Yeungnam Univ J Med.
2019 Sep;36(3):201-207. 10.12701/yujm.2019.00283.
Prepectoral breast reconstruction
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Catholic University of Daegu School of Medicine, Daegu, Korea. fdghfg26@cu.ac.kr
- KMID: 2460188
- DOI: http://doi.org/10.12701/yujm.2019.00283
Abstract
- Implant-based breast reconstruction is the most commonly used reconstruction technique after mastectomy. This is because skin-sparing mastectomy has become possible with advancements in oncology. In addition, the development of breast implants and the advent of acellular dermal matrices have reduced postoperative complications and resulted in superior cosmetic results. The most frequently performed surgical breast reconstruction procedure for the past 20 years was the insertion of an implant under the pectoralis major muscle by means of the dual plane approach. However, some patients suffered from pain and animation deformity caused by muscle manipulation. Recently, a prepectoral approach has been used to solve the above problems in select patients, and the results are similar to subpectoral results. However, this technique is not always chosen due to the number of considerations for successful surgery. In this article, we will discuss the emergence of prepectoral breast reconstruction, indications and contraindications, surgical procedures, and outcomes.
MeSH Terms
Figure
Reference
-
References
1. American Society of Plastic Surgeons. 2018 Plastic surgery statistics report [Internet]. Arlington Heights: American Society of Plastic Surgeons;2019. [cited 2019 Jun 27]. https://www.plasticsurgery.org/documents/News/Statistics/2018/plastic-surgery-statistics-full-report-2018.pdf.2. Schlenker JD, Bueno RA, Ricketson G, Lynch JB. Loss of silicone implants after subcutaneous mastectomy and reconstruction. Plast Reconstr Surg. 1978; 62:853–61.
Article3. Gruber RP, Kahn RA, Lash H, Maser MR, Apfelberg DB, Laub DR. Breast reconstruction following mastectomy: a comparison of submuscular and subcutaneous techniques. Plast Reconstr Surg. 1981; 67:312–7.4. Puckett CL, Croll GH, Reichel CA, Concannon MJ. A critical look at capsule contracture in subglandular versus subpectoral mammary augmentation. Aesthetic Plast Surg. 1987; 11:23–8.
Article5. Biggs TM, Yarish RS. Augmentation mammaplasty: a comparative analysis. Plast Reconstr Surg. 1990; 85:368–72.6. Spear SL, Pelletiere CV. Immediate breast reconstruction in two stages using textured, integrated-valve tissue expanders and breast implants. Plast Reconstr Surg. 2004; 113:2098–103.
Article7. Serra-Renom JM, Fontdevila J, Monner J, Benito J. Mammary reconstruction using tissue expander and partial detachment of the pectoralis major muscle to expand the lower breast quadrants. Ann Plast Surg. 2004; 53:317–21.
Article8. Hammond DC, Capraro PA, Ozolins EB, Arnold JF. Use of a skin-sparing reduction pattern to create a combination skin-muscle flap pocket in immediate breast reconstruction. Plast Reconstr Surg. 2002; 110:206–11.
Article9. Wainwright DJ. Use of an acellular allograft dermal matrix (AlloDerm) in the management of full-thickness burns. Burns. 1995; 21:243–8.
Article10. Salzberg CA. Nonexpansive immediate breast reconstruction using human acellular tissue matrix graft (AlloDerm). Ann Plast Surg. 2006; 57:1–5.
Article11. Kim IK, Park SO, Chang H, Jin US. Inhibition mechanism of acellular dermal matrix on capsule formation in expander-implant breast reconstruction after postmastectomy radiotherapy. Ann Surg Oncol. 2018; 25:2279–87.
Article12. Vidya R, Iqbal FM. A guide to prepectoral breast reconstruction: a new dimension to implant-based breast reconstruction. Clin Breast Cancer. 2017; 17:266–71.13. Ter Louw RP, Nahabedian MY. Prepectoral breast reconstruction. Plast Reconstr Surg. 2017; 140(5 Suppl):51S–9S.
