Allergy Asthma Immunol Res.
2019 Sep;11(5):723-735. 10.4168/aair.2019.11.5.723.
Clinical Features and Culprit Food Allergens of Korean Adult Food Allergy Patients: A Cross-Sectional Single-Institute Study
- Affiliations
-
- 1Division of Allergy and Immunology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. parkjw@yuhs.ac
- 2Institute of Allergy, Yonsei University College of Medicine, Seoul, Korea.
- 3Division of Pulmonology, Department of Internal Medicine, National Health Insurance Service Ilsan Hospital, Goyang, Korea.
- KMID: 2452761
- DOI: http://doi.org/10.4168/aair.2019.11.5.723
Abstract
- PURPOSE
To investigate the causative allergens and clinical characteristics of Korean adult patients with food allergy (FA).
METHODS
This retrospective, cross-sectional single-institutional study enrolled Korean adult patients (n = 812) suspected of having FA. For diagnosis, causality assessment history taking, ImmunoCAP specific immunoglobulin E measurement and/or skin prick test were performed.
RESULTS
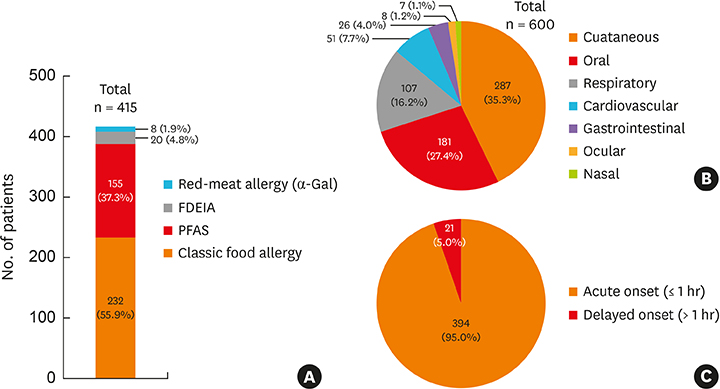
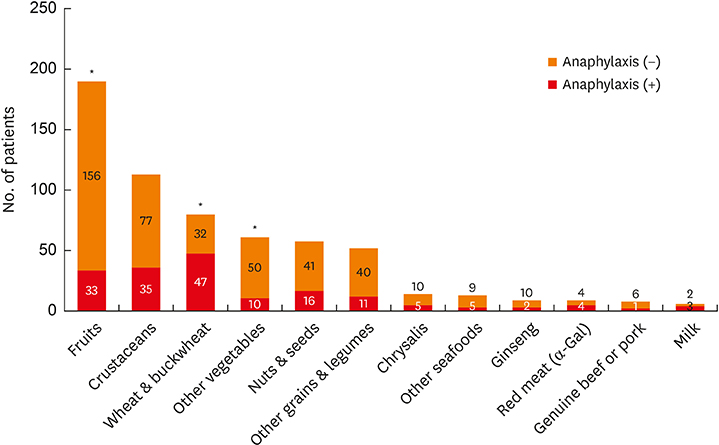
Among 812 patients, 415 were diagnosed as having FA. The most common causative allergen was fruit, with a diagnosis of pollen food allergy syndrome (PFAS: 155, 37.3%), followed by crustaceans (111, 26.7%), wheat (63, 15.1%), fruits in patients without PFAS(43, 10.3%), buckwheat (31, 7.4%), peanut (31, 7.4%), walnut (25, 6.0%), red meat due to reaction to galactose-α-1,3-galactose (α-Gal) (8, 1.9%), and silkworm pupa (13, 3.1%). Allergy to egg, milk, fish, or shellfish was rare in Korean adults. One-third of patients with FA exhibited multiple FAs (238/415, 57.3%); the average number of causative allergens was 2.39. About 129 patients (31.0%) were diagnosed as having anaphylaxis; in these patients, wheat was the most frequent causative food. Twenty patients were further diagnosed with food-dependent exercise-induced anaphylaxis (FDEIA); all were due to wheat. In particular, crustaceans, wheat, PFAS, buckwheat, and red meat (α-Gal) were also frequent causes of anaphylaxis.
CONCLUSIONS
Wheat, fruits with or without PFAS, and crustaceans are important and frequent causative allergens in Korean adult FA; these allergens differ from those found in childhood FA. It is notable that non-classic allergies, such as PFAS, FDEIA, and α-Gal allergy, are the important causes of anaphylaxis in Korean adult FA.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Revised Pollen Calendar in Korea
Jung-Won Park
Allergy Asthma Immunol Res. 2020;12(2):171-172. doi: 10.4168/aair.2020.12.2.171.
