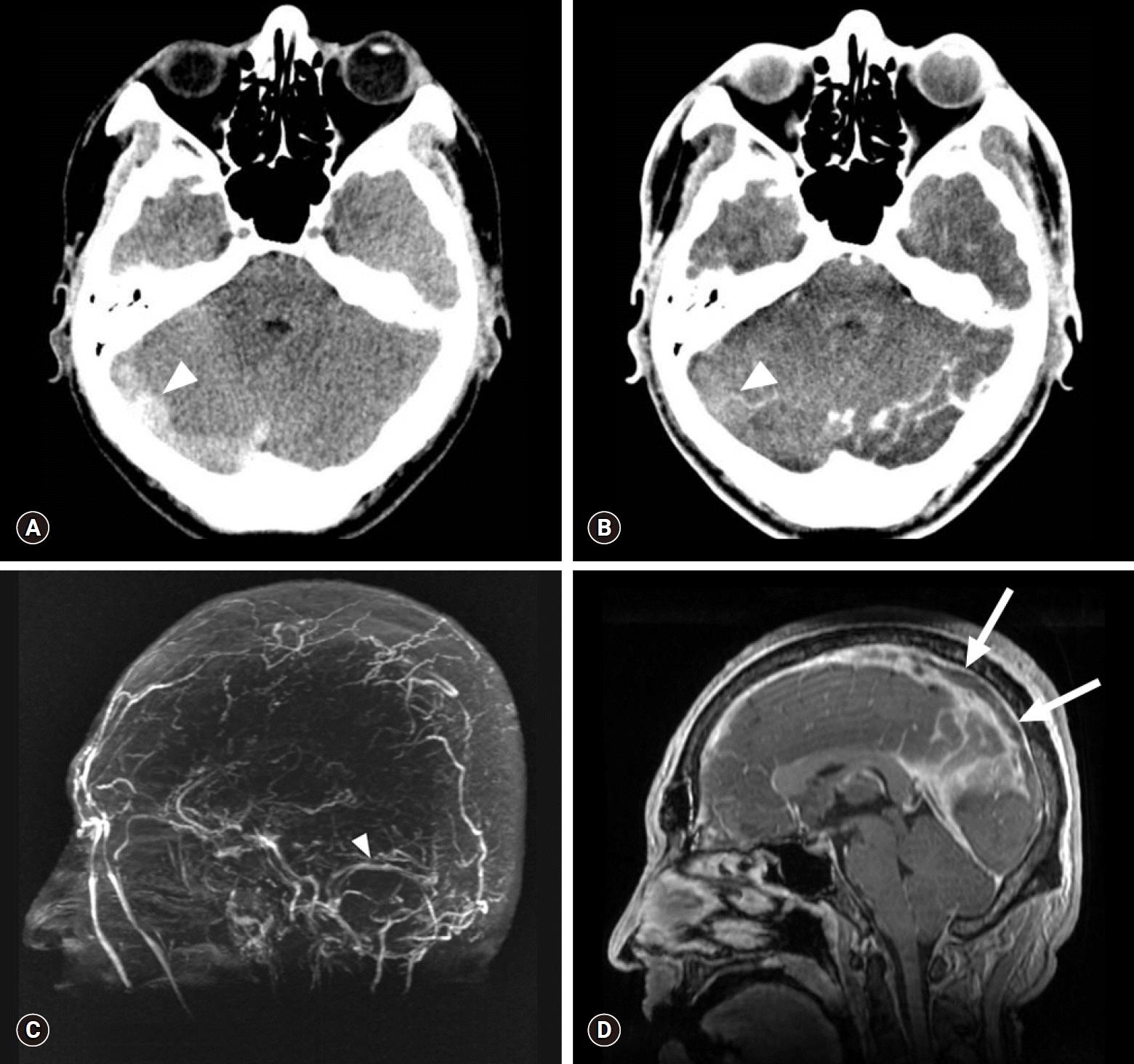
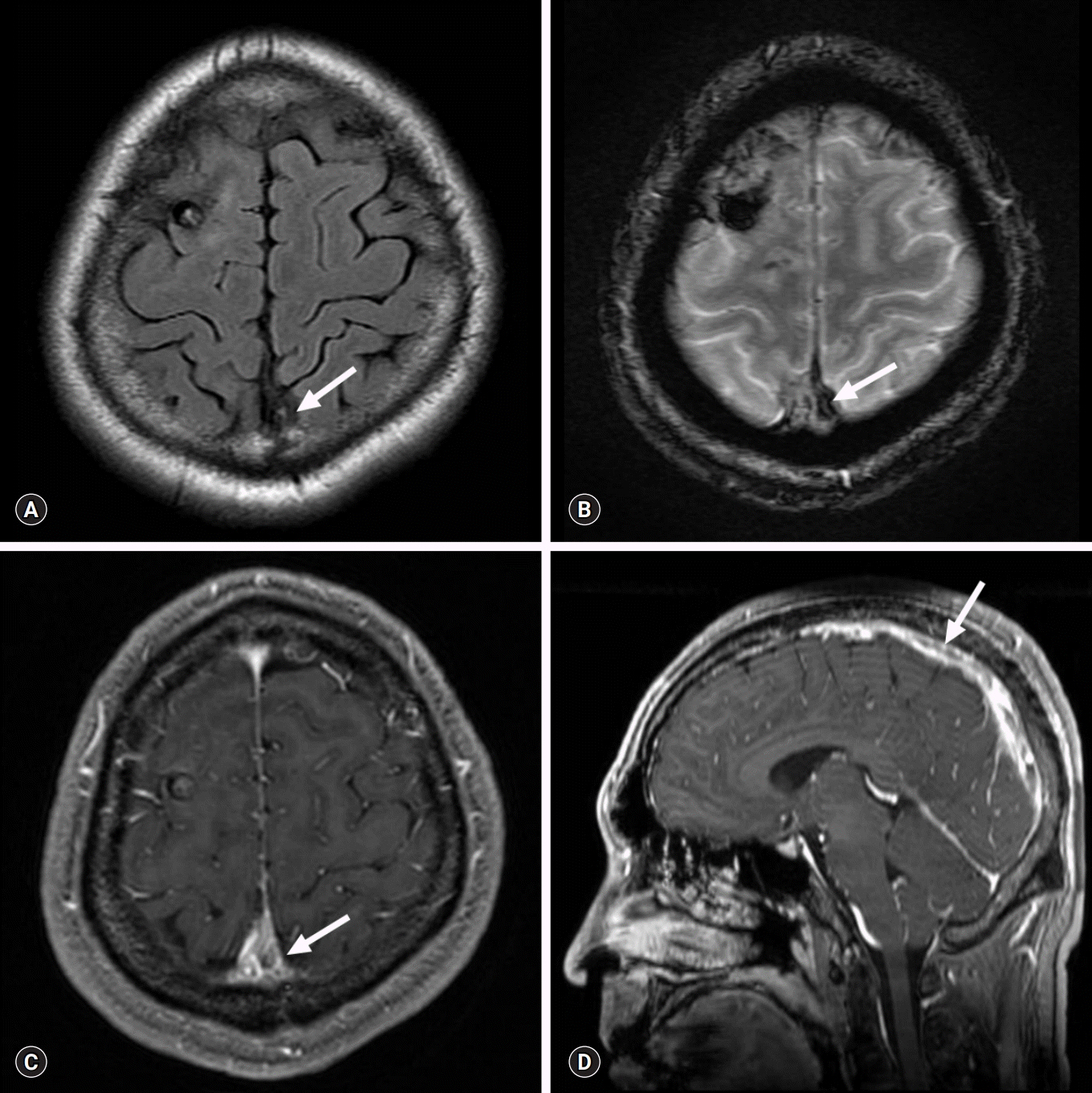
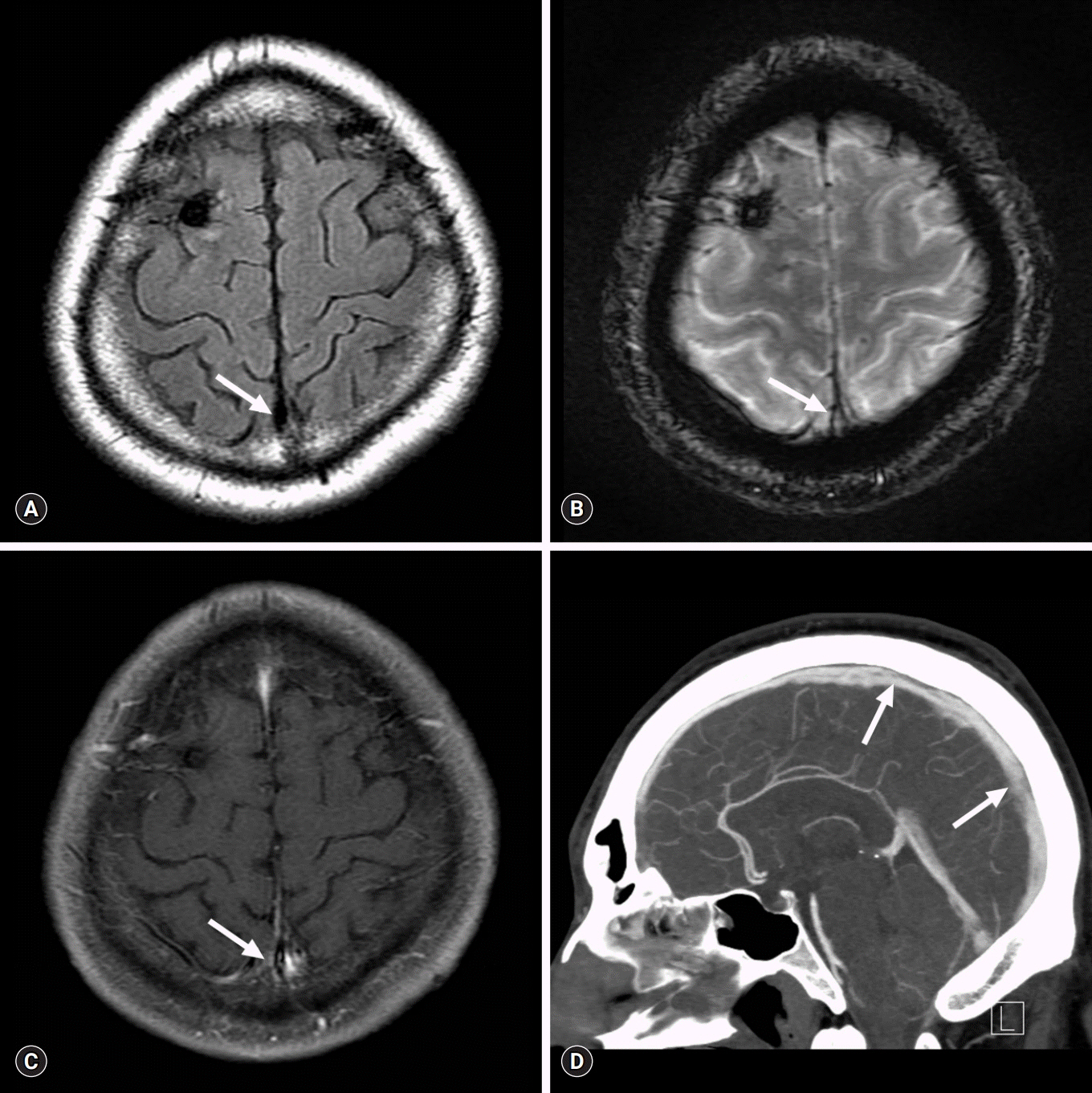
- Cerebral venous sinus thrombosis (CVT) is a rare cerebrovascular condition accounting for 0.5-1% of all types of strokes in the general population. Hyperthyroidism is associated with procoagulant and antifibrinolytic activity, thereby precipitating a hypercoagulable state that predisposes to CVT. We report the case of a 31-year-old Korean man with massive CVT and diagnosis of concomitant Graves' disease at admission. Early diagnosis and prompt treatment of CVT are important to improve prognosis; therefore, CVT should be considered in the differential diagnosis in all patients with hyperthyroidism presenting with neurological symptoms.
MeSH Terms
Figure
Reference
-
References
1. Einhäupl K, Bousser MG, de Bruijn SF, Ferro JM, Martinelli I, Masuhr F, et al. EFNS guideline on the treatment of cerebral venous and sinus thrombosis. Eur J Neurol. 2006; 13:553–9.
