J Korean Neuropsychiatr Assoc.
2019 Aug;58(3):173-181. 10.4306/jknpa.2019.58.3.173.
Motivational Enhancement Therapy and Cognitive Behavioral Therapy for Alcohol Use Disorders
- Affiliations
-
- 1Department of Psychiatry, Chuncheon Sacred Heart Hospital, Hallym University Medical Center, Chuncheon, Korea. skmind@hallym.ac.kr
- KMID: 2456597
- DOI: http://doi.org/10.4306/jknpa.2019.58.3.173
Abstract
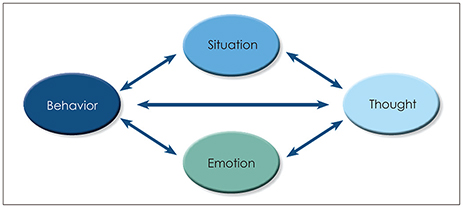
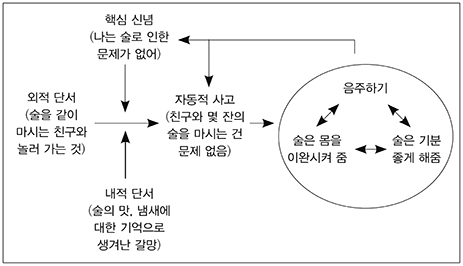
- Alcohol use disorder (AUD) has the highest prevalence and lowest treatment rate of all mental disorders in Korea. Over the last 30 years, there has been significant progress in the development and validation of cognitive behavioral treatments and motivational enhancement approaches for AUD. The goal of psychosocial treatment is to help patients control their urges to use alcohol and remain abstinent by preventing relapse. This review explored first, motivation enhancement therapy, which is an approach to help people with alcohol problems and improve their motivation for change, and second, cognitive behavioral theories for AUD, including practical therapeutic effects, treatment principles, and various treatment methods and techniques. These treatment modalities are particularly useful for patients with AUDs with insufficient or poor compliance. In addition, these treatment models, which enhance the motivation of patients with chronic psychiatric illness, including AUDs and improve the efficacy and effectiveness through a clear intervention approach to the targeted problems, have been transformed into various other forms. Recently, there have been many studies on various online platforms, such as web-based and virtual reality, which are easy to access, and these treatment models are likely to become more important in the psychiatric field in the future.
MeSH Terms
Figure
Reference
-
1. Miller WR. Motivational enhancement therapy manual: a clinical research guide for therapists treating individuals with alcohol abuse and dependence. DIANE Publishing;1995. p. 1–9.2. Gi SW. Recent psychosocial therapeutic approach on alcohol dependence. J Korean Neuropsychiatr Assoc. 2004; 43:646–651.3. Miller WR, Rollnick S. Motivational interviewing: preparing people to change addictive behavior. New York, NY: Guilford Press;1991.4. Prochaska JO, DiClemente CC. Toward a comprehensive model of change. In : Miller WR, Heather M, editors. Treating addictive behaviors: processes of change. Boston, MA: Springer;1986. p. 3–27.5. Bandura A. Self-efficacy mechanism in human agency. Am Psychol. 1982; 37:122–147.
Article6. McHugh RK, Hearon BA, Otto MW. Cognitive behavioral therapy for substance use disorders. Psychiatr Clin North Am. 2010; 33:511–525.
Article7. Carroll KM, Kosten TR, Rounsaville BJ. Choosing a behavioral therapy platform for pharmacotherapy of substance users. Drug Alcohol Depend. 2004; 75:123–134.
Article8. Magill M, Ray LA. Cognitive-behavioral treatment with adult alcohol and illicit drug users: a meta-analysis of randomized controlled trials. J Stud Alcohol Drugs. 2009; 70:516–527.
Article9. Carroll KM, Kiluk BD. Cognitive behavioral interventions for alcohol and drug use disorders: through the stage model and back again. Psychol Addict Behav. 2017; 31:847–861.
Article10. Carroll KM, Nich C, Ball SA, McCance E, Frankforter TL, Rounsaville BJ. One-year follow-up of disulfiram and psychotherapy for cocaine-alcohol users: sustained effects of treatment. Addiction. 2000; 95:1335–1349.
