Kosin Med J.
2019 Jun;34(1):52-56. 10.7180/kmj.2019.34.1.52.
Advantages of Using Ultrasound in Regional Anesthesia for a Super-Super Obese Patient
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Dong-A University College of Medicine, Busan, Korea. parksy@dau.ac.kr
- KMID: 2451776
- DOI: http://doi.org/10.7180/kmj.2019.34.1.52
Abstract
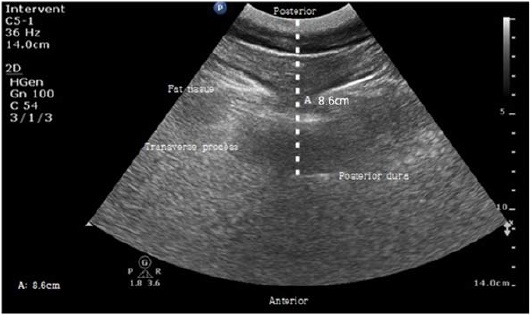
- In this case report, we describe the use of ultrasound in the administration regional anesthesia for a super-super obese patient. A 23-year-old female patient (height 167.2 cm, weight 191.5 kg, body mass index 68.6 kg/m²) was admitted to the hospital for surgical repair of an anterior talofibular ligament rupture. We used ultrasound to help facilitate the administration of regional anesthesia. In the sagittal view of the lumbar spine, (with the patient in a sitting position) we were able to identify the border between the sacrum and the lumbar vertebral; in the transverse view, we were able to identify the transverse process, posterior dura, vertebral body, and the distance from the skin to the posterior dura. After skin marking, regional anesthesia was successfully performed. Based on this case study, we suggest that ultrasound can be very useful in regional anesthesia for severely obese patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Mason EE, Doherty C, Maher JW, Scott DH, Rodriquez EM, Blommers TJ. Super obesity and gastric reduction procedures. Gastroenterol Clin North Am. 1987; 16:495–502.
Article2. Adams JP, Murphy PG. Obesity in anaesthesia and intensive care. Br J Anaesth. 2000; 85:91–108.
Article3. Shenkman Z, Shir Y, Brodsky JB. Perioperative management of the obese patient. Br J Anaesth. 1993; 70:349–359.
Article4. Brodsky JB. Perioperative management of the obese patient. Conferencias Magistrales. 2008; 31:S85–S89.5. Brodsky JB. Positioning the morbidly obese patient for anesthesia. Obes Surg. 2002; 12:751–758.
Article6. Sprung J, Bourke DL, Grass J, Hammel J, Mascha E, Thomas P, et al. Predicting the difficult neuraxial block: a prospective study. Anesth Analg. 1999; 89:384–389.7. Chin KJ, Perlas A, Chan V, Brown-Shreves D, Koshkin A, Vaishnav V. Ultrasound imaging facilitates spinal anesthesia in adults with difficult surface anatomic landmarks. Anesthesiology. 2011; 115:94–101.
Article8. Grau T, Leipold RW, Conradi R, Martin E, Motsch J. Ultrasound imaging facilitates localization of the epidural space during combined spinal and epidural anesthesia. Reg Anesth Pain Med. 2001; 26:64–67.
Article9. Cotter JT, Nielsen KC, Guller U, Steele SM, Klein SM, Greengrass RA, et al. Increased body mass index and ASA physical status IV are risk factors for block failure in ambulatory surgery—an analysis of 9,342 blocks. Can J Anaesth. 2004; 51:810–816.
Article10. Carty S, Nicholls B. Ultrasound-guided regional anaesthesia. Contin Educ Anaesth Crit Care Pain. 2007; 7:20–24.
Article11. Sahin T, Balaban O, Sahin L, Solak M, Toke K. A randomized controlled trial of preinsertion ultrasound guidance for spinal anaesthesia in pregnancy: outcomes among obese and lean parturients: ultrasound for spinal anesthesia in pregnancy. J Anesth. 2014; 28:413–419.
Article12. Turnbull DK, Shepherd DB. Post-dural puncture headache: pathogenesis, prevention and treatment. Br J Anaesth. 2003; 91:718–729.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- New Ultrasonographic Techniques to Differentiate Hepatic Masses: Contrast-Enhanced Ultrasound and Super-Resolution Ultrasound
- Daratumumab in dialysis-dependent multiple myeloma
- Avoiding Venous Anastomotic Dehiscence of an Arteriovenous Graft in a Super-Obese Patient
- A Case of Ingrown Toenails Treated by the Super Elastic Wire Insertion Method
- Can SUPER LIZER(R) Alleviate the Local Pain Induced by Caudal Puncture?