Korean Circ J.
2019 Jun;49(6):498-510. 10.4070/kcj.2018.0296.
The Effects of Preoperative Aspirin on Coronary Artery Bypass Surgery: a Systematic Meta-Analysis
- Affiliations
-
- 1Department of Internal Medicine and Cardiovascular Center, Seoul National University Hospital, Seoul, Korea. bkkoo@snu.ac.kr
- 2Department of Internal Medicine and Cardiovascular Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Division of Biostatistics, Center for Devices and Radiological Health, Food and Drug Administration, Silver Spring, MD, USA.
- 4Department of Thoracic and Cardiovascular Surgery, Seoul National University Hospital, Seoul, Korea.
- 5Department of Thoracic and Cardiovascular Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 6Institute of Aging, Seoul National University, Seoul, Korea.
- KMID: 2454045
- DOI: http://doi.org/10.4070/kcj.2018.0296
Abstract
- BACKGROUND AND OBJECTIVES
Aspirin plays an important role in the maintenance of graft patency and the prevention of thrombotic event after coronary artery bypass graft surgery (CABG). However, the use of preoperative aspirin is still under debate due to the risk of bleeding.
METHODS
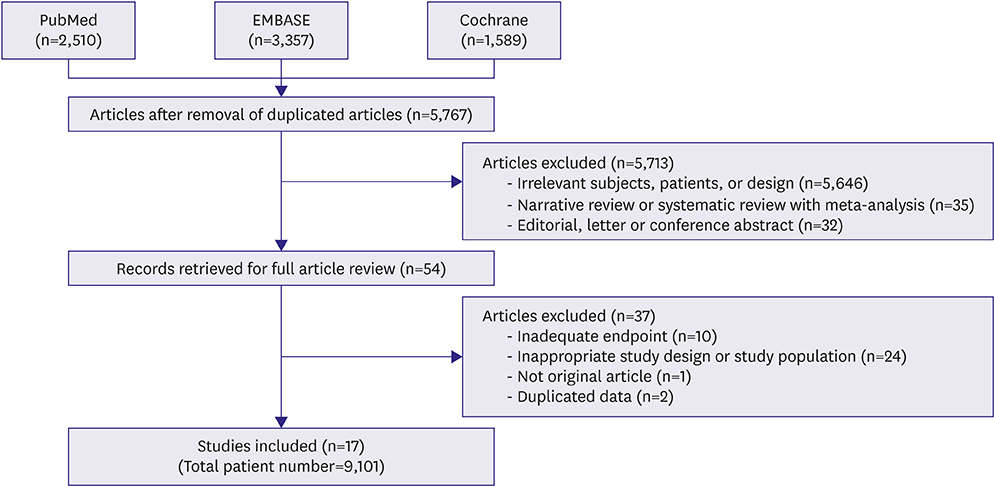
From PubMed, EMBASE, and Cochrane Central Register of Controlled Trials, data were extracted by 2 independent reviewers. Meta-analysis using random effect model was performed.
RESULTS
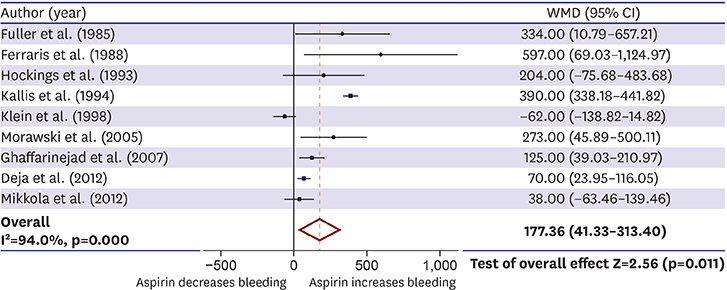
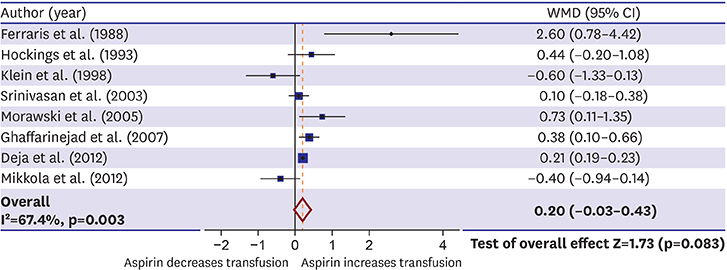
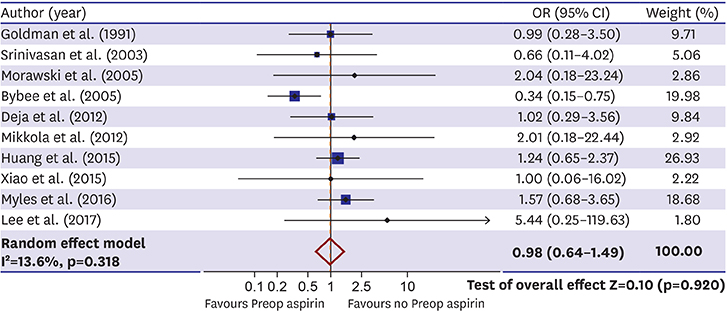
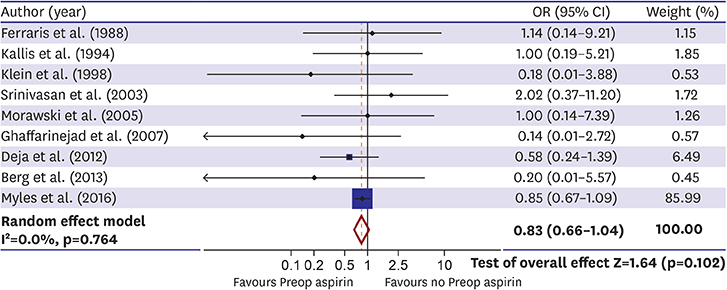
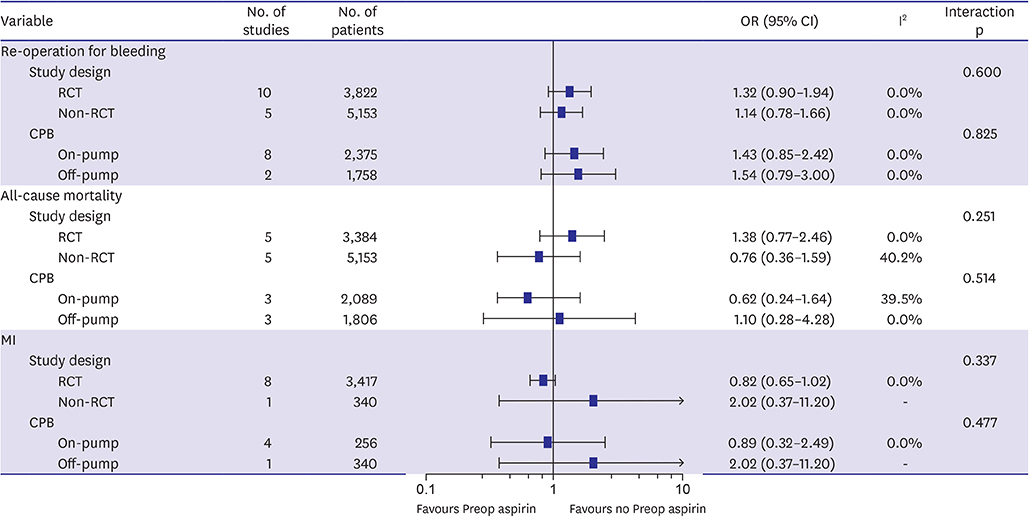
We performed a systemic meta-analysis of 17 studies (12 randomized controlled studies and 5 non-randomized registries) which compared clinical outcomes of 9,101 patients who underwent CABG with or without preoperative aspirin administration. Preoperative aspirin increased chest tube drainage (weighted mean difference 177.4 mL, 95% confidence interval [CI], 41.3-313.4; p=0.011). However, the risk of re-operation