J Cardiovasc Imaging.
2019 Jul;27(3):200-211. 10.4250/jcvi.2019.27.e26.
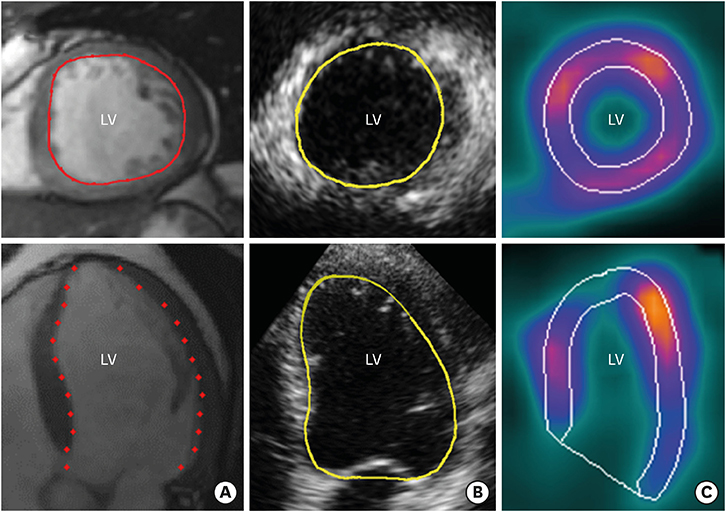
Comparison of Left Ventricular Volumes Measured by 3DE, SPECT and CMR
- Affiliations
-
- 1Department of Molecular Medicine and Surgery, Karolinska Institute, Stockholm, Sweden. jonas.jenner@ki.se
- 2Department of Clinical Physiology, Karolinska University Hospital, Stockholm, Sweden.
- 3Department of Cardiology, Karolinska University Hospital, Stockholm, Sweden.
- KMID: 2456855
- DOI: http://doi.org/10.4250/jcvi.2019.27.e26
Abstract
- BACKGROUND
Information regarding left ventricular (LV) volume and left ventricular ejection fraction (LVEF) has major diagnostic and prognostic value when assessing patients after ST-elevation myocardial infarction (STEMI). We aimed to investigate the agreement between measurement of LV volumes and LVEF by three-dimensional echocardiography (3DE), single-photon emission computed tomography (SPECT) and cardiac magnetic resonance (CMR) imaging in patients in a stable phase after STEMI.
