J Endocr Surg.
2019 Sep;19(3):68-75. 10.16956/jes.2019.19.3.68.
Causes, Timing, and Safety of Completion Thyroidectomy during the Follow-up Period after Lobectomy: a Single-Center Experience
- Affiliations
-
- 1Department of Surgery, Yeungnam University Medical Center, Daegu, Korea. cjegs@yu.ac.kr
- KMID: 2458704
- DOI: http://doi.org/10.16956/jes.2019.19.3.68
Abstract
- PURPOSE
Thyroid lobectomy is a standard procedure for patients with papillary thyroid carcinoma (PTC) with tumor size <4 cm and clinically negative lymph nodes (LNs) and is performed more frequently than total thyroidectomy. Completion thyroidectomy (CT) is an unexpected operation after lobectomy that has an unpredictable complication rate. In this study, we evaluated the causes, timing, and safety of CT based on our experience.
METHODS
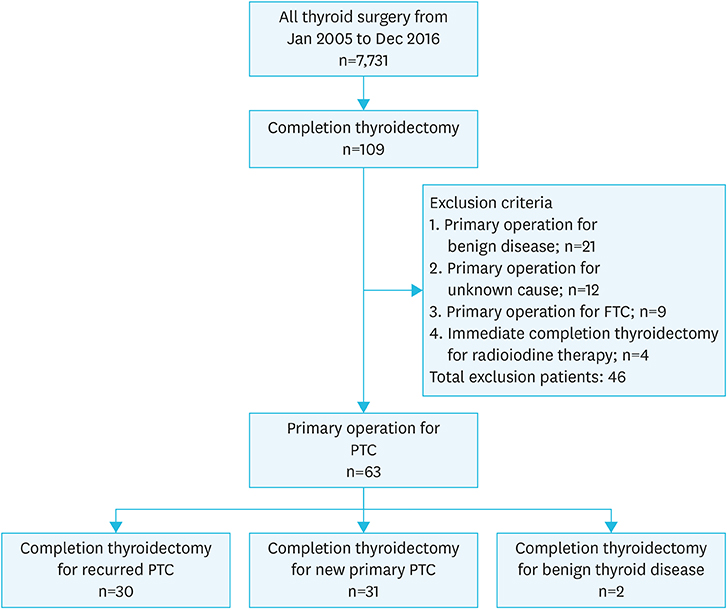
From January 2005 to December 2016, 7,731 patients underwent thyroid surgery in our institution. In this study, we included 63 patients who underwent CT for recurrent or contralateral thyroid disease during the follow-up period after lobectomy for PTC through retrospective chart review. We analyzed the causes and timing of CT, initial clinicopathologic factors of PTC, and the complication rate.
RESULTS
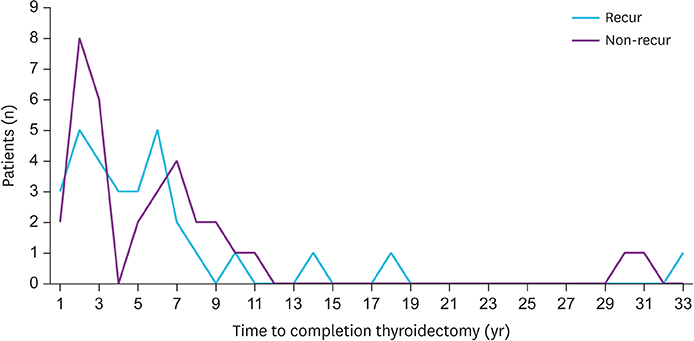
All patients underwent initial thyroid lobectomy for PTC. On initial pathology, mean tumor size was 0.69 cm and 7.9% (5/63) patients had central LN metastasis. Patients underwent CT after a mean of 68.4 months (6-388 months). The cause of CT was local or regional recurrence in 52.4% (30/63) of patients, contralateral PTC in 49.2% (31/63), and contralateral benign nodule in 3.17% (2/63). After CT, persistent hypoparathyroidism occurred in 1.58% (1/63), hoarseness in 1.58% (1/63), and wound infection in 1.58% (1/63).
CONCLUSION
CT may be performed for recurrent or non-recurrent causes anytime during the patient's lifetime after lobectomy. The postoperative complication rate is relatively low. Special attention should be paid during CT.
MeSH Terms
Figure
Reference
-
1. Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al. The Eighth Edition AJCC Cancer Staging Manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017; 67:93–99.
Article2. Mazzaferri EL. Management of low-risk differentiated thyroid cancer. Endocr Pract. 2007; 13:498–512.
