Diabetes Metab J.
2019 Aug;43(4):530-538. 10.4093/dmj.2018.0111.
Impact of Longitudinal Changes in Metabolic Syndrome Status over 2 Years on 10-Year Incident Diabetes Mellitus
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea. kimjang713@gmail.com
- 2Center of Biomedical Data Science, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 3Division of Cardiology, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Division of Cardiology, Department of Internal Medicine, Hallym University Hangang Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- 5Division of Cardiology, Department of Internal Medicine, Gachon University Gil Medical Center, Gachon University College of Medicine, Incheon, Korea. kwangk@gilhospital.com
- KMID: 2455675
- DOI: http://doi.org/10.4093/dmj.2018.0111
Abstract
- BACKGROUND
Metabolic syndrome (MetS) is a known predictor of diabetes mellitus (DM), but whether longitudinal changes in MetS status modify the risk for DM remains unclear. We investigated whether changes in MetS status over 2 years modify the 10-year risk of incident DM.
METHODS
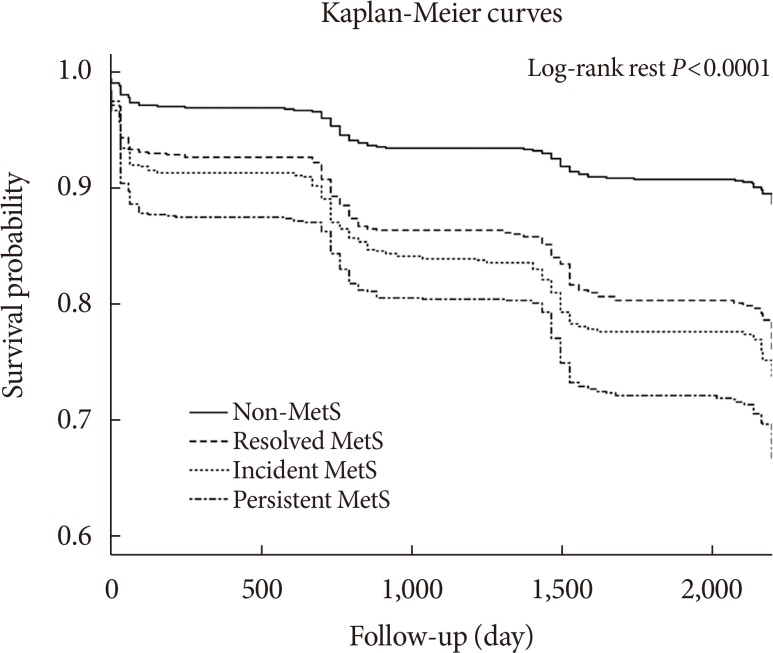
We analyzed data from 7,317 participants aged 40 to 70 years without DM at baseline, who took part in 2001 to 2011 Korean Genome Epidemiology Study. Subjects were categorized into four groups based on repeated longitudinal assessment of MetS status over 2 years: non-MetS, resolved MetS, incident MetS, and persistent MetS. The hazard ratio (HR) of new-onset DM during 10 years was calculated in each group using Cox models.
RESULTS
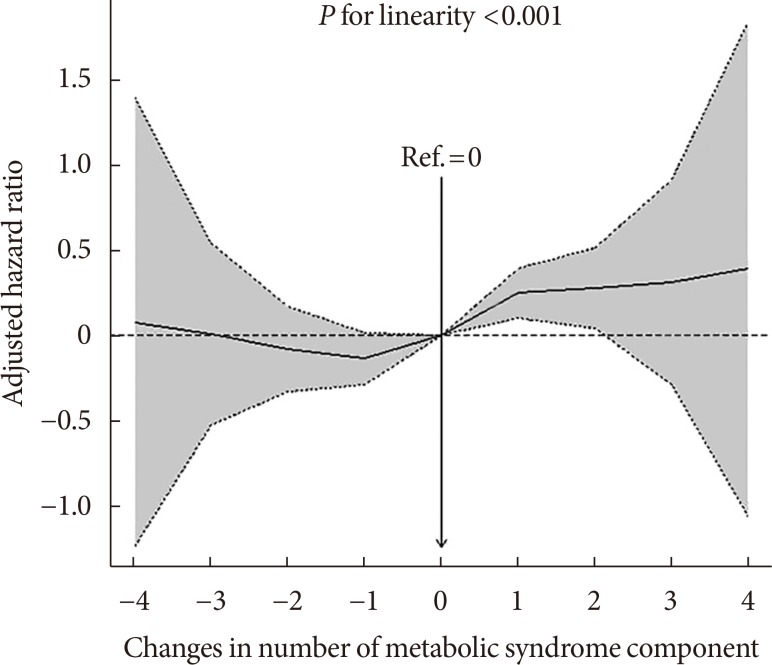
During the 10-year follow-up, 1,099 participants (15.0%) developed DM. Compared to the non-MetS group, the fully adjusted HRs for new-onset DM were 1.28 (95% confidence interval [CI], 0.92 to 1.79) in the resolved MetS group, 1.75 (95% CI, 1.30 to 2.37) in the incident MetS group, and 1.98 (95% CI, 1.50 to 2.61) in the persistent MetS group (P for trend <0.001). The risk of DM in subjects with resolved MetS was significantly attenuated compared to those with persistent MetS over 2 years. In addition, the adjusted HR for 10-year developing DM gradually increased as the number of MetS components increased 2 years later.