METHODS
Fifteen patients underwent examinations by 3DE, SPECT and CMR three months after STEMI.
RESULTS
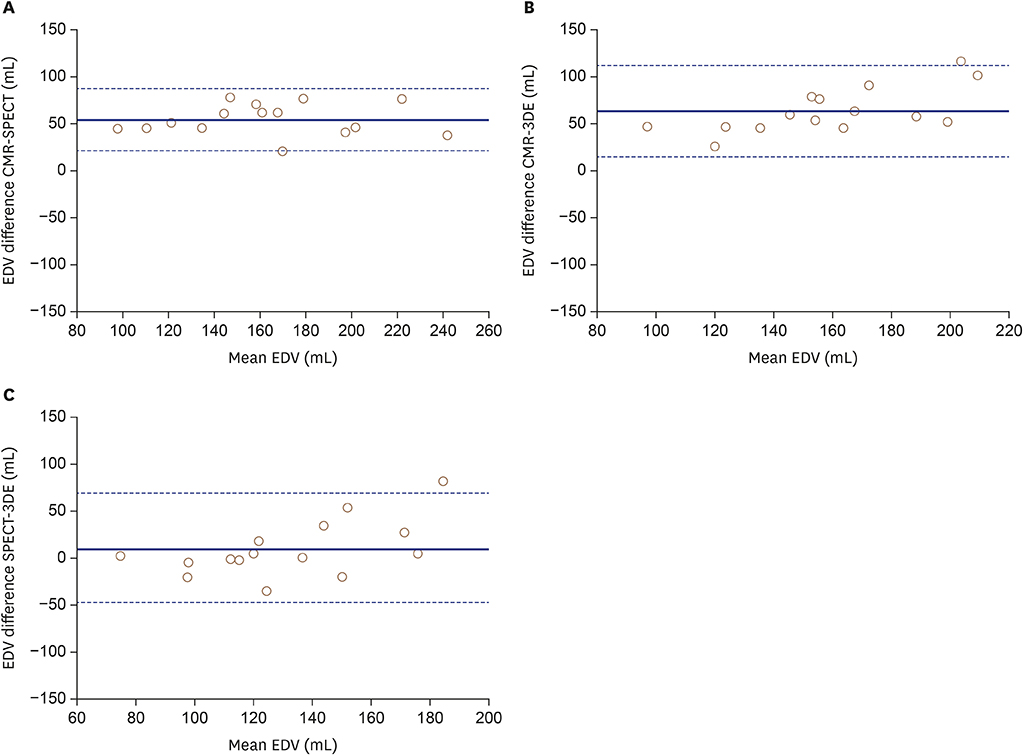
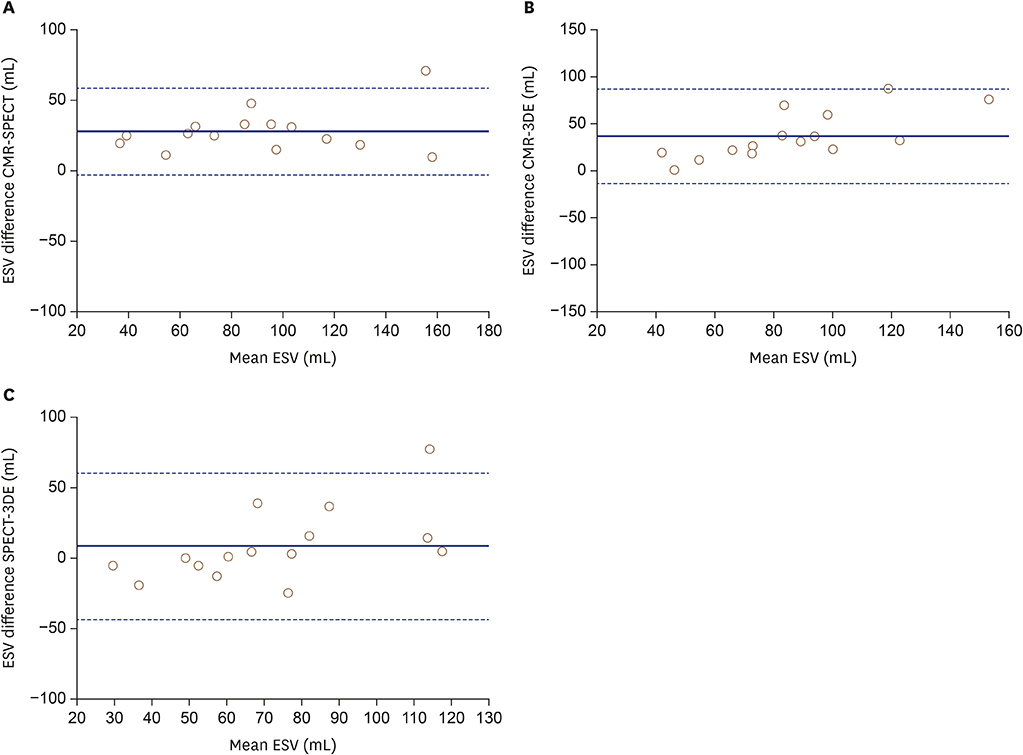
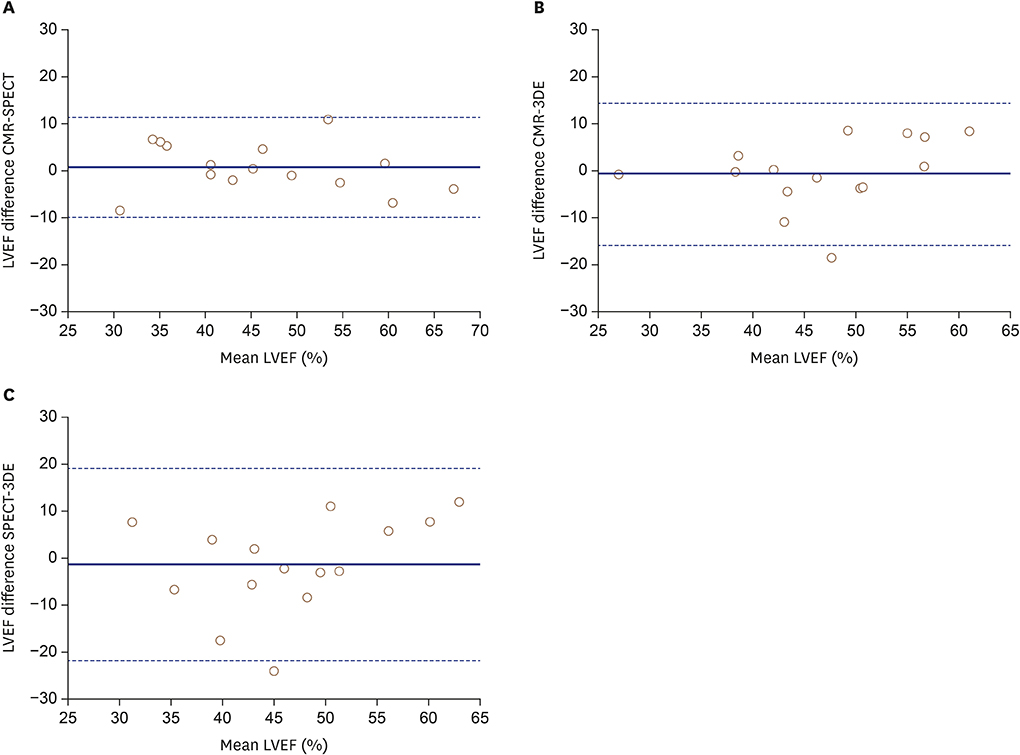
There was a significant bias in end-diastolic volume (EDV) measured by 3DE (-64 mL, p < 0.001) and SPECT (-55 mL, p < 0.001) compared with that measured by CMR. This was also the case for end-systolic volume (ESV) measured by 3DE (-36 mL, p < 0.001) and SPECT (-28 mL, p < 0.001). No significant differences were found between 3DE and SPECT for EDV or ESV. However, LVEF did not differ between the three methods. The agreement between all three methods was moderate (intra-class correlation coefficient [ICC] = 0.44) for LV volume and good for LVEF (ICC = 0.72).
CONCLUSIONS
LV volumes assessed by 3DE did not differ from SPECT, and despite larger LV volumes by CMR, measurements of LVEF showed good agreement between all three methods.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Evaluation of Left Ventricular Volume: Which method Is Your Choice?
Kyung Hee Lim, Sung-A Chang
J Cardiovasc Imaging. 2019;27(3):212-213. doi: 10.4250/jcvi.2019.27.e32.
Reference
-
1. Eriksson SV, Caidahl K, Hamsten A, de Faire U, Rehnqvist N, Lindvall K. Long-term prognostic significance of M mode echocardiography in young men after myocardial infarction. Br Heart J. 1995; 74:124–130.
Article2. Galderisi M, Lauer MS, Levy D. Echocardiographic determinants of clinical outcome in subjects with coronary artery disease (the Framingham Heart Study). Am J Cardiol. 1992; 70:971–976.
Article3. Funaro S, La Torre G, Madonna M, et al. Incidence, determinants, and prognostic value of reverse left ventricular remodelling after primary percutaneous coronary intervention: results of the Acute Myocardial Infarction Contrast Imaging (AMICI) multicenter study. Eur Heart J. 2009; 30:566–575.