Article11. Carroll KM, Fenton LR, Ball SA, Nich C, Frankforter TL, Shi J, et al. Efficacy of disulfiram and cognitive behavior therapy in cocainedependent outpatients: a randomized placebo-controlled trial. Arch Gen Psychiatry. 2004; 61:264–272.
Article12. Wenzel A, Brown GK, Karlin BE. Cognitive behavioral therapy for depression in veterans and military servicemembers: therapist manual. Washington, DC: U.S. Department of Veterans Affairs;2011. p. 7.13. DeMarce JM, Gnys M, Raffa SD, Karlin BE. Cognitive behavioral therapy for substance use disorders among veterans: therapist manual. Washington, DC: U.S. Department of Veterans Affairs;2014.14. Wright FD, Beck AT, Newman CF, Liese BS. Cognitive therapy of substance abuse: theoretical rationale. NIDA Res Monogr. 1993; 137:123–146.
Article15. Dattilio FM, Hanna MA. Collaboration in cognitive-behavioral therapy. J Clin Psychol. 2012; 68:146–158.
Article16. Miller WR, Hester RK. Inpatient alcoholism treatment. Who benefits? Am Psychol. 1986; 41:794–805.
Article17. Otto MW, O'Cleirigh CM, Pollack MH. Attending to emotional cues for drug abuse: bridging the gap between clinic and home behaviors. Sci Pract Perspect. 2007; 3:48–56.
Article18. Bigelow GE, Silverman K. Theoretical and empirical foundations of contingency management treatments for drug abuse. In : Higgins ST, Silverman KE, editors. Motivating behavior change among illicit-drug abusers: research on contingency management interventions. Washington, DC: American Psychological Association;1999. p. 15–31.19. Monti PM, Rohsenow DJ, Swift RM, Gulliver SB, Colby SM, Mueller TI, et al. Naltrexone and cue exposure with coping and communication skills training for alcoholics: treatment process and 1-year outcomes. Alcohol Clin Exp Res. 2001; 25:1634–1647.
Article20. Rohsenow DJ, Monti PM, Rubonis AV, Gulliver SB, Colby SM, Binkoff JA, et al. Cue exposure with coping skills training and communication skills training for alcohol dependence: 6- and 12-month outcomes. Addiction. 2001; 96:1161–1174.
Article21. Otto MW, Safren SA, Pollack MH. Internal cue exposure and the treatment of substance use disorders: lessons from the treatment of panic disorder. J Anxiety Disord. 2004; 18:69–87.
Article22. Zvolensky MJ, Yartz AR, Gregor K, Gonzalez A, Bernstein A. Interoceptive exposure-based cessation intervention for smokers high in anxiety sensitivity: a case series. J Cogn Psychother. 2008; 22:346–365.
Article23. Reynolds B. A review of delay-discounting research with humans: relations to drug use and gambling. Behav Pharmacol. 2006; 17:651–667.
Article24. Hayes SC, Hofmann SG. Process based CBT: the science and core clinical competencies of cognitive behavioral therapy. Oakland, CA: Context Press;2018.25. Hayes SC, Strosahl KD. A practical guide to acceptance and commitment therapy. New York, NY: Springer;2004.26. Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: the process and practice of mindful change. 2nd ed. New York, NY: Guilford Press;2011.27. Byrne SP, Haber P, Baillie A, Costa DSJ, Fogliati V, Morley K. Systematic reviews of mindfulness and acceptance and commitment therapy for alcohol use disorder: should we be using third wave therapies? Alcohol Alcohol. 2019; 54:159–166.
Article28. Na E. Acceptance and commitment therapy. J Med Life Sci. 2018; 15:51–55.
Article29. The Ministry of Health and Welfare. The survey of mental disorders in Korea. Sejong: The Ministry of Health and Welfare;2017.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Strategy for Integrating Behavioral Therapy and Motivational Interviewing for Motivation Enhancement in Patients with Obesity
- Recent Psychosocial Therapeutic Approach on Alcohol Dependence
- Effect of Cognitive Behavioral and Motivational Enhancement Therapy Based Psychoeducation With Mindfulness Meditation on Hazardous Drinking and Motivation for Change
- An Integrative Review of Cognitive Behavioral Therapy for Patients with Alcohol Use Disorder
- The Application of the Cognitive Behavioral Therapy in Schizophrenia