Ann Clin Neurophysiol.
2019 Jul;21(2):98-101. 10.14253/acn.2019.21.2.98.
Facial diplegia as a delayed complication of scrub typhus
- Affiliations
-
- 1Department of Neurology, Catholic University of Daegu School of Medicine, Daegu, Korea. jaehanpark@cu.ac.kr
- 2Department of Internal Medicine, Catholic University of Daegu School of Medicine, Daegu, Korea.
- KMID: 2454731
- DOI: http://doi.org/10.14253/acn.2019.21.2.98
Abstract
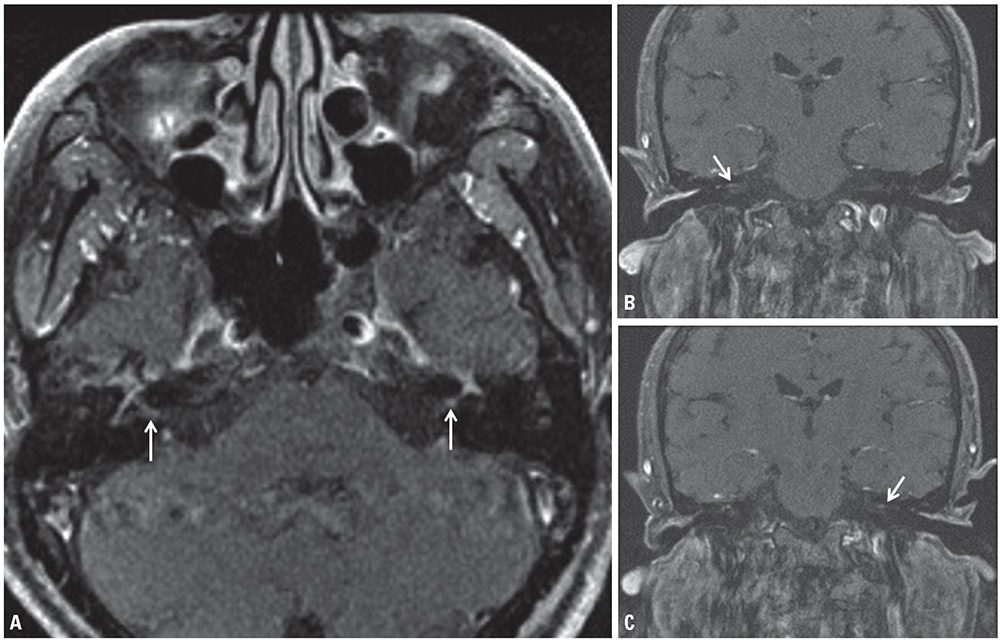
- A 64-year-old man presented with facial diplegia occurring 2 weeks after scrub typhus diagnosis. The serum scrub typhus antibody titer was elevated to 1:5120. Brain magnetic resonance imaging revealed contrast-enhancement of the signal for both facial nerves. He was administered prednisolone. After two weeks, the symptoms improved, and after one month, he completely recovered from facial diplegia. This is the first case in the literature in which the patient exhibited facial diplegia, a delayed complication, in scrub typhus. Facial diplegia should be considered a type of cranial nerve palsy that may occur as a delayed complication of scrub typhus.
Keyword
MeSH Terms
Figure
Reference
-
1. Jain V, Deshmukh A, Gollomp S. Bilateral facial paralysis: case presentation and discussion of differential diagnosis. J Gen Intern Med. 2006; 21:C7–C10.
Article2. Pai H, Sohn S, Seong Y, Kee S, Chang WH, Choe KW. Central nervous system involvement in patients with scrub typhus. Clin Infect Dis. 1997; 24:436–440.
Article3. Mahajan SK, Mahajan SK. Neuropsychiatric manifestations of scrub typhus. J Neurosci Rural Pract. 2017; 8:421–426.
Article4. Lin WR, Chen TH, Lin CY, Lu PL, Chen YH. Bilateral simultaneous facial palsy following scrub typhus meningitis: a case report and literature review. Kaohsiung J Med Sci. 2011; 27:573–576.
Article5. Hughes RA, Cornblath DR. Guillain-Barre' syndrome. Lancet. 2005; 366:1653–1666.6. Lee SH, Jung SI, Park KH, Choi SM, Park MS, Kim BC, et al. Guillain Barr syndrome associated with scrub typhus. Scand J Infect Dis. 2007; 39:826–828.7. Steenerson RL. Bilateral facial paralysis. Am J Otol. 1986; 7:99–103.8. Kang JI, Kim DM, Lee J. Acute sensorineural hearing loss and severe otalgia due to scrub typhus. BMC Infect Dis. 2009; 9:173.
Article9. Bhardwaj B, Panda P, Revannasiddaiah S, Bhardwaj H. Abducens nerve palsy in a patient with scrub typhus: a case report. Trop Biomed. 2013; 30:706–709.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pulmonary Artery Thrombosis Associated with Scrub Typhus
- A Case of Scrub Typhus with Bilateral Sudden Hearing Loss
- Epidemiologic characteristics of scrub typhus on Jeju Island
- Antibiotic Combination Therapy for Severe Scrub Typhus: Is It Necessary?
- Scrub typhus with complications of acute myocarditis and cardiac tamponade in metropolitan areas: two case reports