J Korean Soc Radiol.
2019 May;80(3):591-597. 10.3348/jksr.2019.80.3.591.
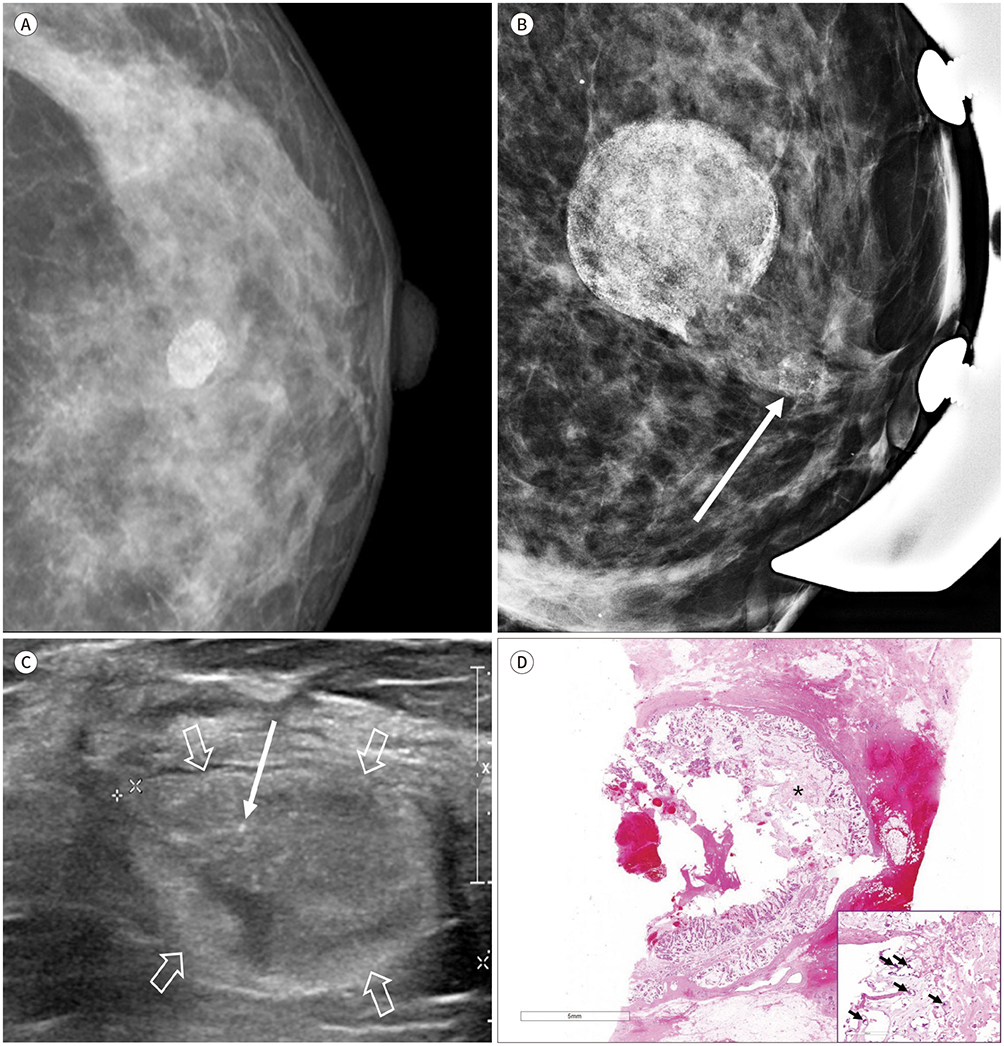
Invasive Breast Cancer Presenting as a Mass Replaced by Calcification on Mammography: A Report of Two Cases
- Affiliations
-
- 1Department of Radiology, Dong-A University Medical Center, Dong-A University College of Medicine, Busan, Korea. jhrad@dau.ac.kr
- 2Pathology Reference Lab, Seegene Medical Foundation, Busan, Korea.
- 3Department of Surgery, Dong-A University Medical Center, Dong-A University College of Medicine, Busan, Korea.
- KMID: 2454041
- DOI: http://doi.org/10.3348/jksr.2019.80.3.591
Abstract
- A distinct calcification pattern is one of the criteria for determining the malignancy of breast cancer according to the Breast Imaging Reporting and Data System. A mass almost entirely replaced by calcification, however, is difficult to categorize and likely to be misdiagnosed. We present the report of two patients with invasive carcinoma of the breast that presented as a mass replaced by calcification on mammography. In the first case, the mass was confirmed as a mixed carcinoma comprising mucinous and micropapillary carcinoma, and in the second case, the mass was a mucinous carcinoma. Diagnosis of cancer in the latter case was missed as the mass had been assessed as a category 2 typically benign calcification at the first screening mammography 2 years ago. This report merits publication because it shows that a mass replaced by calcification on mammography can be misdiagnosed as a benign finding.
MeSH Terms
Figure
Reference
-
1. American College of Radiology. ACR BI-RADS atlas: breast imaging reporting and data system. 5th ed. Reston, VA: American College of Radiology;2013.2. Erguvan-Dogan B, Yazgan C, Atasoy C, Sak SD, Tukel S, Ceyhan K, et al. Radiologic-pathologic conference of the University of Ankara Medical School: metaplastic breast carcinoma with osteochondrosarcomatous differentiation. AJR Am J Roentgenol. 2005; 185:1593–1594.3. Lee JH, Kim EK, Choi SS, Nam KJ, Kim DC, Cho SH. Metaplastic breast carcinoma with extensive osseous differentiation: a case report. Breast. 2008; 17:314–316.
Article4. Evans HA, Shaughnessy EA, Nikiforov YE. Infiltrating ductal carcinoma of the breast with osseous metaplasia: imaging findings with pathologic correlation. AJR Am J Roentgenol. 1999; 172:1420–1422.
Article5. Wilson DA, Kalisher L, Port JE, Titus JM, Kirzner HL. Breast imaging case of the day. Pure mucinous carcinoma with calcifying matrix. Radiographics. 1997; 17:800–880.
Article6. Tani H, Murakami R, Yoshida T, Kumita S, Yanagihara K, Iida S, et al. Mucinous carcinoma of the breast accompanied by coarse calcification. Open J Med Imaging. 2012; 2:125–127.
Article7. Alghofaily KA, Almushayqih MH, Alanazi MF, Salamah AAB, Benediktsson H. Primary osteosarcoma of the breast arising in an intraductal papilloma. Case Rep Radiol. 2017; 2017:5787829.
Article8. Kim JH, Woo HY, Kim EK, Kim MJ, Moon HJ, Yoon JH. Metastatic osteosarcoma to the breast presenting as a densely calcified mass on mammography. J Breast Cancer. 2016; 19:87–91.
Article9. Ozsaran AA, Dikmen Y, Terek MC, Ulukus M, Ozdemir N, Orgüc S, et al. Bilateral metastatic carcinoma of the breast from primary ovarian cancer. Arch Gynecol Obstet. 2000; 264:166–167.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mucinous Breast Carcinoma Presenting as a Coarse and Densely Calcified Mass on Mammography: A Case Report
- Mammographic findings of breast cancer: Emphasis on the tumor and microcalcifications
- Misdiagnosed Breast Cancer on Mammography Retrospective Analysis in 17 Cases
- Usefulness of Ultrasonography for Detection of Breast Cancer in Patients under 30 Years of Age
- Early screening for breast cancer