J Korean Foot Ankle Soc.
2019 Sep;23(3):121-130. 10.14193/jkfas.2019.23.3.121.
Regional Variation in the Incidence of Diabetes-Related Lower Limb Amputations and Its Relationship with the Regional Factors
- Affiliations
-
- 1Department of Orthopedic Surgery, Soon Chun Hyang University Seoul Hospital, Korea.
- 2Department of Orthopedic Surgery, Seoul Paik Hospital, Inje University College of Medicine, Korea.
- 3Department of Biostatistics, Soon Chun Hyang University Seoul Hospital, Seoul, Korea.
- 4Division of Genome Research, Center for Genome Science, Korea National Institute of Health, Cheongju, Korea.
- 5Department of Orthopedic Surgery, Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea. hohotoy@nate.com
- KMID: 2458014
- DOI: http://doi.org/10.14193/jkfas.2019.23.3.121
Abstract
- PURPOSE
To investigate the spatial distribution of diabetes-related lower limb amputations and analyze the relationship between the spatial distribution of diabetes-related lower limb amputations and regional factors.
MATERIALS AND METHODS
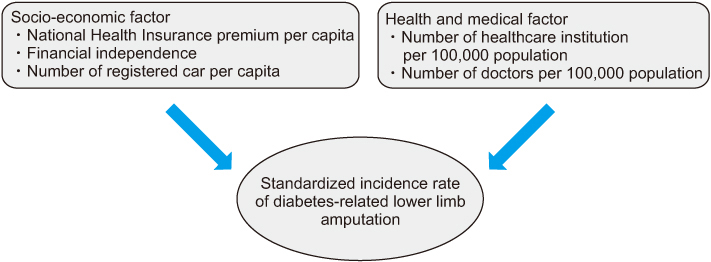
This study was performed based on the data from the Korean Health Insurance Review and Assessment Service, in 2016. The unit of analysis was the administrative districts of city·gun·gu. The dependent variable was the age- and sex-adjusted incidence of diabetes-related lower limb amputations and the regional variables were selected to represent two aspects: socioeconomic factors, and health and medical factors. Along with traditional ordinary least square (OLS) regression analysis, geographically weighted regression (GWR) was applied for spatial analysis.
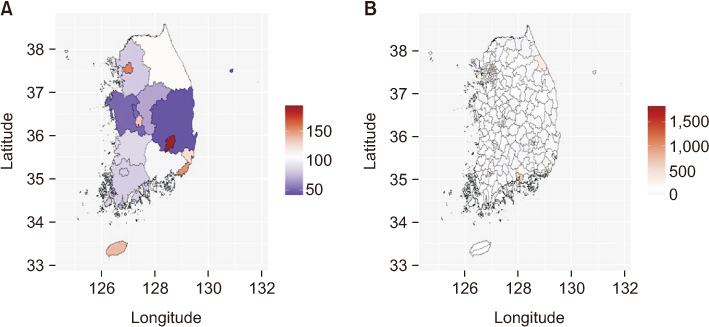
RESULTS
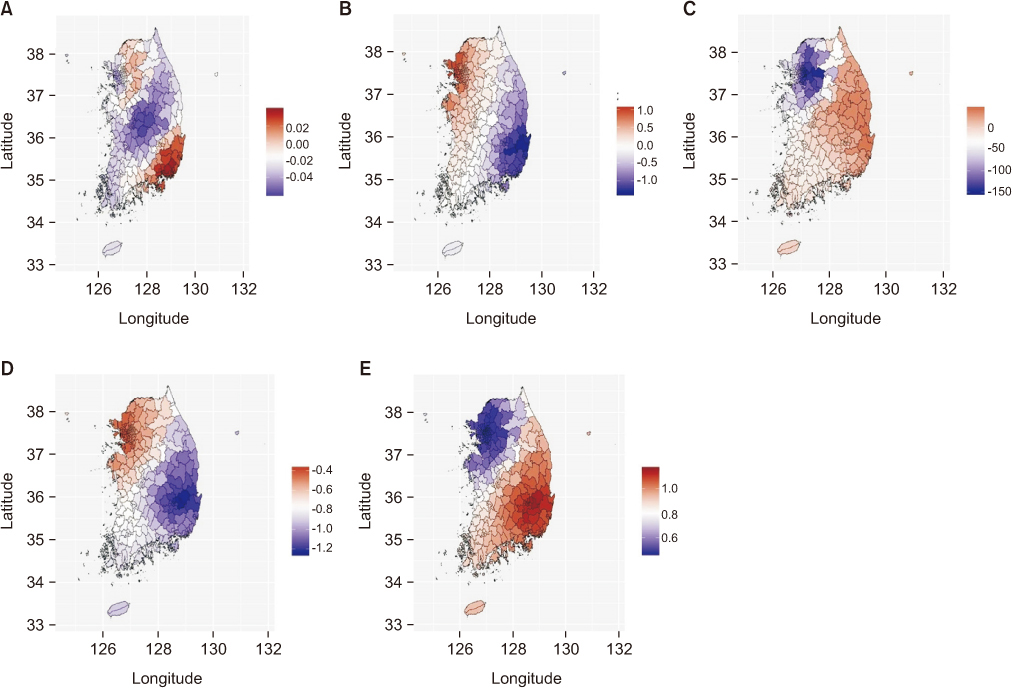
The age- and sex-adjusted incidence of diabetes-related lower limb amputation varied according to region. OLS regression showed that the incidence of diabetes-related lower limb amputation had significant relationships with the health and medical factors (number of healthcare institution and doctors per 100,000 population). In GWR, the effects of regional factors were not consistent.
