Korean J Gastroenterol.
2019 Jul;74(1):46-50. 10.4166/kjg.2019.74.1.46.
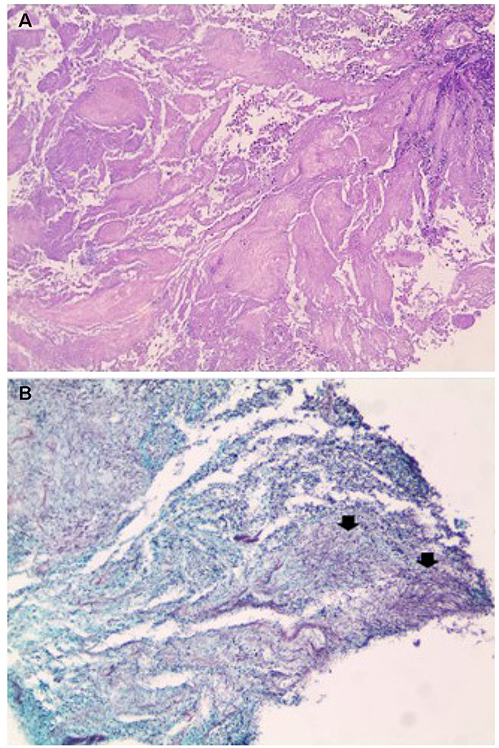
Colonic Diffuse Large B-cell Lymphoma Hidden in Actinomycosis
- Affiliations
-
- 1Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea. pinetrees@hanmail.net
- 2Department of Anatomic Pathology, Kangwon National University School of Medicine, Chuncheon, Korea.
- KMID: 2453258
- DOI: http://doi.org/10.4166/kjg.2019.74.1.46
Abstract
- Actinomycosis can mask malignant diseases. This paper reports a case of colonic diffuse large B-cell lymphoma (DLBCL), which was misdiagnosed as abdominal actinomycosis. A 76-year-old woman presented with right flank pain and weight loss. Abdominal CT and colonoscopy revealed a huge ascending colon mass. Despite the initial impression of a malignancy, a colonoscopic biopsy revealed no malignant cells, but sulfur granules and a filamentous organism suggesting actinomycosis. Intravenous penicillin G was administered under the impression of abdominal actinomycosis but her condition deteriorated rapidly. Follow up CT showed markedly increased colon mass and new multiple nodular lesions around the ascending colon. Sono-guided percutaneous biopsy of the nodular lesion was performed. The pathological result was DLBCL. The patient was scheduled to undergo chemotherapy but the patient expired due to cancer progression. The diagnosis of gastrointestinal infiltrating tumors is often difficult because a superficial biopsy usually does not provide a confirmative diagnosis. This case highlights the difficulty in making a correct diagnosis of lymphoma due to the concomitant actinomycosis. Malignant conditions must be considered in cases of actinomycosis with no response to antimicrobial therapy.
MeSH Terms
Figure
Reference
-
1. Andrews CN, John Gill M, Urbanski SJ, Stewart D, Perini R, Beck P. Changing epidemiology and risk factors for gastrointestinal non-Hodgkin's lymphoma in a North American population: population-based study. Am J Gastroenterol. 2008; 103:1762–1769.
Article2. Katsumata R, Matsumoto H, Motoyasu O, et al. Primary colorectal lymphoma comprising both components of diffuse large B-cell lymphoma and mucosa-associated lymphoid tissue lymphoma combined with cytomegalovirus colitis. Clin J Gastroenterol. 2016; 9:59–62.
Article3. Choi MK, Kim GH. Diagnosis and treatment of gastric MALT lymphoma. Korean J Gastroenterol. 2011; 57:272–280.
Article4. Lim JA, Wong PS, Leong KN, Wong KL, Chow TS. Masking and misleading: concomitant actinomycosis and B-cell lymphoma - a case report and review of literature. Scott Med J. 2018; 63:125–131.
Article5. Gill SS, Heuman DM, Mihas AA. Small intestinal neoplasms. J Clin Gastroenterol. 2001; 33:267–282.
Article6. Shepherd NA, Hall PA, Coates PJ, Levison DA. Primary malignant lymphoma of the colon and rectum. A histopathological and immunohistochemical analysis of 45 cases with clinicopathological correlations. Histopathology. 1998; 12:235–252.
Article7. Wong MT, Eu KW. Primary colorectal lymphomas. Colorectal Dis. 2006; 8:586–591.
Article8. Kim YH, Lee JH, Yang SK, et al. Primary colon lymphoma in Korea: a KASID (Korean Association for the Study of Intestinal Diseases) study. Dig Dis Sci. 2005; 50:2243–2247.
Article9. Ryu SH, Cheon JH, Kim JY, et al. The early diagnostic accuracy for gastrointestinal T-cell lymphoma from a perspective of gastroenterologists. Intest Res. 2011; 9:19–26.
Article10. Choe WH, Kim YH, Kim BJ, et al. The different colonoscopic manifestations of primary colorectal lymphomas by their cellular origin. Intest Res. 2003; 1:22–30.11. Jiang C, Gu L, Luo M, Xu Q, Zhou H. Primary rectal lymphoma: a case report and literature review. Oncol Lett. 2015; 10:43–44.
Article12. Lee HJ, Han JK, Kim TK, et al. Primary colorectal lymphoma: spectrum of imaging findings with pathologic correlation. Eur Radiol. 2002; 12:2242–2249.
Article13. Valour F, Sénéchal A, Dupieux C, et al. Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist. 2014; 7:183–197.14. Ercolak V, Paydas S, Ergin M, et al. Abdominal actinomycosis with multiple myeloma: a case report. Oncol Lett. 2014; 8:1876–1878.
Article15. Carneiro L, Ferreira R, Pinto J. The lymphoma hidden in actinomycosis. GE Port J Gastroenterol. 2016; 23:273–275.
Article16. Blanco-Vela CI, Luna-Ayala VM, Perez-Aguirre J. Colonic mass secondary to actinomycosis: a case report and literature review. Rev Gastroenterol Mex. 2014; 79:206–208.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Primary Rectal Diffuse Large B Cell LymphomaPresented as Multiple Polypoid Lesions
- Relapse of Ocular Lymphoma following Primary Testicular Diffuse Large B-cell Lymphoma
- A Case of Epstein-Barr Virus-Positive Diffuse Large B-Cell Lymphoma Occurring in Thyroid Gland
- Inverse Psoriasis Developed in a Patient with Diffuse Large B Cell Lymphoma
- Relationships among Hepatitis C Virus, Hepatocellular Carcinoma, and Diffuse Large B Cell Lymphoma: A Case Report