Article3. Hay ID. Management of patients with low-risk papillary thyroid carcinoma. Endocr Pract. 2007; 13:521–533.
Article4. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016; 26:1–133.
Article5. Kısaoğlu A, Özoğul B, Akçay MN, Öztürk G, Atamanalp SS, Aydınlı B, et al. Completion thyroidectomy in differentiated thyroid cancer: when to perform? Ulus Cerrahi Derg. 2014; 30:18–21.
Article6. Lefevre JH, Tresallet C, Leenhardt L, Jublanc C, Chigot JP, Menegaux F. Reoperative surgery for thyroid disease. Langenbecks Arch Surg. 2007; 392:685–691.
Article7. Adam MA, Pura J, Gu L, Dinan MA, Tyler DS, Reed SD, et al. Extent of surgery for papillary thyroid cancer is not associated with survival: an analysis of 61,775 patients. Ann Surg. 2014; 260:601–605.8. Haigh PI, Urbach DR, Rotstein LE. Extent of thyroidectomy is not a major determinant of survival in low- or high-risk papillary thyroid cancer. Ann Surg Oncol. 2005; 12:81–89.
Article9. Nixon IJ, Ganly I, Patel SG, Palmer FL, Whitcher MM, Tuttle RM, et al. Thyroid lobectomy for treatment of well differentiated intrathyroid malignancy. Surgery. 2012; 151:571–579.
Article10. Matsuzu K, Sugino K, Masudo K, Nagahama M, Kitagawa W, Shibuya H, et al. Thyroid lobectomy for papillary thyroid cancer: long-term follow-up study of 1,088 cases. World J Surg. 2014; 38:68–79.
Article11. Hedman C, Strang P, Djärv T, Widberg I, Lundgren CI. Anxiety and fear of recurrence despite a good prognosis: an interview study with differentiated thyroid cancer patients. Thyroid. 2017; 27:1417–1423.
Article12. Vaisman F, Shaha A, Fish S, Michael Tuttle R. Initial therapy with either thyroid lobectomy or total thyroidectomy without radioactive iodine remnant ablation is associated with very low rates of structural disease recurrence in properly selected patients with differentiated thyroid cancer. Clin Endocrinol (Oxf). 2011; 75:112–119.
Article13. Durante C, Montesano T, Torlontano M, Attard M, Monzani F, Tumino S, et al. Papillary thyroid cancer: time course of recurrences during postsurgery surveillance. J Clin Endocrinol Metab. 2013; 98:636–642.
Article14. Grant CS. Recurrence of papillary thyroid cancer after optimized surgery. Gland Surg. 2015; 4:52–62.15. Pasieka JL, Thompson NW, McLeod MK, Burney RE, Macha M. The incidence of bilateral well-differentiated thyroid cancer found at completion thyroidectomy. World J Surg. 1992; 16:711–716.
Article16. Pitt SC, Sippel RS, Chen H. Contralateral papillary thyroid cancer: does size matter? Am J Surg. 2009; 197:342–347.
Article17. Hardman JC, Smith JA, Nankivell P, Sharma N, Watkinson JC. Re-operative thyroid surgery: a 20-year prospective cohort study at a tertiary referral centre. Eur Arch Otorhinolaryngol. 2015; 272:1503–1508.
Article18. Vaiman M, Nagibin A, Olevson J. Complications in primary and completed thyroidectomy. Surg Today. 2010; 40:114–118.
Article19. Rafferty MA, Goldstein DP, Rotstein L, Asa SL, Panzarella T, Gullane P, et al. Completion thyroidectomy versus total thyroidectomy: is there a difference in complication rates? An analysis of 350 patients. J Am Coll Surg. 2007; 205:602–607.
Article20. Rudolph N, Dominguez C, Beaulieu A, De Wailly P, Kraimps JL. The morbidity of reoperative surgery for recurrent benign nodular goitre: impact of previous unilateral thyroid lobectomy versus subtotal thyroidectomy. J Thyroid Res. 2014; 2014:231857.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Completion Thyroidectomy
- Safety of Completion Thyroidectomy for Thyroid Cancer
- Observational study of central metastases following thyroid lobectomy without a completion thyroidectomy for papillary carcinoma
- Is Completion Thyroidectomy Necessary in Patients with Papillary Thyroid Carcinoma who Underwent Lobectomy?
- Thyroid Lobectomy as an Initial Treatment Option on 1-4 cm Papillary Cancer