CONCLUSION
The spatial distribution of the incidence of diabetes-related lower limb amputations and the effects of regional factors varied according to the regions. The regional characteristics should be considered when establishing health policy related to diabetic foot care.
Keyword
MeSH Terms
Figure
Reference
-
1. Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000; 321:405–412. DOI: 10.1136/bmj.321.7258.405.
Article2. Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014; 103:137–149. DOI: 10.1016/j.diabres.2013.11.002.
Article3. Jeffcoate WJ, Harding KG. Diabetic foot ulcers. Lancet. 2003; 361:1545–1551. DOI: 10.1016/S0140-6736(03)13169-8.
Article4. Mayfield JA, Reiber GE, Sanders LJ, Janisse D, Pogach LM. American Diabetes Association. Preventive foot care in diabetes. Diabetes Care. 2004; 27 Suppl 1:S63–S64. DOI: 10.2337/diacare.27.2007.s63.
Article5. Morbach S, Furchert H, Gröblinghoff U, Hoffmeier H, Kersten K, Klauke GT, et al. Long-term prognosis of diabetic foot patients and their limbs: amputation and death over the course of a decade. Diabetes Care. 2012; 35:2021–2027. DOI: 10.2337/dc12-0200.
Article6. Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010; 87:4–14. DOI: 10.1016/j.diabres.2009.10.007.
Article7. Kim JK, Jung YR, Kim KT, Shin CS, Lee KB. A report on diabetic foot and amputation from the Korean health insurance review & assessment service data. J Korean Foot Ankle Soc. 2017; 21:66–69. DOI: 10.14193/jkfas.2017.21.2.66.
Article8. Park SA, Ko SH, Lee SH, Cho JH, Moon SD, Jang SA, et al. Incidence of diabetic foot and associated risk factors in Type 2 diabetic patients: a five-year observational study. Korean Diabetes J. 2009; 33:315–323. DOI: 10.4093/kdj.2009.33.4.315.
Article9. Chung CH, Kim DJ, Kim J, Kim H, Kim H, Min KW, et al. Current status of diabetic foot in Korean patients using national health insurance database. J Korean Diabetes Assoc. 2006; 30:372–376. DOI: 10.4093/jkda.2006.30.5.372.
Article10. Bae JI, Won JH, Kim JS, Kim MD, Yoon CJ, Cho YK. Prevalence and current status of treatment of diabetic foot in South Korea. J Korean Soc Radiol. 2016; 74:169–176. DOI: 10.3348/jksr.2016.74.3.169.
Article11. Jeffcoate W, Barron E, Lomas J, Valabhji J, Young B. Using data to tackle the burden of amputation in diabetes. Lancet. 2017; 390:e29–e30. DOI: 10.1016/S0140-6736(17)32401-7.
Article12. Schulz AJ, Zenk S, Odoms-Young A, Hollis-Neely T, Nwankwo R, Lockett M, et al. Healthy eating and exercising to reduce diabetes: exploring the potential of social determinants of health frameworks within the context of community-based participatory diabetes prevention. Am J Public Health. 2005; 95:645–651. DOI: 10.2105/AJPH.2004.048256.
Article13. Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 2011; 40:804–818. DOI: 10.1093/ije/dyr029.
