Clin Exp Otorhinolaryngol.
2019 Aug;12(3):287-293. 10.21053/ceo.2018.01165.
Comparison Between Endoscopic Prelacrimal Medial Maxillectomy and Caldwell-Luc Approach for Benign Maxillary Sinus Tumors
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. kkam97@gmail.com
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Najran University, Najran, Saudi Arabia.
- KMID: 2455370
- DOI: http://doi.org/10.21053/ceo.2018.01165
Abstract
OBJECTIVES
Endoscopic prelacrimal medial maxillectomy (EPMM) was previously reported to treat maxillary inverted papilloma. This study aimed to compare prelacrimal recess approach with the conventional Caldwell-Luc approach (CLA) to remove benign maxillary sinus tumors and to evaluate the usefulness of this approach based on our experience.
METHODS
Ten patients who underwent EPMM at our hospital from January 2013 to December 2017 were reviewed. We also reviewed 30 patients who underwent benign maxillary sinus tumor resection via CLA during the same period. From medical records, postoperative pathological results, complications due to surgery, and recurrence rate were evaluated.
RESULTS
There were eight inverted papilloma, one ameloblastoma, and one ossifying fibroma in the EPMM group. In the CLA group, all 30 cases were inverted papilloma. There were no cases of failure at gross total removal during surgery, and no recurrences were observed during follow-up in either groups. Mean follow-up period was 13.0 months in CLA group and 10.8 months in EPMM group. Regarding postoperative complications, 11 patients of the CLA group (37%) and three patients of