Ann Clin Neurophysiol.
2019 Jul;21(2):71-78. 10.14253/acn.2019.21.2.71.
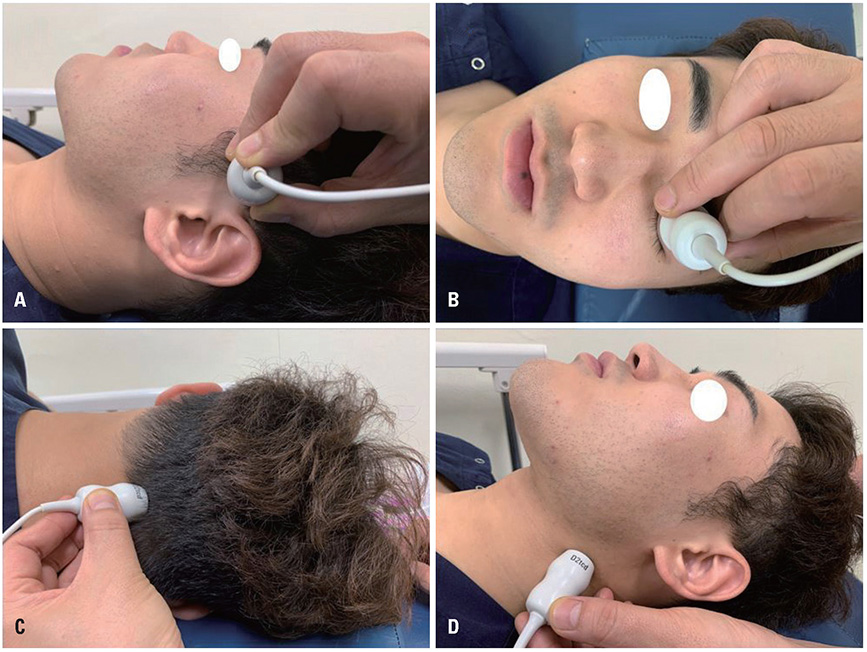
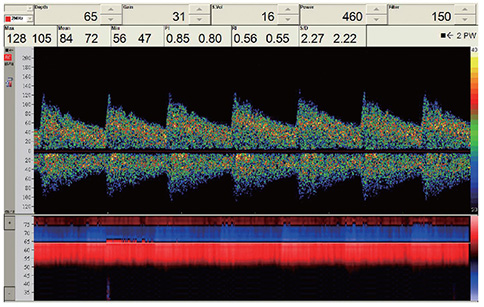
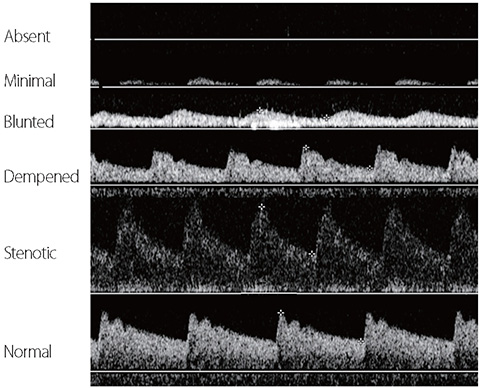
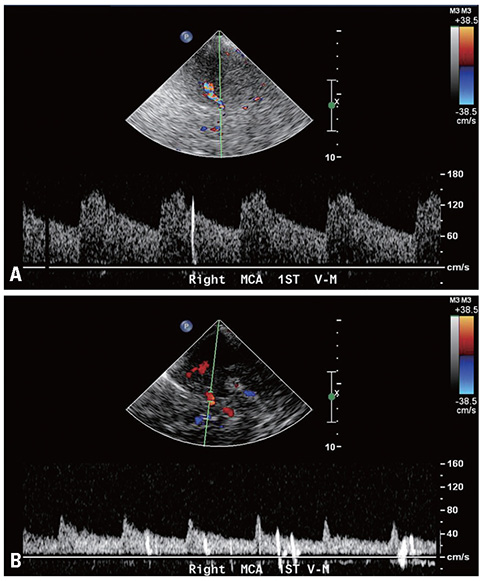
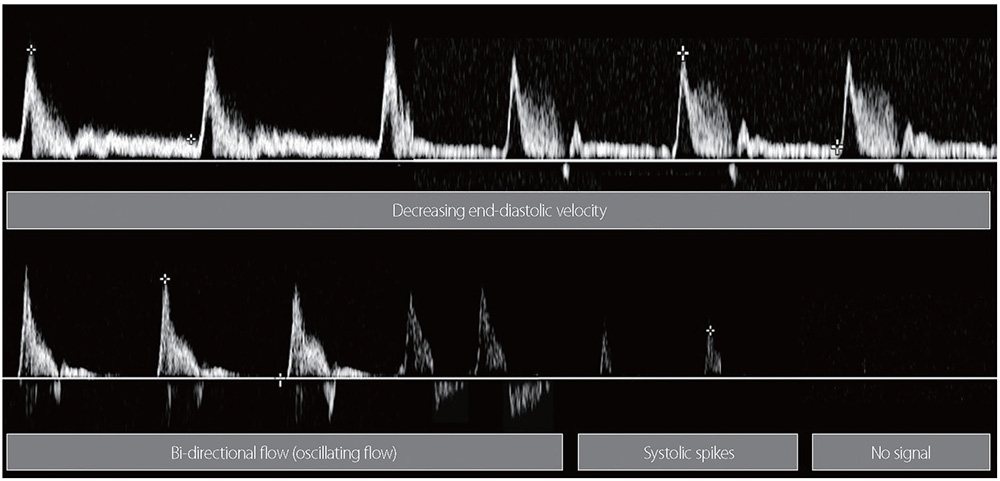
Transcranial Doppler: examination techniques and interpretation
- Affiliations
-
- 1Department of Neurology, Catholic University of Daegu School of Medicine, Daegu, Korea. dyr4173@cu.ac.kr
- 2Department of Neurology, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 3Department of Neurology, National Health Insurance Service Ilsan Hospital, Ilsan, Korea.
- KMID: 2454727
- DOI: http://doi.org/10.14253/acn.2019.21.2.71
Abstract
- Transcranial Doppler (TCD) was introduced in 1982 to assess intracranial arteries noninvasively, since when it has been widely used to assess and monitor cerebrovascular hemodynamics. The clinical applications of TCD are broadening to include other fields that require monitoring of the cerebral blood flow. TCD has fewer temporal and spatial restrictions than other methods, can be performed on less-compliant patients, and causes no harm to the body. However, its reliance on high levels of examiner skill and experience, as well as a lack of standardized scanning protocols are obstacles that still need to be overcome. In this report we review TCD examination techniques and interpret their findings for several conditions.
Figure
Reference
-
1. Aaslid R, Markwalder TM, Nornes H. Noninvasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries. J Neurosurg. 1982; 57:769–774.