Article14. Dijkstra A, Janssen F, De Bakker M, Bos J, Lub R, Van Wissen LJ, et al. Using spatial analysis to predict health care use at the local level: a case study of type 2 diabetes medication use and its association with demographic change and socioeconomic status. PLoS One. 2013; 8:e72730. DOI: 10.1371/journal.pone.0072730.
Article15. Green C, Hoppa RD, Young TK, Blanchard JF. Geographic analysis of diabetes prevalence in an urban area. Soc Sci Med. 2003; 57:551–560. DOI: 10.1016/s0277-9536(02)00380-5.
Article16. Jo EK, Seo EW, Lee KS. Spatial distribution of diabetes prevalence rates and its relationship with the regional characteristics. Health Policy Manag. 2016; 26:30–38. DOI: 10.4332/KJHPA.2016.26.1.30.
Article17. Brown AF, Ettner SL, Piette J, Weinberger M, Gregg E, Shapiro MF, et al. Socioeconomic position and health among persons with diabetes mellitus: a conceptual framework and review of the literature. Epidemiol Rev. 2004; 26:63–77. DOI: 10.1093/epirev/mxh002.
Article18. Choi HW, Park JM, Kim HW, Kim YO. Identifying spatial distribution pattern of water quality in Masan Bay using spatial autocorrelation index and Pearson's r. Ocean Polar Res. 2007; 29:391–400. DOI: 10.4217/OPR.2007.29.4.391.
Article19. Seok HS, Kang SH. A Study on The regional variation factor of hypertension prevalence. Health Soc Welf Rev. 2013; 33:210–236. DOI: 10.15709/hswr.2013.33.3.210.
Article20. Lee KS, Choi YJ. Analysis on the relationships between the spatial distribution of primary care organizations and socio-demographic characteristics in a metropolitan city using the geographic weighted regression method. Product Rev. 2013; 27:193–214. DOI: 10.15843/kpapr.27.2.201306.193.
Article21. Brunsdon C, Fotheringham AS, Charlton ME. Geographically weighted regression: a method for exploring spatial nonstationarity. Geogr Anal. 1996; 28:281–298. DOI: 10.1111/j.1538-4632.1996.tb00936.x.
Article22. van Houtum WH, Lavery LA. Regional variation in the incidence of diabetes-related amputations in The Netherlands. Diabetes Res Clin Pract. 1996; 31:125–132.
Article23. Bocquier A, Cortaredona S, Nauleau S, Jardin M, Verger P. Prevalence of treated diabetes: geographical variations at the small-area level and their association with area-level characteristics. a multilevel analysis in Southeastern France. Diabetes Metab. 2011; 37:39–46. DOI: 10.1016/j.diabet.2010.07.004.
Article24. Connolly V, Unwin N, Sherriff P, Bilous R, Kelly W. Diabetes prevalence and socioeconomic status: a population based study showing increased prevalence of type 2 diabetes mellitus in deprived areas. J Epidemiol Community Health. 2000; 54:173–177. DOI: 10.1136/jech.54.3.173.
Article25. Ha KH, Kim DJ. Current status of managing diabetes mellitus in Korea. Korean J Intern Med. 2016; 31:845–850. DOI: 10.3904/kjim.2016.253.
Article26. Holman N, Young RJ, Jeffcoate WJ. Variation in the recorded incidence of amputation of the lower limb in England. Diabetologia. 2012; 55:1919–1925. DOI: 10.1007/s00125-012-2468-6.
Article27. Shaw J. Diabetes: regional variation in lower limb amputation incidence. Nat Rev Endocrinol. 2012; 8:386–388. DOI: 10.1038/nrendo.2012.78.
Article28. Margolis DJ, Hoffstad O, Nafash J, Leonard CE, Freeman CP, Hennessy S, et al. Location, location, location: geographic clustering of lower-extremity amputation among Medicare beneficiaries with diabetes. Diabetes Care. 2011; 34:2363–2367. DOI: 10.2337/dc11-0807.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Regional Variation in Accessing Regional Hospitals for Cancer Patients
- The Investigation of the Pain after the Orthotic Treatment in Adolescent Idiopathic Scoliosis
- Intravenous Regional Anesthesia
- Spatial Distribution of Diabetes Prevalence Rates and Its Relationship with the Regional Characteristics
- Analysing the Effects of Regional Factors on the Regional Variation of Obesity Rates Using the Geographically Weighted Regression