Article14. Storm-Dickerson T, Sigalove N. Prepectoral breast reconstruction: the breast surgeon's perspective. Plast Reconstr Surg. 2017; 140(6 Suppl):43S–8S.15. Spear SL, Boehmler JH, Bogue DP, Mafi AA. Options in reconstructing the irradiated breast. Plast Reconstr Surg. 2008; 122:379–88.
Article16. Sigalove S, Maxwell GP, Sigalove NM, Storm-Dickerson TL, Pope N, Rice J, et al. Prepectoral implant-based breast reconstruction and postmastectomy radiotherapy: short-term outcomes. Plast Reconstr Surg Glob Open. 2017; 5:e1631.17. Sinnott CJ, Persing SM, Pronovost M, Hodyl C, McConnell D, Ott Young A. Impact of postmastectomy radiation therapy in prepectoral versus subpectoral implant-based breast reconstruction. Ann Surg Oncol. 2018; 25:2899–908.
Article18. Sbitany H, Gomez-Sanchez C, Piper M, Lentz R. Prepectoral breast reconstruction in the setting of postmastectomy radiation therapy: an assessment of clinical outcomes and benefits. Plast Reconstr Surg. 2019; 143:10–20.
Article19. Gabriel A, Maxwell GP. Implant selection in the setting of prepectoral breast reconstruction. Gland Surg. 2019; 8:36–42.
Article20. Salibian AH, Harness JK, Mowlds DS. Staged suprapectoral expander/implant reconstruction without acellular dermal matrix following nipple-sparing mastectomy. Plast Reconstr Surg. 2017; 139:30–9.
Article21. Kobraei EM, Cauley R, Gadd M, Austen WG Jr, Liao EC. Avoiding breast animation deformity with pectoralis-sparing subcutaneous direct-to-implant breast reconstruction. Plast Reconstr Surg Glob Open. 2016; 4:e708.
Article22. Reitsamer R, Peintinger F. Prepectoral implant placement and complete coverage with porcine acellular dermal matrix: a new technique for direct-to-implant breast reconstruction after nipple-sparing mastectomy. J Plast Reconstr Aesthet Surg. 2015; 68:162–7.
Article23. Woo A, Harless C, Jacobson SR. Revisiting an old place: single-surgeon experience on post-mastectomy subcutaneous implant-based breast reconstruction. Breast J. 2017; 23:545–53.
Article24. Eskenazi LB. New options for immediate reconstruction: achieving optimal results with adjustable implants in a single stage. Plast Reconstr Surg. 2007; 119:28–37.
Article25. Glasberg SB. The economics of prepectoral breast reconstruction. Plast Reconstr Surg. 2017; 140(6 Suppl):49S–52S.
Article26. Radovan C. Breast reconstruction after mastectomy using the temporary expander. Plast Reconstr Surg. 1982; 69:195–208.
Article27. Frey JD, Alperovich M, Weichman KE, Wilson SC, Hazen A, Saadeh PB, et al. Breast reconstruction using contour fenestrated alloderm: does improvement in design translate to improved outcomes? Plast Reconstr Surg Glob Open. 2015; 3:e505.28. Sigalove S. Options in acellular dermal matrix-device assembly. Plast Reconstr Surg. 2017; 140(6 Suppl):39S–42S.
Article29. Macadam SA, Lennox PA. Acellular dermal matrices: use in reconstructive and aesthetic breast surgery. Can J Plast Surg. 2012; 20:75–89.
Article30. Sigalove S, Maxwell GP, Sigalove NM, Storm-Dickerson TL, Pope N, Rice J, et al. Prepectoral implant-based breast reconstruction: rationale, indications, and preliminary results. Plast Reconstr Surg. 2017; 139:287–94.31. Zhu L, Mohan AT, Abdelsattar JM, Wang Z, Vijayasekaran A, Hwang SM, et al. Comparison of subcutaneous versus submuscular expander placement in the first stage of immediate breast reconstruction. J Plast Reconstr Aesthet Surg. 2016; 69:e77–86.
