J Korean Ophthalmol Soc.
2019 Jul;60(7):701-705. 10.3341/jkos.2019.60.7.701.
Chronic Recurrent Methicillin Resistant Staphylococcus Hemolyticus Endophthalmitis after Cataract Surgery
- Affiliations
-
- 1Department of Ophthalmology, Hanyang University College of Medicine, Seoul, Korea. syu2000@hanmail.net
- KMID: 2453023
- DOI: http://doi.org/10.3341/jkos.2019.60.7.701
Abstract
- PURPOSE
To report a case of recurrent endophthalmitis due to methicillin resistant Staphylococcus hemolyticus after phacoemulsification and posterior chamber intraocular lens (IOL) implantation.
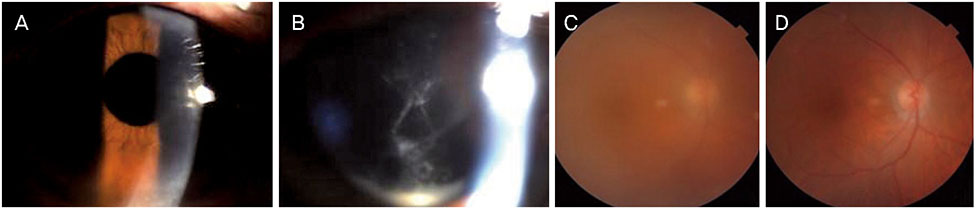
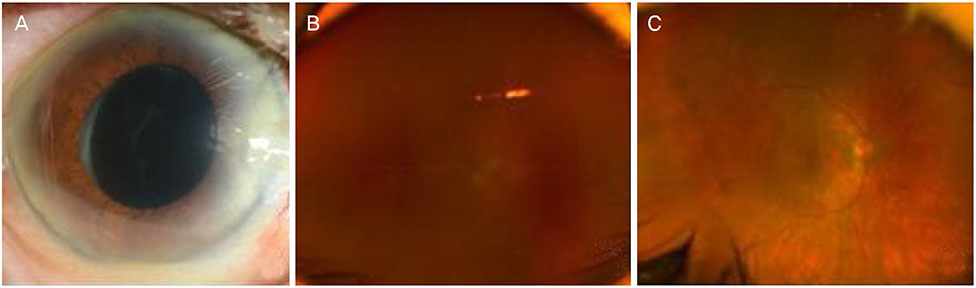
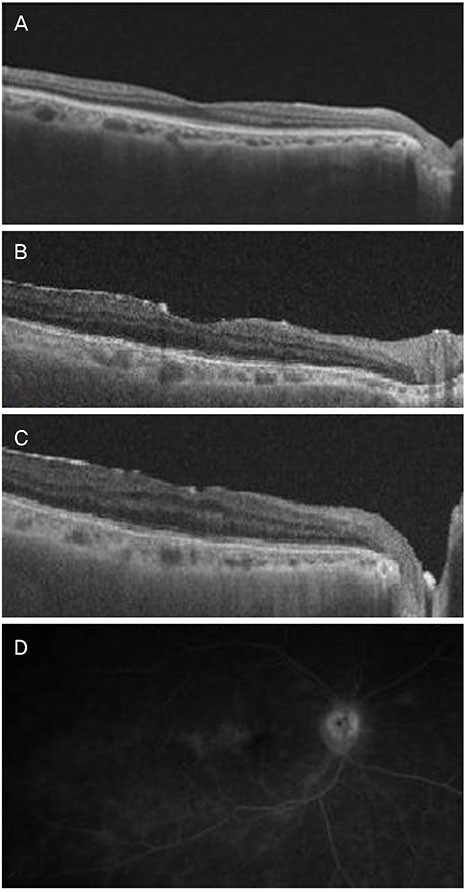
CASE SUMMARY
A 76-year-old female visited our outpatient clinic with decreased vision 40 days after uncomplicated cataract surgery in her right eye. At the visit, anterior chamber inflammation and cloudy fluid between the posterior capsule and IOL were observed. Uveitis due to residual cortex of lens or capsular block syndrome was suspected, so YAG laser capsulotomy and subconjunctival injection of dexamethasone were performed. Two days later, hypopyon and vitreous opacity were seen. The patient underwent an emergency vitrectomy and intravitreal antibiotic injection with suspicion of bacterial endophthalmitis. The culture was negative. Twenty days after the vitrectomy, anterior chamber inflammation and vitreous opacity developed. The recurrence of endophthalmitis was suspected due to infection by bacteria in the surrounding tissue of the IOL, so the patient underwent an IOL and lens capsule removal with intravitreal antibiotic injection. At this time, the culture revealed methicillin resistant staphylococcus hemolyticus. Systemic and topical vancomycin was then administered, resulting in decreased inflammation. Twenty days after the IOL removal, decreased vision, anterior chamber inflammation, and vitreous opacity developed. Endophthalmitis was decreased by intravitreal antibiotic injection and topical antibiotic treatment.
