Anesth Pain Med.
2019 Jul;14(3):316-321. 10.17085/apm.2019.14.3.316.
The change of stroke volume variation during thoracotomy or one lung ventilation
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Chonbuk National University Medical School and Hospital, Jeonju, Korea. aneduke@jbnu.ac.kr
- KMID: 2454817
- DOI: http://doi.org/10.17085/apm.2019.14.3.316
Abstract
- BACKGROUND
Stroke volume variation (SVV) is based on cyclic changes of intrathoracic pressure during respiratory cycle. Thoracotomy and one-lung ventilation (OLV) can lead to changes in airway and intrathoracic pressure. The aim of this study was to determine whether thoracotomy and converting from two lung ventilation to OLV could affect SVV values.
METHODS
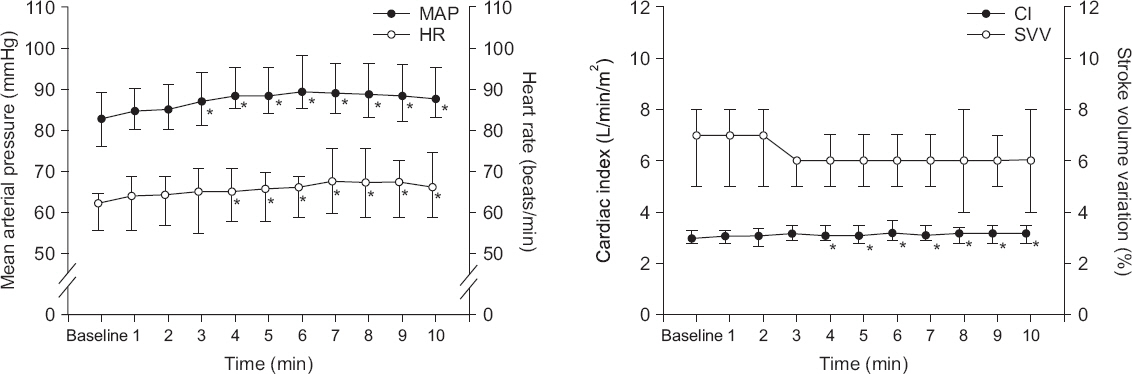
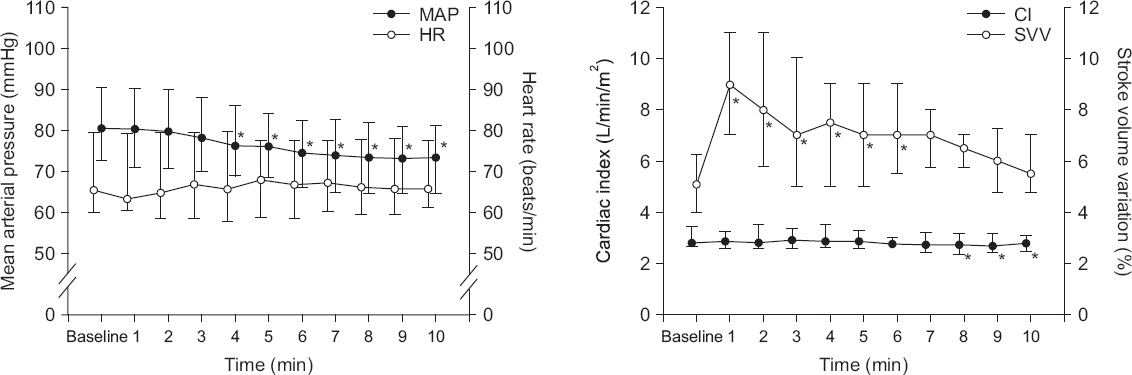
Thirty patients who were scheduled for pulmonary lobectomy or pneumonectomy requiring OLV were enrolled. Induction and maintenance of anesthesia were performed with propofol and remifentanil via total intravenous anesthesia. Hemodynamic variables including mean arterial pressure (MAP), heart rate (HR), cardiac index (CI), and SVV were measured at intervals of 1 min for 10 min after thoracotomy and OLV, respectively.
RESULTS
MAP and HR increased from baseline at intervals between 3 and 10 min and between 4 and 10 min after thoracotomy, respectively (P < 0.001). CI increased between 4 and 10 min (P < 0.001). SVV did not change for 10 min after thoracotomy. After OLV, MAP decreased between 4 and 10 min (P = 0.112). SVV was the highest at 1 min after OLV. It returned to the baseline value at 7 min (P < 0.001). CI decreased between 8 and 10 min after OLV (P < 0.001).
CONCLUSIONS
SVV can increase after OLV temporarily. Transient increase of SVV may be considered when fluid responsiveness is predicted by SVV during early period after OLV.