Reference
-
1. Sicherer SH. Epidemiology of food allergy. J Allergy Clin Immunol. 2011; 127:594–602.
Article2. Rhee CS, Wee JH, Ahn JC, Lee WH, Tan KL, Ahn S, et al. Prevalence, risk factors and comorbidities of allergic rhinitis in South Korea: The Fifth Korea National Health and Nutrition Examination Survey. Am J Rhinol Allergy. 2014; 28:e107–e114.
Article3. D'Amato G, Holgate ST, Pawankar R, Ledford DK, Cecchi L, Al-Ahmad M, et al. Meteorological conditions, climate change, new emerging factors, and asthma and related allergic disorders. A statement of the World Allergy Organization. World Allergy Organ J. 2015; 8:25.4. Shek LP, Lee BW. Food allergy in Asia. Curr Opin Allergy Clin Immunol. 2006; 6:197–201.
Article5. Oh JW, Pyun BY, Choung JT, Ahn KM, Kim CH, Song SW, et al. Epidemiological change of atopic dermatitis and food allergy in school-aged children in Korea between 1995 and 2000. J Korean Med Sci. 2004; 19:716–723.
Article6. Yang SH, Kim EJ, Kim YN, Seong KS, Kim SS, Han CK, et al. Comparison of eating habits and dietary intake patterns between people with and without allergy. Korean J Nutr. 2009; 42:523–535.
Article7. Osterballe M, Hansen TK, Mortz CG, Høst A, Bindslev-Jensen C. The prevalence of food hypersensitivity in an unselected population of children and adults. Pediatr Allergy Immunol. 2005; 16:567–573.
Article8. Pawankar R, Canonica GW, Holgate ST, Lockey RF, Blaiss MS. World Allergy Organization (WAO) White Book on Allergy: Update 2013. Milwaukee, WI: World Allergy Organization;2013.9. Sampson HA, Aceves S, Bock SA, James J, Jones S, Lang D, et al. Food allergy: a practice parameter update-2014. J Allergy Clin Immunol. 2014; 134:1016–1025.e43.10. Burks AW, Tang M, Sicherer S, Muraro A, Eigenmann PA, Ebisawa M, et al. ICON: food allergy. J Allergy Clin Immunol. 2012; 129:906–920.
Article11. Lee SH, Ban GY, Jeong K, Shin YS, Park HS, Lee S, et al. A retrospective study of Korean adults with food allergy: differences in phenotypes and causes. Allergy Asthma Immunol Res. 2017; 9:534–539.
Article12. Kim SR, Park HJ, Park KH, Lee JH, Park JW. IgE sensitization patterns to commonly consumed foods determined by skin prick test in Korean adults. J Korean Med Sci. 2016; 31:1197–1201.
Article13. Kim MA, Kim DK, Yang HJ, Yoo Y, Ahn Y, Park HS, et al. Pollen-food allergy syndrome in Korean pollinosis patients: a nationwide survey. Allergy Asthma Immunol Res. 2018; 10:648–661.
Article14. Kim JH, Kim SH, Park HW, Cho SH, Chang YS. Oral allergy syndrome in birch pollen-sensitized patients from a Korean university hospital. J Korean Med Sci. 2018; 33:e218.
Article15. Brownson RC, Gurney JG, Land GH. Evidence-based decision making in public health. J Public Health Manag Pract. 1999; 5:86–97.
Article16. Simons FE, Ardusso LR, Bilò MB, Dimov V, Ebisawa M, El-Gamal YM, et al. 2012 Update: World Allergy Organization Guidelines for the assessment and management of anaphylaxis. Curr Opin Allergy Clin Immunol. 2012; 12:389–399.17. Sampson HA, Aceves S, Bock SA, James J, Jones S, Lang D, et al. Food allergy: a practice parameter update-2014. J Allergy Clin Immunol. 2014; 134:1016–25.e43.18. Oh EJ, Lee SA, Lim J, Park YJ, Han K, Kim Y. Detection of allergen specific IgE by AdvanSure Allergy Screen test. Korean J Lab Med. 2010; 30:420–431.
Article19. Rim JH, Park BG, Kim JH, Kim HS. Comparison and clinical utility evaluation of four multiple allergen simultaneous tests including two newly introduced fully automated analyzers. Pract Lab Med. 2016; 4:50–61.
Article20. Park KH, Lee J, Lee SC, Son YW, Sim DW, Lee JH, et al. Comparison of the ImmunoCAP assay and AdvanSure™ AlloScreen advanced multiplex specific IgE detection assay. Yonsei Med J. 2017; 58:786–792.