Article4. Sheehan FH, Doerr R, Schmidt WG, et al. Early recovery of left ventricular function after thrombolytic therapy for acute myocardial infarction: an important determinant of survival. J Am Coll Cardiol. 1988; 12:289–300.
Article5. Carstensen S, Bonarjee VV, Berning J, Edner M, Nilsen DW, Caidahl K. Effects of early enalapril treatment on global and regional wall motion in acute myocardial infarction. CONSENSUS II Multi Echo Study Group. Am Heart J. 1995; 129:1101–1108.6. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018; 39:119–177.7. Pfeffer MA, Braunwald E, Moyé LA, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement trial. The SAVE Investigators. N Engl J Med. 1992; 327:669–677.8. Alfakih K, Reid S, Jones T, Sivananthan M. Assessment of ventricular function and mass by cardiac magnetic resonance imaging. Eur Radiol. 2004; 14:1813–1822.
Article9. Ioannidis JP, Trikalinos TA, Danias PG. Electrocardiogram-gated single-photon emission computed tomography versus cardiac magnetic resonance imaging for the assessment of left ventricular volumes and ejection fraction: a meta-analysis. J Am Coll Cardiol. 2002; 39:2059–2068.10. Mesquita CT, Pessoa MC, Vasconcelos PP, et al. Ventricular function following coronary artery bypass grafting: comparison between gated SPECT and cardiac magnetic resonance imaging. Arq Bras Cardiol. 2009; 92:327–333. 344–350. 357–363.11. Paul AK, Nabi HA. Gated myocardial perfusion SPECT: basic principles, technical aspects, and clinical applications. J Nucl Med Technol. 2004; 32:179–187. quiz 188-9.12. Pennell DJ. Ventricular volume and mass by CMR. J Cardiovasc Magn Reson. 2002; 4:507–513.
Article13. Jenkins C, Bricknell K, Chan J, Hanekom L, Marwick TH. Comparison of two- and three-dimensional echocardiography with sequential magnetic resonance imaging for evaluating left ventricular volume and ejection fraction over time in patients with healed myocardial infarction. Am J Cardiol. 2007; 99:300–306.
Article14. Kawai J, Tanabe K, Morioka S, Shiotani H. Rapid freehand scanning three-dimensional echocardiography: accurate measurement of left ventricular volumes and ejection fraction compared with quantitative gated scintigraphy. J Am Soc Echocardiogr. 2003; 16:110–115.
Article15. Lipiec P, Wejner-Mik P, Krzemińska-Pakuła M, et al. Gated 99mTc-MIBI single-photon emission computed tomography for the evaluation of left ventricular ejection fraction: comparison with three-dimensional echocardiography. Ann Nucl Med. 2008; 22:723–726.
Article16. Mannaerts HF, Van Der Heide JA, Kamp O, et al. Quantification of left ventricular volumes and ejection fraction using freehand transthoracic three-dimensional echocardiography: comparison with magnetic resonance imaging. J Am Soc Echocardiogr. 2003; 16:101–109.
Article17. Persson E, Carlsson M, Palmer J, Pahlm O, Arheden H. Evaluation of left ventricular volumes and ejection fraction by automated gated myocardial SPECT versus cardiovascular magnetic resonance. Clin Physiol Funct Imaging. 2005; 25:135–141.
Article18. Tighe DA, Rosetti M, Vinch CS, et al. Influence of image quality on the accuracy of real time three-dimensional echocardiography to measure left ventricular volumes in unselected patients: a comparison with gated-SPECT imaging. Echocardiography. 2007; 24:1073–1080.
Article19. Chan J, Jenkins C, Khafagi F, Du L, Marwick TH. What is the optimal clinical technique for measurement of left ventricular volume after myocardial infarction? A comparative study of 3-dimensional echocardiography, single photon emission computed tomography, and cardiac magnetic resonance imaging. J Am Soc Echocardiogr. 2006; 19:192–201.