CONCLUSION
We found that discrete longitudinal changes pattern in MetS status over 2 years associated with 10-year risk of DM. These findings suggest that monitoring change of MetS status and controlling it in individuals may be important for risk prediction of DM.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Metabolic Syndrome Severity Score for Predicting Cardiovascular Events: A Nationwide Population-Based Study from Korea
Yo Nam Jang, Jun Hyeok Lee, Jin Sil Moon, Dae Ryong Kang, Seong Yong Park, Jerim Cho, Jang-Young Kim, Ji Hye Huh
Diabetes Metab J. 2021;45(4):569-577. doi: 10.4093/dmj.2020.0103.The efficacy and safety of
Dendropanax morbifera leaf extract on the metabolic syndrome: a 12-week, placebo controlled, double blind, and randomized controlled trial
Ji Eun Jun, You-Cheol Hwang, Kyu Jeung Ahn, Ho Yeon Chung, Se Young Choung, In-Kyung Jeong
Nutr Res Pract. 2022;16(1):60-73. doi: 10.4162/nrp.2022.16.1.60.
Reference
-
1. Kahn R, Buse J, Ferrannini E, Stern M. American Diabetes Association. European Association for the Study of Diabetes. The metabolic syndrome: time for a critical appraisal: joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2005; 28:2289–2304. PMID: 16123508.
Article2. Aguilar M, Bhuket T, Torres S, Liu B, Wong RJ. Prevalence of the metabolic syndrome in the United States, 2003-2012. JAMA. 2015; 313:1973–1974. PMID: 25988468.
Article3. Zuo H, Shi Z, Hu X, Wu M, Guo Z, Hussain A. Prevalence of metabolic syndrome and factors associated with its components in Chinese adults. Metabolism. 2009; 58:1102–1108. PMID: 19481771.
Article4. Lim S, Shin H, Song JH, Kwak SH, Kang SM, Won Yoon J, Choi SH, Cho SI, Park KS, Lee HK, Jang HC, Koh KK. Increasing prevalence of metabolic syndrome in Korea: the Korean National Health and Nutrition Examination Survey for 1998-2007. Diabetes Care. 2011; 34:1323–1328. PMID: 21505206.5. Dekker JM, Girman C, Rhodes T, Nijpels G, Stehouwer CD, Bouter LM, Heine RJ. Metabolic syndrome and 10-year cardiovascular disease risk in the Hoorn Study. Circulation. 2005; 112:666–673. PMID: 16061755.
Article6. Vinluan CM, Zreikat HH, Levy JR, Cheang KI. Comparison of different metabolic syndrome definitions and risks of incident cardiovascular events in the elderly. Metabolism. 2012; 61:302–309. PMID: 21840552.
Article7. Hanley AJ, Karter AJ, Williams K, Festa A, D'Agostino RB Jr, Wagenknecht LE, Haffner SM. Prediction of type 2 diabetes mellitus with alternative definitions of the metabolic syndrome: the Insulin Resistance Atherosclerosis Study. Circulation. 2005; 112:3713–3721. PMID: 16344402.8. Chen W, Srinivasan SR, Li S, Xu J, Berenson GS. Clustering of long-term trends in metabolic syndrome variables from childhood to adulthood in Blacks and Whites: the Bogalusa Heart Study. Am J Epidemiol. 2007; 166:527–533. PMID: 17573336.
Article9. Wilson PW, D'Agostino RB, Parise H, Sullivan L, Meigs JB. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation. 2005; 112:3066–3072. PMID: 16275870.
Article10. Ohnishi H, Saitoh S, Akasaka H, Furukawa T, Mori M, Miura T. Impact of longitudinal status change in metabolic syndrome defined by two different criteria on new onset of type 2 diabetes in a general Japanese population: the Tanno-Sobetsu Study. Diabetol Metab Syndr. 2016; 8:64. PMID: 27602060.
Article11. Walden P, Jiang Q, Jackson EA, Oral EA, Weintraub MS, Rubenfire M. Assessing the incremental benefit of an extended duration lifestyle intervention for the components of the metabolic syndrome. Diabetes Metab Syndr Obes. 2016; 9:177–184. PMID: 27330320.
Article12. Akbaraly TN, Kivimaki M, Shipley MJ, Tabak AG, Jokela M, Virtanen M, Marmot MG, Ferrie JE, Singh-Manoux A. Metabolic syndrome over 10 years and cognitive functioning in late midlife: the Whitehall II study. Diabetes Care. 2010; 33:84–89. PMID: 19837794.13. Cho YS, Go MJ, Kim YJ, Heo JY, Oh JH, Ban HJ, Yoon D, Lee MH, Kim DJ, Park M, Cha SH, Kim JW, Han BG, Min H, Ahn Y, Park MS, Han HR, Jang HY, Cho EY, Lee JE, Cho NH, Shin C, Park T, Park JW, Lee JK, Cardon L, Clarke G, McCarthy MI, Lee JY, Lee JK, Oh B, Kim HL. A large-scale genome-wide association study of Asian populations uncovers genetic factors influencing eight quantitative traits. Nat Genet. 2009; 41:527–534. PMID: 19396169.