for bleeding was not different between the preoperative aspirin group and the control group (3.2% vs. 2.4%; odds ratio [OR], 1.23; 95% CI, 0.94-1.60; p=0.102). There was no difference in the rates of all-cause mortality (1.6% vs. 1.5%; OR, 0.98; 95% CI, 0.64-1.49; p=0.920) and myocardial infarction (MI) (8.7% vs. 10.4%; OR, 0.83; 95% CI, 0.66-1.04; p=0.102) between patients with and without preoperative aspirin administration.
CONCLUSIONS
Although aspirin increased the amount of chest tube drainage, it was not associated with increased risk of re-operation for bleeding. In addition, the risks of early postoperative all-cause mortality and MI were not reduced by using preoperative aspirin.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Feel Free to Use Aspirin before Coronary Artery Bypass Surgery
Jung-Min Ahn
Korean Circ J. 2019;49(6):511-513. doi: 10.4070/kcj.2019.0155.
Reference
-
1. Schwartz L, Bourassa MG, Lespérance J, et al. Aspirin and dipyridamole in the prevention of restenosis after percutaneous transluminal coronary angioplasty. N Engl J Med. 1988; 318:1714–1719.
Article2. Savage MP, Goldberg S, Bove AA, et al. Effect of thromboxane A2 blockade on clinical outcome and restenosis after successful coronary angioplasty. Multi-hospital eastern atlantic restenosis trial (M-HEART II). Circulation. 1995; 92:3194–3200.3. Goldman S, Copeland J, Moritz T, et al. Improvement in early saphenous vein graft patency after coronary artery bypass surgery with antiplatelet therapy: results of a veterans administration cooperative study. Circulation. 1988; 77:1324–1332.
Article4. Chesebro JH, Clements IP, Fuster V, et al. A platelet-inhibitor-drug trial in coronary-artery bypass operations: benefit of perioperative dipyridamole and aspirin therapy on early postoperative vein-graft patency. N Engl J Med. 1982; 307:73–78.5. Hastings S, Myles P, McIlroy D. Aspirin and coronary artery surgery: a systematic review and meta-analysis. Br J Anaesth. 2015; 115:376–385.