the EPMM group (30%) had numbness around the cheek and upper lip area after surgery (P=0.715). In the CLA group, there were eight patients who had numbness lasting more than 3 months after surgery, and two patients had numbness for more than 1 year. However, facial numbness disappeared within 3 months in all patients in the EPMM group, in which epiphora was not observed.
CONCLUSION
EPMM is the effective surgical approach for resecting benign maxillary sinus tumor compared with CLA. Although facial numbness was reported in EPMM, the duration of numbness was shorter than CLA.
Keyword
MeSH Terms
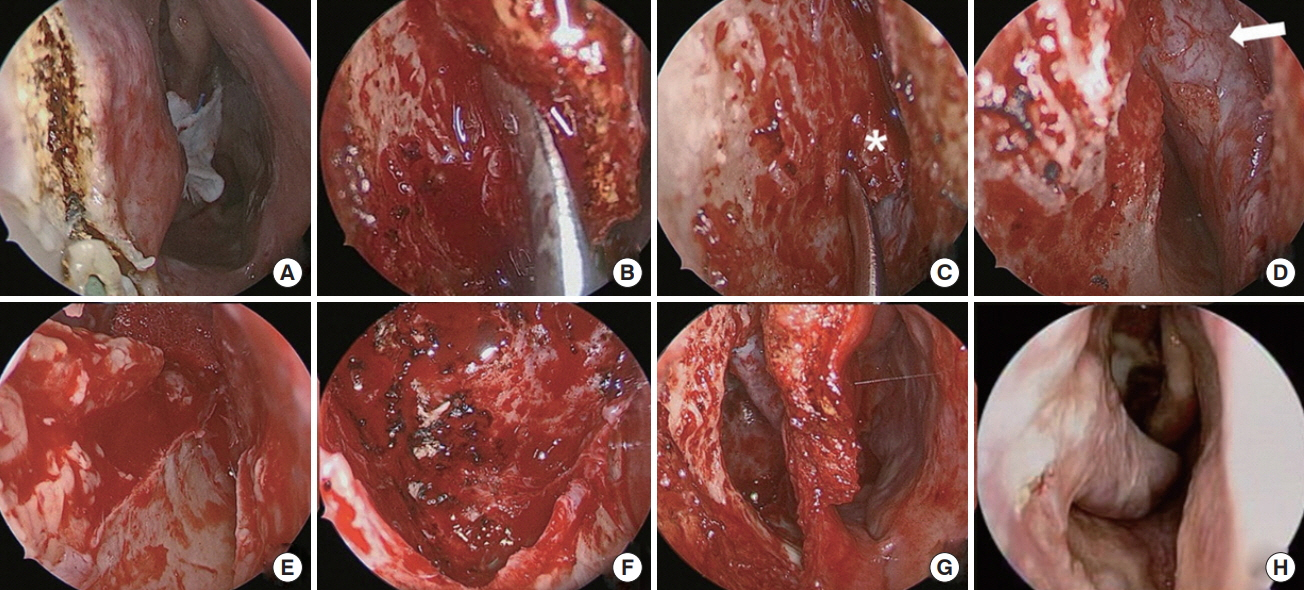
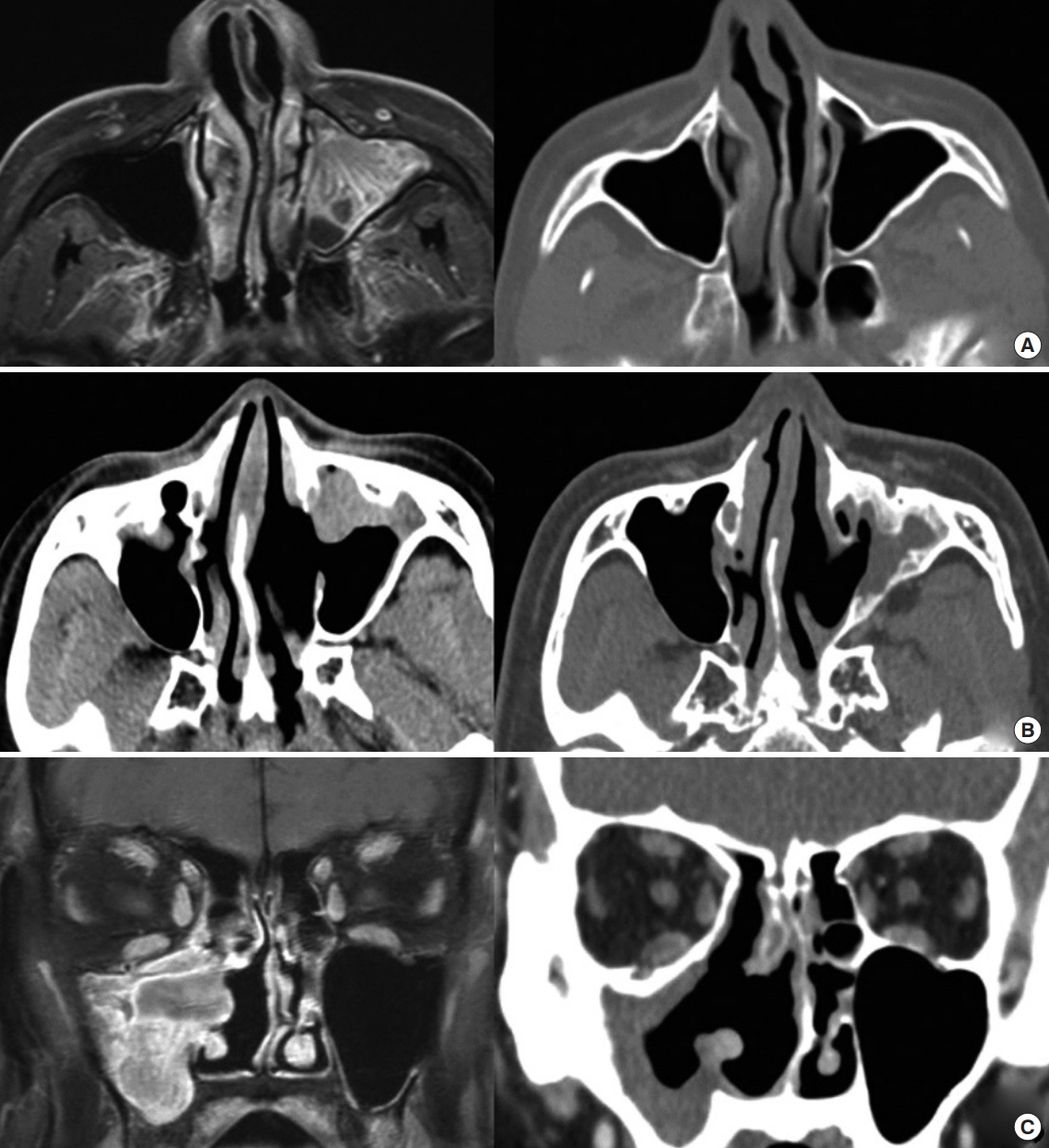
Figure
Cited by 2 articles
-
Comparison of Surgical Outcomes for Treatment of Maxillary Sinus Inverted Papilloma: Endoscopic Prelacrimal Recess Approach versus Caldwell-Luc Approach
Yeong Jun Park, Byung Whoo Park, Tae Kyung Suh, Mi Ra Kim, Sang-Yeon Kim, Shin Hye Kim, Moo Jin Baek, Myoungjoo Kang, Yong Wan Kim
Korean J Otorhinolaryngol-Head Neck Surg. 2021;64(3):161-168. doi: 10.3342/kjorl-hns.2020.00031.The Prelacrimal Recess Approach: A Review of Surgical Applications, Outcomes, and Recent Advances
Yeon Hee Im, Soo Whan Kim, Chan-Soon Park, Dong-Hyun Kim
J Rhinol. 2025;32(1):17-27. doi: 10.18787/jr.2024.00041.
Reference
-
1. Kennedy DW. Functional endoscopic sinus surgery: technique. Arch Otolaryngol. 1985; Oct. 111(10):643–9.
Article2. Ungari C, Riccardi E, Reale G, Agrillo A, Rinna C, Mitro V, et al. Management and treatment of sinonasal inverted papilloma. Ann Stomatol (Roma). 2016; Feb. 6(3-4):87–90.