Article2. Navarro JC, Lao AY, Sharma VK, Tsivgoulis G, Alexandrov AV. The accuracy of transcranial Doppler in the diagnosis of middle cerebral artery stenosis. Cerebrovasc Dis. 2007; 23:325–330.
Article3. Feldmann E, Wilterdink JL, Kosinski A, Lynn M, Chimowitz MI, Sarafin J, et al. The Stroke Outcomes and Neuroimaging of Intracranial Atherosclerosis (SONIA) trial. Neurology. 2007; 68:2099–2106.
Article4. Zhao L, Barlinn K, Sharma VK, Tsivgoulis G, Cava LF, Vasdekis SN, et al. Velocity criteria for intracranial stenosis revisited: an international multicenter study of transcranial Doppler and digital subtraction angiography. Stroke. 2011; 42:3429–3434.5. Alexandrov AV, Neumyer MM. Diagnostic criteria for cerebrovascular ultrasound. In : Alexandrov AV, editor. Cerebrovascular ultrasound in stroke prevention and treatment. 2nd ed. New York: Wiley Blackwell Publishing;2008. p. 79–129.6. Demchuk AM, Burgin WS, Christou I, Felberg RA, Barber PA, Hill MD, et al. Thrombolysis in brain ischemia (TIBI) transcranial Doppler flow grades predict clinical severity, early recovery, and mortality in patients treated with intravenous tissue plasminogen activator. Stroke. 2001; 32:89–93.
Article7. Schneider PA, Rossman ME, Bernstein EF, Ringelstein EB, Otis SM. Noninvasive assessment of cerebral collateral blood supply through the ophthalmic artery. Stroke. 1991; 22:31–36.
Article8. Kim Y, Sin DS, Park HY, Park MS, Cho KH. Relationship between flow diversion on transcranial Doppler sonography and leptomeningeal collateral circulation in patients with middle cerebral artery occlusive disorder. J Neuroimaging. 2009; 19:23–26.