Article32. Bernini M, Calabrese C, Cecconi L, Santi C, Gjondedaj U, Roselli J, et al. Subcutaneous direct-to-implant breast reconstruction: surgical, functional, and aesthetic results after long-term follow-up. Plast Reconstr Surg Glob Open. 2016; 3:e574.33. Schaeffer CV, Dassoulas KR, Thuman J, Campbell CA. Early functional outcomes after prepectoral breast reconstruction: a case-matched cohort study. Ann Plast Surg. 2019; 82(6S Suppl 5):S399–403.34. Darrach H, Kraenzlin F, Khavanin N, Chopra K, Sacks JM. The role of fat grafting in prepectoral breast reconstruction. Gland Surg. 2019; 8:61–6.
Article35. Sbitany H, Piper M, Lentz R. Prepectoral breast reconstruction: a safe alternative to submuscular prosthetic reconstruction following nipple-sparing mastectomy. Plast Reconstr Surg. 2017; 140:432–43.
Article36. Cattelani L, Polotto S, Arcuri MF, Pedrazzi G, Linguadoca C, Bonati E. One-step prepectoral breast reconstruction with dermal matrix-covered implant compared to submuscular implantation: functional and cost evaluation. Clin Breast Cancer. 2018; 18:e703–11.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
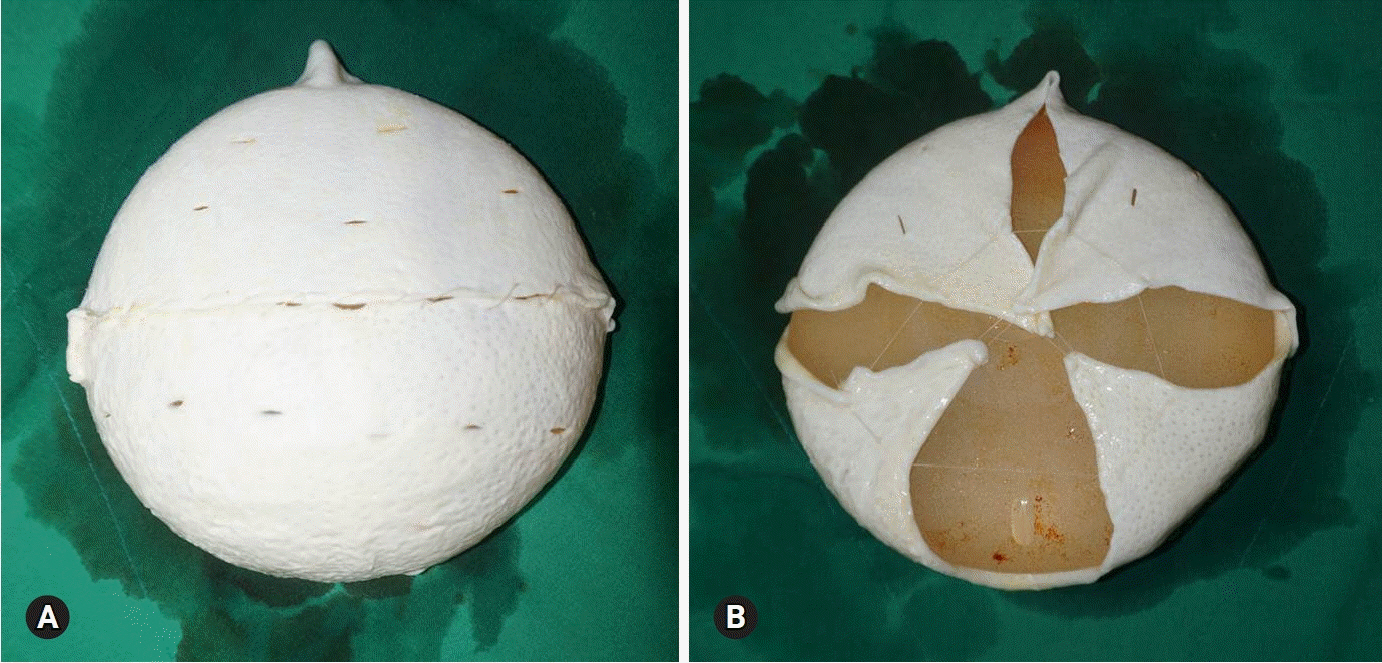
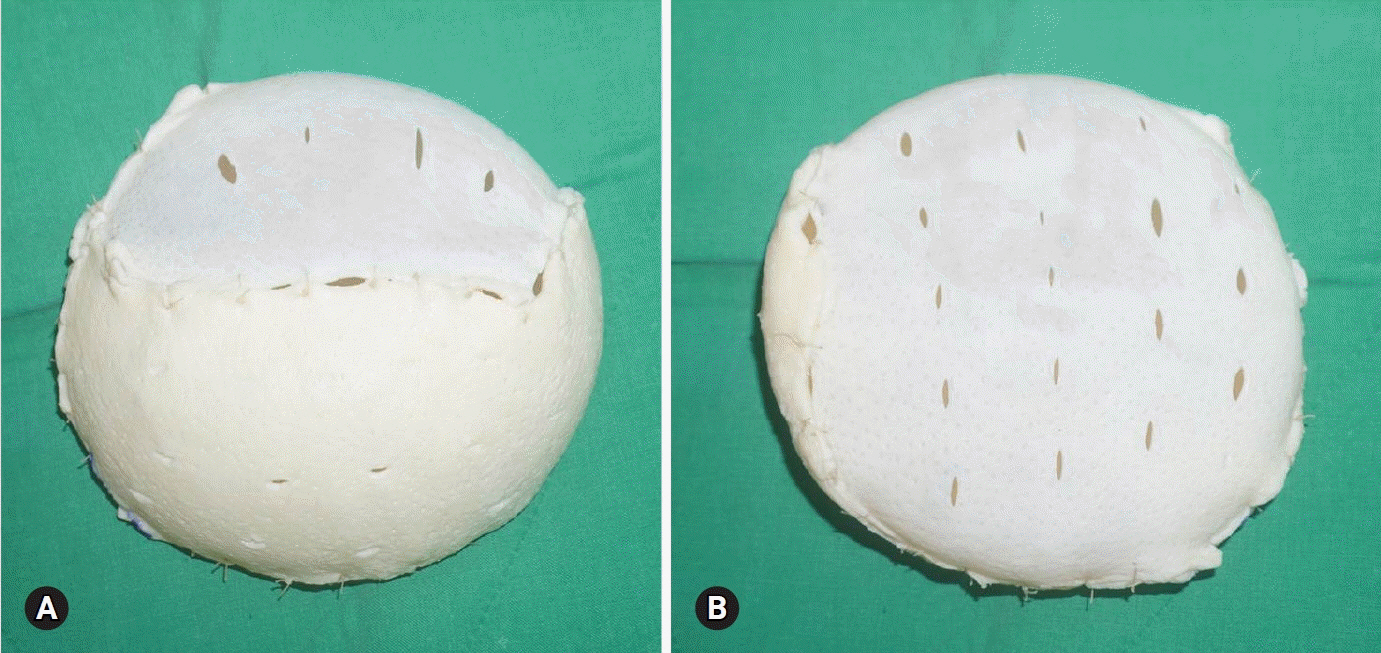
- Outcome of complete acellular dermal matrix wrap with polyurethane implant in immediate prepectoral breast reconstruction
- Considerations for patient selection: Prepectoral versus subpectoral implant-based breast reconstruction
- A prospective comparison of prepectoral and subpectoral methods for immediate breast reconstruction with acellular dermal matrix: the cogwheel-shaped anterior wrapping method
- A simple clinical assessment of breast animation deformity following direct-to-implant breast reconstruction
- Initial experiences and usefulness of porcine acellular dermal matrix-assisted prepectoral breast implant surgery: a case series and systematic review