Article3. Robinson S, Wormald PJ. Patterns of innervation of the anterior maxilla: a cadaver study with relevance to canine fossa puncture of the maxillary sinus. Laryngoscope. 2005; Oct. 115(10):1785–8.
Article4. Sathananthar S, Nagaonkar S, Paleri V, Le T, Robinson S, Wormald PJ. Canine fossa puncture and clearance of the maxillary sinus for the severely diseased maxillary sinus. Laryngoscope. 2005; Jun. 115(6):1026–9.
Article5. Robinson SR, Baird R, Le T, Wormald PJ. The incidence of complications after canine fossa puncture performed during endoscopic sinus surgery. Am J Rhinol. 2005; Mar-Apr. 19(2):203–6.
Article6. Ferekidis E, Tzounakos P, Kandiloros D, Kaberos A, Adamopoulos G. Modifications of the Caldwell-Luc procedure for the prevention of post-operative sensitivity disorders. J Laryngol Otol. 1996; Mar. 110(3):228–31.
Article7. Zhou B, Han DM, Cui SJ, Huang Q, Wang CS. Intranasal endoscopic prelacrimal recess approach to maxillary sinus. Chin Med J (Engl). 2013; Apr. 126(7):1276–80.8. Zhou B, Han DM, Cui SJ, Huang Q, Wei YX, Liu HC, et al. Endoscopic nasal lateral wall dissection approach to maxillary sinus. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2007; Oct. 42(10):743–8.9. Lin YT, Lin CF, Yeh TH. Application of the endoscopic prelacrimal recess approach to the maxillary sinus in unilateral maxillary diseases. Int Forum Allergy Rhinol. 2018; Apr. 8(4):530–6.
Article10. Zhou B, Huang Q, Shen PH, Cui SJ, Wang CS, Li YC, et al. The intranasal endoscopic removal of schwannoma of the pterygopalatine and infratemporal fossae via the prelacrimal recess approach. J Neurosurg. 2016; Apr. 124(4):1068–73.
Article11. Chen HH, Wang F, Weng BQ, Wang SQ. Endoscopic prelacrimal recess approach adjunct with vestibular sulcus incision: case report of a minimally invasive access to remove infratemporal fossa tumor. Eur Arch Otorhinolaryngol. 2015; Jul. 272(7):1813–7.
Article12. Ojiri H, Ujita M, Tada S, Fukuda K. Potentially distinctive features of sinonasal inverted papilloma on MR imaging. AJR Am J Roentgenol. 2000; Aug. 175(2):465–8.
Article13. Michaels L. Benign mucosal tumors of the nose and paranasal sinuses. Semin Diagn Pathol. 1996; May. 13(2):113–7.14. Lee DK, Chung SK, Dhong HJ, Kim HY, Kim HJ, Bok KH. Focal hyperostosis on CT of sinonasal inverted papilloma as a predictor of tumor origin. AJNR Am J Neuroradiol. 2007; Apr. 28(4):618–21.15. Hosemann W, Scotti O, Bentzien S. Evaluation of telescopes and forceps for endoscopic transnasal surgery on the maxillary sinus. Am J Rhinol. 2003; Sep-Oct. 17(5):311–6.
Article16. Robey A, O’Brien EK, Leopold DA. Assessing current technical limitations in the small-hole endoscopic approach to the maxillary sinus. Am J Rhinol Allergy. 2010; Sep-Oct. 24(5):396–401.
Article17. Feldmann H. The maxillary sinus and its illness in the history of rhinology: images from the history of otorhinolaryngology, highlighted by instruments from the collection of the German Medical History Museum in Ingolstadt. Laryngorhinootologie. 1998; Oct. 77(10):587–95.18. Osguthorpe JD, Weisman RA. ‘Medial maxillectomy’ for lateral nasal wall neoplasms. Arch Otolaryngol Head Neck Surg. 1991; Jul. 117(7):751–6.
Article19. Wormald PJ, Ooi E, van Hasselt CA, Nair S. Endoscopic removal of sinonasal inverted papilloma including endoscopic medial maxillectomy. Laryngoscope. 2003; May. 113(5):867–73.
Article20. Morrissey DK, Wormald PJ, Psaltis AJ. Prelacrimal approach to the maxillary sinus. Int Forum Allergy Rhinol. 2016; Feb. 6(2):214–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of Postoperative Mucocele of the Maxillary Sinus through Endoscopic Approach
- A Case of Removal of Medial Maxillary Intraosseous Hemangioma through an Intranasal Endoscopic Prelacrimal Recess Approach
- Comparison of Surgical Outcomes for Treatment of Maxillary Sinus Inverted Papilloma: Endoscopic Prelacrimal Recess Approach versus Caldwell-Luc Approach
- Treatment Results of 111 Cases of Antrochoanal Polyp
- Two Cases of Pneumocele of Maxillary Sinus