Keyword
MeSH Terms
Figure
Reference
-
1. Lorsomradee S, Lorsomradee S, Cromheecke S, De Hert SG. Uncalibrated arterial pulse contour analysis versus continuous thermodilution technique:effects of alterations in arterial waveform. J Cardiothorac Vasc Anesth. 2007; 21:636–43. DOI: 10.1053/j.jvca.2007.02.003. PMID: 17905266.2. Della Rocca G, Costa MG, Chiarandini P, Bertossi G, Lugano M, Pompei L, et al. Arterial pulse cardiac output agreement with thermodilution in patients in hyperdynamic conditions. J Cardiothorac Vasc Anesth. 2008; 22:681–7. DOI: 10.1053/j.jvca.2008.02.021. PMID: 18922423.3. Breukers RM, Sepehrkhouy S, Spiegelenberg SR, Groeneveld AB. Cardiac output measured by a new arterial pressure waveform analysis method without calibration compared with thermodilution after cardiac surgery. J Cardiothorac Vasc Anesth. 2007; 21:632–5. DOI: 10.1053/j.jvca.2007.01.001. PMID: 17905265.4. Manecke GR Jr, Auger WR. Cardiac output determination from the arterial pressure wave:clinical testing of a novel algorithm that does not require calibration. J Cardiothorac Vasc Anesth. 2007; 21:3–7. DOI: 10.1053/j.jvca.2006.08.004. PMID: 17289472.5. Marik PE. Techniques for assessment of intravascular volume in critically ill patients. J Intensive Care Med. 2009; 24:329–37. DOI: 10.1177/0885066609340640. PMID: 19648183.6. Jang EA, Lee SE, Choi JI, Cho SY. Changes in the hemodynamic parameters between the prone and supine positions measured by an arterial pulse contour cardiac output monitoring system. Anesth Pain Med. 2015; 10:291–4. DOI: 10.17085/apm.2015.10.4.291.7. Kim HJ, Jung YS, Kim JH, Bahk JH, Gil NS, Lim YJ, et al. Predictability of passive leg raising test on anesthesia-induced hypotension in patients undergoing cardiac surgery. Anesth Pain Med. 2013; 8:104–11.8. Cannesson M, Musard H, Desebbe O, Boucau C, Simon R, Hénaine R, et al. The ability of stroke volume variations obtained with Vigileo/FloTrac system to monitor fluid responsiveness in mechanically ventilated patients. Anesth Analg. 2009; 108:513–7. DOI: 10.1213/ane.0b013e318192a36b. PMID: 19151280.9. Biais M, Nouette-Gaulain K, Roullet S, Quinart A, Revel P, Sztark F. A comparison of stroke volume variation measured by Vigileo/ FloTrac system and aortic Doppler echocardiography. Anesth Analg. 2009; 109:466–9. DOI: 10.1213/ane.0b013e3181ac6dac. PMID: 19608819.10. Biais M, Nouette-Gaulain K, Quinart A, Roullet S, Revel P, Sztark F. Uncalibrated stroke volume variations are able to predict the hemodynamic effects of positive end-expiratory pressure in patients with acute lung injury or acute respiratory distress syndrome after liver transplantation. Anesthesiology. 2009; 111:855–62. DOI: 10.1097/ALN.0b013e3181b27fb2. PMID: 19741498.11. Biais M, Nouette-Gaulain K, Cottenceau V, Revel P, Sztark F. Uncalibrated pulse contour-derived stroke volume variation predicts fluid responsiveness in mechanically ventilated patients undergoing liver transplantation. Br J Anaesth. 2008; 101:761–8. DOI: 10.1093/bja/aen277. PMID: 18852114.12. Benes J, Chytra I, Altmann P, Hluchy M, Kasal E, Svitak R, et al. Intraoperative fluid optimization using stroke volume variation in high risk surgical patients:results of prospective randomized study. Crit Care. 2010; 14:R118. DOI: 10.1186/cc9070. PMID: 20553586. PMCID: PMC2911766.13. Eichenbaum KD, Neustein SM. Acute lung injury after thoracic surgery. J Cardiothorac Vasc Anesth. 2010; 24:681–90. DOI: 10.1053/j.jvca.2009.10.032. PMID: 20060320.14. Cheng YJ, Chan KC, Chien CT, Sun WZ, Lin CJ. Oxidative stress during 1-lung ventilation. J Thorac Cardiovasc Surg. 2006; 132:513–8. DOI: 10.1016/j.jtcvs.2006.03.060. PMID: 16935103.15. Kozian A, Schilling T, Fredén F, Maripuu E, Röcken C, Strang C, et al. One-lung ventilation induces hyperperfusion and alveolar damage in the ventilated lung:an experimental study. Br J Anaesth. 