Article21. Zuidmeer L, Goldhahn K, Rona RJ, Gislason D, Madsen C, Summers C, et al. The prevalence of plant food allergies: a systematic review. J Allergy Clin Immunol. 2008; 121:1210–1218.e4.
Article22. Kamdar TA, Peterson S, Lau CH, Saltoun CA, Gupta RS, Bryce PJ. Prevalence and characteristics of adult-onset food allergy. J Allergy Clin Immunol Pract. 2015; 3:114–115.e1.
Article23. Yang MS, Lee SH, Kim TW, Kwon JW, Lee SM, Kim SH, et al. Epidemiologic and clinical features of anaphylaxis in Korea. Ann Allergy Asthma Immunol. 2008; 100:31–36.
Article24. Kim SH, Kang HR, Kim KM, Kim TB, Kim SS, Chang YS, et al. The sensitization rates of food allergens in a Korean population: a multi-center study. J Asthma Allergy Clin Immunol. 2003; 23:502–514.25. Boyce JA, Assa'ad A, Burks AW, Jones SM, Sampson HA, Wood RA, et al. Guidelines for the diagnosis and management of food allergy in the United States: summary of the NIAID-sponsored expert panel report. Nutr Res. 2011; 31:61–75.
Article26. Han DK, Kim MK, Yoo JE, Choi SY, Kwon BC, Sohn MH, et al. Food sensitization in infants and young children with atopic dermatitis. Yonsei Med J. 2004; 45:803–809.
Article27. Lee SE, Kim H. Update on early nutrition and food allergy in children. Yonsei Med J. 2016; 57:542–548.
Article28. Muraro A, Werfel T, Hoffmann-Sommergruber K, Roberts G, Beyer K, Bindslev-Jensen C, et al. EAACI food allergy and anaphylaxis guidelines: diagnosis and management of food allergy. Allergy. 2014; 69:1008–1025.29. Boyce JA, Assa'ad A, Burks AW, Jones SM, Sampson HA, Wood RA, et al. Guidelines for the diagnosis and management of food allergy in the United States: summary of the NIAID-Sponsored Expert Panel report. J Am Acad Dermatol. 2011; 64:175–192.
Article30. Nowak-Węgrzyn A, Albin S. Oral immunotherapy for food allergy: mechanisms and role in management. Clin Exp Allergy. 2015; 45:368–383.
Article31. Vickery BP, Scurlock AM, Kulis M, Steele PH, Kamilaris J, Berglund JP, et al. Sustained unresponsiveness to peanut in subjects who have completed peanut oral immunotherapy. J Allergy Clin Immunol. 2014; 133:468–475.
Article32. Adkinson NF Jr, Bochner BS, Burks AW, Busse WW, Holgate ST, Lemanske RF, et al. Middleton's Allergy E-Book: Principles and Practice. Philadelphia, PA: Elsevier Health Sciences;2013.33. Nurmatov U, Dhami S, Arasi S, Pajno GB, Fernandez-Rivas M, Muraro A, et al. Allergen immunotherapy for IgE-mediated food allergy: a systematic review and meta-analysis. Allergy. 2017; 72:1133–1147.
Article34. Jeong KY, Son M, Park JH, Park KH, Park HJ, Lee JH, et al. Cross-reactivity between oak and birch pollens in Korean tree pollinosis. J Korean Med Sci. 2016; 31:1202–1207.
Article35. Kong N, Kim S, Lee SC, Park KH, Lee JH, Park JW. Subcutaneous immunotherapy in patients with Fagales pollen-induced oral allergy syndrome. Yonsei Med J. 2019; 60:389–394.
Article36. Rancé F, Kanny G, Dutau G, Moneret-Vautrin DA. Food hypersensitivity in children: clinical aspects and distribution of allergens. Pediatr Allergy Immunol. 1999; 10:33–38.
Article37. Gupta RS, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. 2011; 128:e9–e17.
Article38. Chung CH, Mirakhur B, Chan E, Le QT, Berlin J, Morse M, et al. Cetuximab-induced anaphylaxis and IgE specific for galactose-alpha-1,3-galactose. N Engl J Med. 2008; 358:1109–1117.39. Fischer J, Hebsaker J, Caponetto P, Platts-Mills TA, Biedermann T. Galactose-alpha-1,3-galactose sensitization is a prerequisite for pork-kidney allergy and cofactor-related mammalian meat anaphylaxis. J Allergy Clin Immunol. 2014; 134:755–759.e1.
Article40. Commins SP, James HR, Kelly LA, Pochan SL, Workman LJ, Perzanowski MS, et al. The relevance of tick bites to the production of IgE antibodies to the mammalian oligosaccharide galactose-α-1,3-galactose. J Allergy Clin Immunol. 2011; 127:1286–1293.e6.
Article