Article2. Saposnik G, Barinagarrementeria F, Brown RD Jr, Bushnell CD, Cucchiara B, Cushman M, et al. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011; 42:1158–92.
Article3. Kaliebe H. Autochthone sinusthrombose bei einem falle von morbus basedow und tabes. Med Klin. 1913; 9:1929–32.4. Doyle JB. Obstruction of the longitudinal sinus. Arch Neurol Psychiatry. 1927; 18:374–82.
Article5. Hermans E, Mariën P, De Deyn PP. Sinus sigmoideus thrombosis secondary to graves' disease: a case description. Case Rep Neurol. 2011; 3:203–9.
Article6. Hwang JU, Kwon KY, Hur JW, Lee JW, Lee HK. The role of hyperthyroidism as the predisposing factor for superior sagittal sinus thrombosis. J Cerebrovasc Endovasc Neurosurg. 2012; 14:251–4.
Article7. Merino M, Guijarro MG, Iglesias P, Aladro Y, Montero P. Thyrotoxicosis and cerebral venous sinus thrombosis, causality or chance alone? Endocrinol Nutr. 2012; 59:462–3.
Article8. Migeot M, Rutgers MP, Gille M. Puerperal cerebral sinus venous thrombosis and acute hyperthyroidism in Graves' disease. Acta Neurol Belg. 2013; 113:331–3.
Article9. Bensalah M, Squizzato A, Ould Kablia S, Menia H, Kemali Z. Cerebral vein and sinus thrombosis and hyperthyrodism: a case report and a systematic review of the literature. Thromb Res. 2011; 128:98–100.
Article10. Squizzato A, Romualdi E, Büller HR, Gerdes VE. Thyroid dysfunction and effects on coagulation and fibrinolysis: a systematic review. J Clin Endocrinol Metab. 2007; 92:2415–20.
Article11. Rosendaal FR. Venous thrombosis: a multicausal disease. Lancet. 1999; 353:1167–73.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Leptomeningeal Metastasis Associated with Cerebral Venous Thrombosis
- A Case of Cerebral Venous Thrombosis in a Patient with Graves' Disease
- Neuro-Behcet's Disease Presented with Cerebral Venous Sinus Thrombosis: A Case Report
- Cerebral Venous Sinus Thrombosis Associated with Antithrombin III Deficiency: A Case Report
- Development of Subdural Hemorrhage in a Patient With Cerebral Venous Sinus Thrombosis