J Clin Neurol.
2019 Jul;15(3):347-352. 10.3988/jcn.2019.15.3.347.
Clinical Significance of Asymmetric Minimum Intensity Projection Images of Brain Magnetic Resonance Imaging in Children
- Affiliations
-
- 1Department of Pediatrics, Chonbuk National University Children's Hospital, Jeonju, Korea. sunjun@jbnu.ac.kr
- KMID: 2451119
- DOI: http://doi.org/10.3988/jcn.2019.15.3.347
Abstract
- BACKGROUND AND PURPOSE
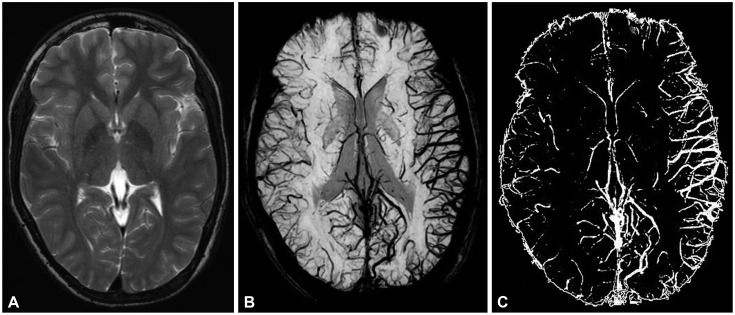
The susceptibility-weighted imaging form of brain MRI using minimum intensity projection (mIP) is useful for assessing traumatic brain injuries because it readily reveals deoxyhemoglobin or paramagnetic compounds. We investigated the efficacy of using this methodology in nontraumatic patients.
METHODS
We retrospectively analyzed the asymmetric mIP findings in nontraumatic patients. Asymmetric mIP images were first verified visually and then using ImageJ software. We enrolled patients with a difference of >5% between hemispheres in ImageJ analysis. All patients underwent detailed history-taking and EEG, and asymmetric mIP findings were compared.
RESULTS
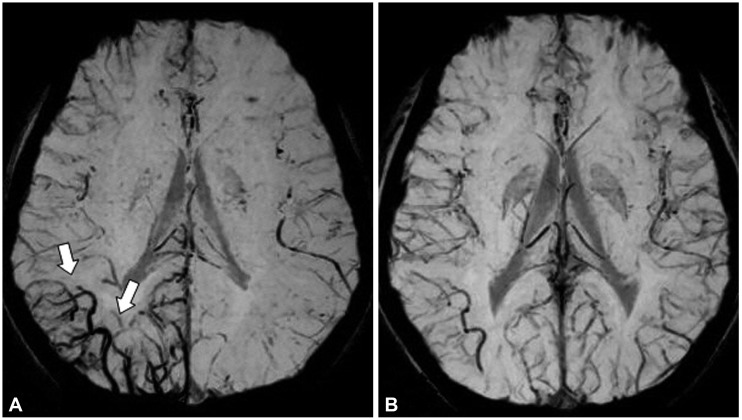
The visual analysis identified 54 pediatric patients (37 males and 17 females) with asymmetric mIP findings. Ten patients were excluded because they did not meet the ImageJ verification criteria. The 44 patients with asymmetry comprised 36 with epilepsy, 6 with headache, and 2 with cerebral infarction. Thirty-one of the 36 epileptic patients showed definite partial seizure activities in semiology, while the remaining patients did not demonstrate a history of partial seizure manifestations. The MRI findings were normal in all patients except for five with periventricular leukomalacia unrelated to seizure symptoms. There was agreement between mIP images and semiology in 29 (93.5%) of the 31 epileptic patients with focal signs, while the other 2 demonstrated discordance. Twenty (64.5%) of the 31 patients showed consistent EEG abnormalities.
CONCLUSIONS
Our data suggest that asymmetric mIP findings are an excellent lateralizing indicator in pediatric patients with partial epilepsy.
MeSH Terms
Figure
Reference
-
1. Liu C, Li W, Tong KA, Yeom KW, Kuzminski S. Susceptibility-weighted imaging and quantitative susceptibility mapping in the brain. J Magn Reson Imaging. 2015; 42:23–41. PMID: 25270052.