Article9. Jauss M, Zanette E. Detection of right-to-left shunt with ultrasound contrast agent and transcranial Doppler sonography. Cerebrovasc Dis. 2000; 10:490–496.
Article10. Wu CT, Han K, Guo ZN, Yang Y, Gao YS, Bai J, et al. Effects of patient position on right-to-left shunt detection by contrast transcranial Doppler. Ultrasound Med Biol. 2015; 41:654–658.
Article11. Agustin SJ, Yumul MP, Kalaw AJ, Teo BC, Eng J, Phua Z, et al. Effects of posture on right-to-left shunt detection by contrast transcranial doppler. Stroke. 2011; 42:2201–2205.
Article12. Spencer MP, Moehring MA, Jesurum J, Gray WA, Olsen JV, Reisman M. Power M-mode transcranial Doppler for diagnosis of patent foramen ovale and assessing transcatheter closure. J Neuroimaging. 2004; 14:342–349.
Article13. Katsanos AH, Psaltopoulou T, Sergentanis TN, Frogoudaki A, Vrettou AR, Ikonomidis I, et al. Transcranial Doppler versus transthoracic echocardiography for the detection of patent foramen ovale in patients with cryptogenic cerebral ischemia: a systematic review and diagnostic test accuracy meta-analysis. Ann Neurol. 2016; 79:625–635.
Article14. Osiro S, Zurada A, Gielecki J, Shoja MM, Tubbs RS, Loukas M. A review of subclavian steal syndrome with clinical correlation. Med Sci Monit. 2012; 18:RA57–RA63.
Article15. Sakima H, Wakugawa Y, Isa K, Yasaka M, Ogata T, Saitoh M, et al. Correlation between the degree of left subclavian artery stenosis and the left vertebral artery waveform by pulse Doppler ultrasonography. Cerebrovasc Dis. 2011; 31:64–67.
Article16. Kliewer MA, Hertzberg BS, Kim DH, Bowie JD, Courneya DL, Carroll BA. Vertebral artery Doppler waveform changes indicating subclavian steal physiology. AJR Am J Roentgenol. 2000; 174:815–819.
Article17. Chang JJ, Tsivgoulis G, Katsanos AH, Malkoff MD, Alexandrov AV. Diagnostic accuracy of transcranial doppler for brain death confirmation: systematic review and meta-analysis. AJNR Am J Neuroradiol. 2016; 37:408–414.
Article18. Ducrocq X, Hassler W, Moritake K, Newell DW, von Reutern GM, Shiogai T, et al. Consensus opinion on diagnosis of cerebral circulatory arrest using Doppler-sonography: Task Force Group on cerebral death of the Neurosonology Research Group of the World Federation of Neurology. J Neurol Sci. 1998; 159:145–150.19. Frontera JA, Fernandez A, Schmidt JM, Claassen J, Wartenberg KE, Badjatia N, et al. Defining vasospasm after subarachnoid hemorrhage: what is the most clinically relevant definition? Stroke. 2009; 40:1963–1968.20. Yamakami I, Isobe K, Yamaura A, Nakamura T, Makino H. Vasospasm and regional cerebral blood flow (rCBF) in patients with ruptured intracranial aneurysm: serial rCBF studies with the xenon-133 inhalation method. Neurosurgery. 1983; 13:394–401.
Article21. Lindegaard KF, Nornes H, Bakke SJ, Sorteberg W, Nakstad P. Cerebral vasospasm after subarachnoid haemorrhage investigated by means of transcranial Doppler ultrasound. Acta Neurochir Suppl (Wien). 1988; 42:81–84.
Article22. Sviri GE, Ghodke B, Britz GW, Douville CM, Haynor DR, Mesiwala AH, et al. Transcranial Doppler grading criteria for basilar artery vasospasm. Neurosurgery. 2006; 59:360–366. discussion 360-366.
Article23. Soustiel JF, Shik V, Shreiber R, Tavor Y, Goldsher D. Basilar vasospasm diagnosis: investigation of a modified “Lindegaard Index” based on imaging studies and blood velocity measurements of the basilar artery. Stroke. 2002; 33:72–77.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Implications of a Variation of Middle Cerebral Artery in the Interpretation of Transcranial Doppler
- Usefulness of Transcranial Doppler Sonography for Determining Brain Death
- The Findings of MRI and Transcranial Doppler Sonography in Three Cases of Moyamoya Disease
- Transcranial Doppler Measurement of Intracraial Arterial Flow Velocity in Subarachnoid Hemorrhage
- Transcranial Doppler Sonography in Acute Ischemic Stroke