Article20. Sörensson P, Saleh N, Bouvier F, et al. Effect of postconditioning on infarct size in patients with ST elevation myocardial infarction. Heart. 2010; 96:1710–1715.
Article21. Heiberg E, Sjögren J, Ugander M, Carlsson M, Engblom H, Arheden H. Design and validation of Segment--freely available software for cardiovascular image analysis. BMC Med Imaging. 2010; 10:1.
Article22. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174.
Article23. Chan YH. Biostatistics 104: correlational analysis. Singapore Med J. 2003; 44:614–619.24. Mor-Avi V, Jenkins C, Kühl HP, et al. Real-time 3-dimensional echocardiographic quantification of left ventricular volumes: multicenter study for validation with magnetic resonance imaging and investigation of sources of error. JACC Cardiovasc Imaging. 2008; 1:413–423.25. Mistry N, Halvorsen S, Hoffmann P, et al. Assessment of left ventricular function with magnetic resonance imaging vs. echocardiography, contrast echocardiography, and single-photon emission computed tomography in patients with recent ST-elevation myocardial infarction. Eur J Echocardiogr. 2010; 11:793–800.
Article26. Bavelaar-Croon CD, Kayser HW, van der Wall EE, et al. Left ventricular function: correlation of quantitative gated SPECT and MR imaging over a wide range of values. Radiology. 2000; 217:572–575.
Article27. Thorley PJ, Plein S, Bloomer TN, Ridgway JP, Sivananthan UM. Comparison of 99mTc tetrofosmin gated SPECT measurements of left ventricular volumes and ejection fraction with MRI over a wide range of values. Nucl Med Commun. 2003; 24:763–769.
Article28. Binder T. Three-dimensional echocardiography: principles and promises. J Clin Basic Cardiol. 2002; 5:149–152.29. Johri AM, Passeri JJ, Picard MH. Three dimensional echocardiography: approaches and clinical utility. Heart. 2010; 96:390–397.
Article30. Mor-Avi V, Lang RM. The use of real-time three-dimensional echocardiography for the quantification of left ventricular volumes and function. Curr Opin Cardiol. 2009; 24:402–409.
Article31. Thavendiranathan P, Grant AD, Negishi T, Plana JC, Popović ZB, Marwick TH. Reproducibility of echocardiographic techniques for sequential assessment of left ventricular ejection fraction and volumes: application to patients undergoing cancer chemotherapy. J Am Coll Cardiol. 2013; 61:77–84.32. Jenkins C, Bricknell K, Hanekom L, Marwick TH. Reproducibility and accuracy of echocardiographic measurements of left ventricular parameters using real-time three-dimensional echocardiography. J Am Coll Cardiol. 2004; 44:878–886.
Article33. Bellenger NG, Davies LC, Francis JM, Coats AJ, Pennell DJ. Reduction in sample size for studies of remodeling in heart failure by the use of cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2000; 2:271–278.
Article34. Soneson H, Ubachs JF, Ugander M, Arheden H, Heiberg E. An improved method for automatic segmentation of the left ventricle in myocardial perfusion SPECT. J Nucl Med. 2009; 50:205–213.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison between Three-Dimensional Navigator-Gated Whole-Heart MRI and Two-Dimensional Cine MRI in Quantifying Ventricular Volumes
- Comparison of Left and Right Ventricular Volume and Cardiac Output by MRI and Echocardiography
- Left Ventricular Ejection Fraetion Determmed by Cated Tl-201 Perfusion SPECT and Quantitative Software
- Principles and Clinical Applications of Feature-Tracking Cardiac Magnetic Resonance Imaging: A Literature Review
- Usefulness of Mitral Annular Systolic Velocity in the Detection of Left Ventricular Systolic Dysfunction: Comparison with Three Dimensional Echocardiographic Data