Article6. Bybee KA, Powell BD, Valeti U, et al. Preoperative aspirin therapy is associated with improved postoperative outcomes in patients undergoing coronary artery bypass grafting. Circulation. 2005; 112:I286–I292.7. Dacey LJ, Munoz JJ, Johnson ER, et al. Effect of preoperative aspirin use on mortality in coronary artery bypass grafting patients. Ann Thorac Surg. 2000; 70:1986–1990.
Article8. Mangano DT. Multicenter Study of Perioperative Ischemia Research Group. Aspirin and mortality from coronary bypass surgery. N Engl J Med. 2002; 347:1309–1317.
Article9. Awtry EH, Loscalzo J. Aspirin. Circulation. 2000; 101:1206–1218.
Article10. Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: executive summary: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Thorac Cardiovasc Surg. 2012; 143:4–34.11. Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Circulation. 2011; 124:e652–735.12. Ferraris VA, Brown JR, Despotis GJ, et al. 2011 update to the Society of Thoracic Surgeons and the Society of Cardiovascular Anesthesiologists blood conservation clinical practice guidelines. Ann Thorac Surg. 2011; 91:944–982.
Article13. Ferraris VA, Saha SP, Oestreich JH, et al. 2012 update to the Society of Thoracic Surgeons guideline on use of antiplatelet drugs in patients having cardiac and noncardiac operations. Ann Thorac Surg. 2012; 94:1761–1781.
Article14. Myles PS, Smith JA, Forbes A, et al. Stopping vs. continuing aspirin before coronary artery surgery. N Engl J Med. 2016; 374:728–737.
Article15. Cahill RA, McGreal GT, Crowe BH, et al. Duration of increased bleeding tendency after cessation of aspirin therapy. J Am Coll Surg. 2005; 200:564–573.
Article16. Ahmed I, Sutton AJ, Riley RD. Assessment of publication bias, selection bias, and unavailable data in meta-analyses using individual participant data: a database survey. BMJ. 2012; 344:d7762.
Article17. Head SJ, Kieser TM, Falk V, Huysmans HA, Kappetein AP. Coronary artery bypass grafting: part 1--the evolution over the first 50 years. Eur Heart J. 2013; 34:2862–2872.
Article18. Fuller JK, Copeland JG. Does short-term pre-operative aspirin in coronary bypass patients increase post-operative bleeding? Vasc Surg. 1985; 19:174–178.
Article19. Ferraris VA, Ferraris SP, Lough FC, Berry WR. Preoperative aspirin ingestion increases operative blood loss after coronary artery bypass grafting. Ann Thorac Surg. 1988; 45:71–74.
Article20. Goldman S, Copeland J, Moritz T, et al. Starting aspirin therapy after operation. Effects on early graft patency. Circulation. 1991; 84:520–526.21. Hockings BE, Ireland MA, Gotch-Martin KF, Taylor RR. Placebo-controlled trial of enteric coated aspirin in coronary bypass graft patients. Effect on graft patency. Med J Aust. 1993; 159:376–378.22. Klein M, Keith PR, Dauben HP, et al. Aprotinin counterbalances an increased risk of peri-operative hemorrhage in CABG patients pre-treated with aspirin. Eur J Cardiothorac Surg. 1998; 14:360–366.23. Ghaffarinejad MH, Fazelifar AF, Shirvani SM, et al. The effect of preoperative aspirin use on postoperative bleeding and perioperative myocardial infarction in patients undergoing coronary artery bypass surgery. Cardiol J. 2007; 14:453–457.24. Collaborative overview of randomised trials of antiplatelet therapy--I: Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. Antiplatelet Trialists' Collaboration. BMJ. 1994; 308:81–106.25. Leon MB, Baim DS, Popma JJ, et al. A clinical trial comparing three antithrombotic-drug regimens after coronary-artery stenting. Stent Anticoagulation Restenosis Study Investigators. N Engl J Med. 1998; 339:1665–1671.26. Myles PS. Stopping aspirin before coronary artery surgery: between the devil and the deep blue sea. Circulation. 2011; 123:571–573.27. Sun JC, Whitlock R, Cheng J, et al. The effect of pre-operative aspirin on bleeding, transfusion, myocardial infarction, and mortality in coronary artery bypass surgery: a systematic review of randomized and observational studies. Eur Heart J. 2008; 29:1057–1071.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Feel Free to Use Aspirin before Coronary Artery Bypass Surgery
- Effects of Preoperative Combined Antiplatelet Agents on the Postoperative Bleeding that Occurs during Off-pump Coronary Artery Bypass Surgery
- Effect of Preoperative Aspirin Use on Postoperative Bleeding and Thromboelastography in Off-Pump Coronary Artery Bypass Operations
- Effects of Preoperative Continuous Use of Aspirin and Plavix in Off-pump Coronary Artery Bypass Surgery
- Preoperative Aspirin Resistance does not Increase Myocardial Injury during Off-pump Coronary Artery Bypass Surgery