Article14. Lim S, Jang HC, Lee HK, Kimm KC, Park C, Cho NH. A rural-urban comparison of the characteristics of the metabolic syndrome by gender in Korea: the Korean Health and Genome Study (KHGS). J Endocrinol Invest. 2006; 29:313–319. PMID: 16699297.
Article15. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985; 28:412–419. PMID: 3899825.16. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC Jr, Spertus JA, Costa F. American Heart Association. National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005; 112:2735–2752. PMID: 16157765.17. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014; 37(Suppl 1):S81–S90. PMID: 24357215.18. Ceriello A. Hypothesis: the “metabolic memory”, the new challenge of diabetes. Diabetes Res Clin Pract. 2009; 86(Suppl 1):S2–S6. PMID: 20115927.
Article19. Ihnat MA, Thorpe JE, Kamat CD, Szabo C, Green DE, Warnke LA, Lacza Z, Cselenyak A, Ross K, Shakir S, Piconi L, Kaltreider RC, Ceriello A. Reactive oxygen species mediate a cellular ‘memory’ of high glucose stress signalling. Diabetologia. 2007; 50:1523–1531. PMID: 17508197.
Article20. Itoh H, Kurihara I, Miyashita K, Tanaka M. Clinical significance of ‘cardiometabolic memory’: a systematic review of randomized controlled trials. Hypertens Res. 2017; 40:526–534. PMID: 28100921.
Article21. Action to Control Cardiovascular Risk in Diabetes Follow-On (ACCORDION) Eye Study Group and the Action to Control Cardiovascular Risk in Diabetes Follow-On (ACCORDION) Study Group. Persistent effects of intensive glycemic control on retinopathy in type 2 diabetes in the action to control cardiovascular risk in diabetes (ACCORD) follow-on study. Diabetes Care. 2016; 39:1089–1100. PMID: 27289122.22. Wong MG, Perkovic V, Chalmers J, Woodward M, Li Q, Cooper ME, Hamet P, Harrap S, Heller S, MacMahon S, Mancia G, Marre M, Matthews D, Neal B, Poulter N, Rodgers A, Williams B, Zoungas S. ADVANCE-ON Collaborative Group. Long-term benefits of intensive glucose control for preventing end-stage kidney disease: ADVANCE-ON. Diabetes Care. 2016; 39:694–700. PMID: 27006512.
Article23. Bosch J, Lonn E, Pogue J, Arnold JM, Dagenais GR, Yusuf S. HOPE/HOPE-TOO Study Investigators. Long-term effects of ramipril on cardiovascular events and on diabetes: results of the HOPE study extension. Circulation. 2005; 112:1339–1346. PMID: 16129815.24. Lindstrom J, Peltonen M, Eriksson JG, Ilanne-Parikka P, Aunola S, Keinänen-Kiukaanniemi S, Uusitupa M, Tuomilehto J. Finnish Diabetes Prevention Study (DPS). Improved lifestyle and decreased diabetes risk over 13 years: long-term follow-up of the randomised Finnish Diabetes Prevention Study (DPS). Diabetologia. 2013; 56:284–293. PMID: 23093136.25. Li G, Zhang P, Wang J, Gregg EW, Yang W, Gong Q, Li H, Li H, Jiang Y, An Y, Shuai Y, Zhang B, Zhang J, Thompson TJ, Gerzoff RB, Roglic G, Hu Y, Bennett PH. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet. 2008; 371:1783–1789. PMID: 18502303.
Article26. Sumner AE, Cowie CC. Ethnic differences in the ability of triglyceride levels to identify insulin resistance. Atherosclerosis. 2008; 196:696–703. PMID: 17254586.
Article27. Walker SE, Gurka MJ, Oliver MN, Johns DW, DeBoer MD. Racial/ethnic discrepancies in the metabolic syndrome begin in childhood and persist after adjustment for environmental factors. Nutr Metab Cardiovasc Dis. 2012; 22:141–148. PMID: 20708390.
Article28. Gaillard T, Schuster D, Osei K. Differential impact of serum glucose, triglycerides, and high-density lipoprotein cholesterol on cardiovascular risk factor burden in nondiabetic, obese African American women: implications for the prevalence of metabolic syndrome. Metabolism. 2010; 59:1115–1123. PMID: 20051282.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Type 2 diabetes mellitus and metabolic syndrome
- Metabolic Syndrome and Male Infertility
- Impact of Visceral Obesity on the Risk of Incident Metabolic Syndrome in Metabolically Healthy Normal Weight and Overweight Groups: A Longitudinal Cohort Study in Korea
- Serum Calcium and the Risk of Incident Metabolic Syndrome: A 4.3-Year Retrospective Longitudinal Study
- On the Severity of Carpal Tunnel Syndrome: Diabetes or Metabolic Syndrome