CONCLUSIONS
Methicillin resistant staphylococcus hemolyticus should be considered in the differential diagnosis of chronic recurrent endophthalmitis after cataract surgery.
MeSH Terms
-
Aged
Ambulatory Care Facilities
Anterior Chamber
Bacteria
Cataract*
Dexamethasone
Diagnosis, Differential
Emergencies
Endophthalmitis*
Female
Humans
Inflammation
Lasers, Solid-State
Lenses, Intraocular
Methicillin Resistance*
Methicillin*
Phacoemulsification
Recurrence
Staphylococcus*
Uveitis
Vancomycin
Vitrectomy
Dexamethasone
Methicillin
Vancomycin
Figure
Reference
-
1. Vaziri K, Schwartz SG, Kishor K, Flynn HW Jr. Endophthalmitis: state of the art. Clin Ophthalmol. 2015; 9:95–108.2. Durand ML. Endophthalmitis. Clin Microbiol Infect. 2013; 19:227–234.3. Endophthalmitis Vitrectomy Study Group. Results of the endophthalmitis vitrectomy study. A randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol. 1995; 113:1479–1496.4. Ramakrishnan R, Bharathi MJ, Shivkumar C, et al. Microbiological profile of culture-proven cases of exogenous and endogenous endophthalmitis: a 10-year retrospective study. Eye (Lond). 2009; 23:945–956.
Article5. Cao H, Zhang L, Li L, Lo S. Risk factors for acute endophthalmitis following cataract surgery: a systematic review and meta-analysis. PLoS One. 2013; 8:e71731.
Article6. Shirodkar AR, Pathengay A, Flynn HW Jr, et al. Delayed-versus acute-onset endophthalmitis after cataract surgery. Am J Ophthalmol. 2012; 153:391–398.e2.7. Königsdörffer E, Augsten R, Oehme A, Strobel J. Prognosis of postoperative endophthalmitis. Ophthalmologe. 2000; 97:121–125.8. Rogers NK, Fox PD, Noble BA, et al. Aggressive management of an epidemic of chronic pseudophakic endophthalmitis: results and literature survey. Br J Ophthalmol. 1994; 78:115–119.
Article9. Schimel AM, Miller D, Flynn HW Jr. Endophthalmitis isolates and antibiotic susceptibilities: a 10-year review of culture-proven cases. Am J Ophthalmol. 2013; 156:50–52.e1.
Article10. Czekaj T, Ciszewski M, Szewczyk EM. Staphylococcus hemolyticus - an emerging threat in the twilight of the antibiotics age. Microbiology. 2015; 161:2061–2068.11. Wong RW, Rhodes KM. Endophthalmitis caused by Staphylococcus hominis and two different colonies of Staphylococcus hemolyticus after cataract surgery. Retin Cases Brief Rep. 2015; 9:181–184.12. Packer M, Chang DF, Dewey SH, et al. Prevention, diagnosis, and management of acute postoperative bacterial endophthalmitis. J Cataract Refract Surg. 2011; 37:1699–1714.
Article13. Han DP, Wisniewski SR, Wilson LA, et al. Spectrum and susceptibilities of microbiologic isolates in the endophthalmitis vitrectomy study. Am J Ophthalmol. 1996; 122:1–17.
Article14. Callegan MC, Engelbert M, Parke DW 2nd, et al. Bacterial endophthalmitis: epidemiology, therapeutics, and bacterium-host interactions. Clin Microbiol Rev. 2002; 15:111–124.
Article15. Smith RE. Inflammation after cataract surgery. Am J Ophthalmol. 1986; 102:788–790.
Article16. Ormerod LD, Ho DD, Becker LE, et al. Endophthalmitis caused by the coagulase-negative staphylococcoi. 1 Disease spectrum and outcome. Ophthalmology. 1993; 100:715–723.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Detection of Multidrug Resistant Patterns and Associated - genes of Methicillin Resistant Staphylococcus aureus ( MRSA ) Isolated from Clinical Specimens
- Bilateral Staphylococcus Epidermidis Endophthalmitis After Cataract Extraction
- A statistical analysis of methicillin-resistant staphylococcus aureus
- Subacute Methicillin-resistant Coagulase-Negative Staphylococcus hominis Endophthalmitis after Penetrating Keratoplasty Re-operation
- A case of multiple furunculosis caused by methicillin-resistant staphylococcs aureus