2008; 100:549–59. DOI: 10.1093/bja/aen021. PMID: 18308740.16. Alam N, Park BJ, Wilton A, Seshan VE, Bains MS, Downey RJ, et al. Incidence and risk factors for lung injury after lung cancer resection. Ann Thorac Surg. 2007; 84:1085–91. DOI: 10.1016/j.athoracsur.2007.05.053. PMID: 17888952.17. Licker M, de Perrot M, Spiliopoulos A, Robert J, Diaper J, Chevalley C, et al. Risk factors for acute lung injury after thoracic surgery for lung cancer. Anesth Analg. 2003; 97:1558–65. DOI: 10.1213/01.ANE.0000087799.85495.8A. PMID: 14633519.18. Brister NW, Barnette RE, Kim V, Keresztury M. Anesthetic considerations in candidates for lung volume reduction surgery. Proc Am Thorac Soc. 2008; 5:432–7. DOI: 10.1513/pats.200709-149ET. PMID: 18453351. PMCID: PMC2645315.19. Sentürk M. New concepts of the management of one-lung ventilation. Curr Opin Anaesthesiol. 2006; 19:1–4. DOI: 10.1097/01.aco.0000192778.17151.2c. PMID: 16547426.20. Reuter DA, Goepfert MS, Goresch T, Schmoeckel M, Kilger E, Goetz AE. Assessing fluid responsiveness during open chest conditions. Br J Anaesth. 2005; 94:318–23. DOI: 10.1093/bja/aei043. PMID: 15591333.21. Reuter DA, Goresch T, Goepfert MS, Wildhirt SM, Kilger E, Goetz AE. Effects of mid-line thoracotomy on the interaction between mechanical ventilation and cardiac filling during cardiac surgery. Br J Anaesth. 2004; 92:808–13. DOI: 10.1093/bja/aeh151. PMID: 15096443.22. de Waal EE, Rex S, Kruitwagen CL, Kalkman CJ, Buhre WF. Dynamic preload indicators fail to predict fluid responsiveness in open-chest conditions. Crit Care Med. 2009; 37:510–5. DOI: 10.1097/CCM.0b013e3181958bf7. PMID: 19114886.23. Wyffels PA, Sergeant P, Wouters PF. The value of pulse pressure and stroke volume variation as predictors of fluid responsiveness during open chest surgery. Anaesthesia. 2010; 65:704–9. DOI: 10.1111/j.1365-2044.2010.06371.x. PMID: 20477782.24. Sander M, Spies CD, Berger K, Grubitzsch H, Foer A, Krämer M, et al. Prediction of volume response under open-chest conditions during coronary artery bypass surgery. Crit Care. 2007; 11:R121. DOI: 10.1186/cc6181. PMID: 18034888. PMCID: PMC2246213.25. Vieillard-Baron A, Chergui K, Augarde R, Prin S, Page B, Beauchet A, et al. Cyclic changes in arterial pulse during respiratory support revisited by Doppler echocardiography. Am J Respir Crit Care Med. 2003; 168:671–6. DOI: 10.1164/rccm.200301-135OC. PMID: 12869360.26. Michard F. Changes in arterial pressure during mechanical ventilation. Anesthesiology. 2005; 103:419–28. DOI: 10.1097/00000542-200508000-00026. PMID: 16052125.27. De Blasi RA, Palmisani S, Cigognetti L, Iasenzaniro M, Arcioni R, Mercieri M, et al. Effects of sternotomy on heart-lung interaction in patients undergoing cardiac surgery receiving pressure- controlled mechanical ventilation. Acta Anaesthesiol Scand. 2007; 51:441–6. DOI: 10.1111/j.1399-6576.2007.01245.x. PMID: 17378782.28. Suehiro K, Okutani R. Influence of tidal volume for stroke volume variation to predict fluid responsiveness in patients undergoing one-lung ventilation. J Anesth. 2011; 25:777–80. DOI: 10.1007/s00540-011-1200-x. PMID: 21744128.29. Mesquida J, Kim HK, Pinsky MR. Effect of tidal volume, intrathoracic pressure, and cardiac contractility on variations in pulse pressure, stroke volume, and intrathoracic blood volume. Intensive Care Med. 2011; 37:1672–9. DOI: 10.1007/s00134-011-2304-3. PMID: 21739340. PMCID: PMC3818902.30. De Backer D, Taccone FS, Holsten R, Ibrahimi F, Vincent JL. Influence of respiratory rate on stroke volume variation in mechanically ventilated patients. Anesthesiology. 2009; 110:1092–7. DOI: 10.1097/ALN.0b013e31819db2a1. PMID: 19352152.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The effect of ambient pressure oxygen apply via T-piece in thoracoscopic surgery or thoracotomy
- Bronchial Cuff Volume of Univent Tube for One Lung Ventilation
- Change of the Peak Inspiratory Airway Pressure and Exhaled Volume during One Lung Ventilation
- Effect of Unilateral Lung Collapse and One-Lung Ventilation on Pulmonary Hemodynamics and Shunt Ratio in Dogs
- One-lung ventilation in a pediatric patient using a wire-guided endobronchial blocker for video-assisted thoracoscopic surgery: A case report