Article2. Ogawa S, Lee TM. Magnetic resonance imaging of blood vessels at high fields: in vivo and in vitro measurements and image simulation. Magn Reson Med. 1990; 16:9–18. PMID: 2255240.3. Elnekeidy AE, Yehia A, Elfatatry A. Importance of susceptibility weighted imaging (SWI) in management of cerebro-vascular strokes (CVS). Alexandria J Med. 2014; 50:83–91.
Article4. Soman S, Holdsworth SJ, Barnes PD, Rosenberg J, Andre JB, Bammer R, et al. Improved T2* imaging without increase in scan time: SWI processing of 2D gradient echo. AJNR Am J Neuroradiol. 2013; 34:2092–2097. PMID: 23744690.
Article5. Hingwala D, Kesavadas C, Thomas B, Kapilamoorthy TR. Clinical utility of susceptibility-weighted imaging in vascular diseases of the brain. Neurol India. 2010; 58:602–607. PMID: 20739803.
Article6. Haacke EM, Makki M, Ge Y, Maheshwari M, Sehgal V, Hu J, et al. Characterizing iron deposition in multiple sclerosis lesions using susceptibility weighted imaging. J Magn Reson Imaging. 2009; 29:537–544. PMID: 19243035.
Article7. Tong KA, Ashwal S, Obenaus A, Nickerson JP, Kido D, Haacke EM. Susceptibility-weighted MR imaging: a review of clinical applications in children. AJNR Am J Neuroradiol. 2008; 29:9–17. PMID: 17925363.
Article8. King MA, Newton MR, Jackson GD, Fitt GJ, Mitchell LA, Silvapulle MJ, et al. Epileptology of the first-seizure presentation: a clinical, electroencephalographic, and magnetic resonance imaging study of 300 consecutive patients. Lancet. 1998; 352:1007–1011. PMID: 9759742.
Article9. Liu RS, Lemieux L, Bell GS, Sisodiya SM, Bartlett PA, Shorvon SD, et al. The structural consequences of newly diagnosed seizures. Ann Neurol. 2002; 52:573–580. PMID: 12402254.
Article10. Hakami T, McIntosh A, Todaro M, Lui E, Yerra R, Tan KM, et al. MRI-identified pathology in adults with new-onset seizures. Neurology. 2013; 81:920–927. PMID: 23925763.
Article11. Shinnar S, Kang H, Berg AT, Goldensohn ES, Hauser WA, Moshé SL. EEG abnormalities in children with a first unprovoked seizure. Epilepsia. 1994; 35:471–476. PMID: 8026390.
Article12. Vallejo-Illarramendi A, Marciano DK, Reichardt LF. A novel method that improves sensitivity of protein detection in PAGE and Western blot. Electrophoresis. 2013; 34:1148–1150. PMID: 23400834.
Article13. Pohlmann-Eden B, Newton M. First seizure: EEG and neuroimaging following an epileptic seizure. Epilepsia. 2008; 49(Suppl 1):19–25.
Article14. Shinnar S, O'Dell C, Mitnick R, Berg AT, Moshe SL. Neuroimaging abnormalities in children with an apparent first unprovoked seizure. Epilepsy Res. 2001; 43:261–269. PMID: 11248538.
Article15. Devous MD Sr, Thisted RA, Morgan GF, Leroy RF, Rowe CC. SPECT brain imaging in epilepsy: a meta-analysis. J Nucl Med. 1998; 39:285–293. PMID: 9476937.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Advanced Magnetic Resonance Imaging for Pediatric Brain Tumors: Current Imaging Techniques and Interpretation Algorithms
- A Projection-based Intensity Correction Method of Phased-Array Coil Images
- Diffusion-Weighted Imaging of Brain Injury Due to Neonatal Hypoglycemia: A Case Report
- MRCP Using Breath-hold HASTE Sequence: Comparison of Maximum Intensity Projection Image with Single Slice Acquisition Image
- A Case of Metronidazole-Induced Encephalopathy: Atypical Involvement of the Brain on MRI