Blood Res.
2019 Mar;54(1):38-44. 10.5045/br.2019.54.1.38.
Microcytosis in children and adolescents with the sickle cell trait in Basra, Iraq
- Affiliations
-
- 1Center for Hereditary Blood Diseases, Basrah Heath Directorate, Basrah, Iraq. alasfoor_mk@yahoo.com
- 2Department of Pediatrics, College of Medicine, University of Basrah, Basrah, Iraq.
- KMID: 2451054
- DOI: http://doi.org/10.5045/br.2019.54.1.38
Abstract
- BACKGROUND
Microcytic anemia, the most common form of anemia in children and adolescents, is a heterogeneous group of diseases that is acquired or inherited. We assessed the frequency and causes of microcytosis in children and adolescents with the sickle cell trait (SCT).
METHODS
This descriptive study included 95 subjects (49 males and 46 females) with SCT who attended Basra Center for Hereditary Blood Diseases for evaluation. Investigations included complete blood count, high performance liquid chromatography, capillary electrophoresis, and measurement of serum ferritin and transferrin levels.
RESULTS
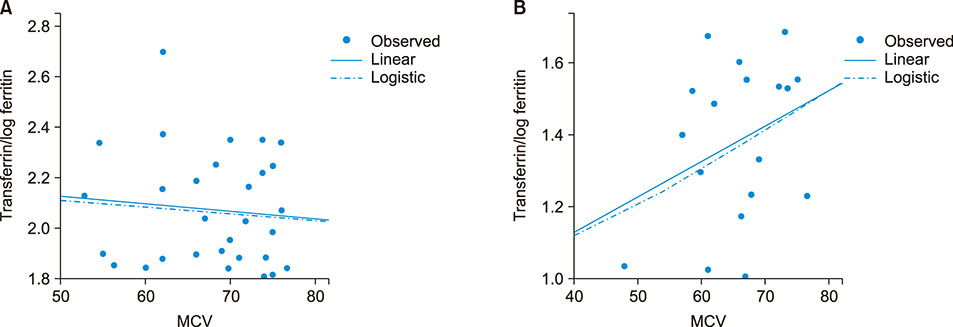
SCT subjects had a low hemoglobin (Hb) concentration (9.79±1.75 g/dL), low mean corpuscular volume (MCV, 67.43±9.22), low mean corpuscular Hb (21.15±3.64), and a normal red cell distribution width (RDW, 14.00±2.30). Among 95 SCT subjects, 81 (85.26%) had microcytosis, 12 (12.63%) had normal MCV, and 2 (2.11%) exhibited macrocytosis. Sixty-three (77.78%) SCT subjects with microcytosis were iron deficient, and 18 (22.22%) had normal iron levels. The mean serum ferritin and HbA2 levels were significantly lower, while the RDW, sickle Hb, and serum transferrin levels were significantly higher in patients with microcytosis and iron deficiency compared to non-iron deficient subjects (P<0.05). Correlation coefficients did not reveal a significant association between the MCV and iron status of SCT subjects (P>0.05).
CONCLUSION
Despite the frequent occurrence of iron deficiency in SCT subjects, co-inheritance of alpha-thalassemia seemed to be the cause of low MCV in non-iron deficient individuals with microcytosis. Genetic analysis is required to understand the genetic basis of this phenomenon.
Keyword
MeSH Terms
Figure
Reference
-
1. Tsaras G, Owusu-Ansah A, Boateng FO, Amoateng-Adjepong Y. Complications associated with sickle cell trait: a brief narrative review. Am J Med. 2009; 122:507–512.
Article2. Naik RP, Haywood C Jr. Sickle cell trait diagnosis: clinical and social implications. Hematology Am Soc Hematol Educ Program. 2015; 2015:160–167.
Article3. Key NS, Derebail VK. Sickle-cell trait: novel clinical significance. Hematology Am Soc Hematol Educ Program. 2010; 2010:418–422.
Article4. Hassan MK, Taha JY, Al-Naama LM, Widad NM, Jasim SN. Frequency of haemoglobinopathies and glucose-6-phosphate dehydrogenase deficiency in Basra. East Mediterr Health J. 2003; 9:45–54.
Article5. Al-Allawi NA, Al-Dousky AA. Frequency of haemoglobinopathies at premarital health screening in Dohuk, Iraq: implications for a regional prevention programme. East Mediterr Health J. 2010; 16:381–385.
Article6. Iolascon A, De Falco L, Beaumont C. Molecular basis of inherited microcytic anemia due to defects in iron acquisition or heme synthesis. Haematologica. 2009; 94:395–408.
Article7. Miller JL. Iron deficiency anemia: a common and curable disease. Cold Spring Harb Perspect Med. 2013; 3:a011866.
Article8. World Health Organization. The global prevalence of anaemia in 2011. Geneva, Switzerland: World Health Organization;2015. p. 4–5.9. Iraqi Ministry of Health. Nutrition Research Institute Iraq 2014. Baghdad, Iraq: Iraqi Ministry of Health;2014. Accessed February 15, 2016. at http://www.ffinetwork.org/about/calendar/2014/documents/QIraq2014.pdf.10. Medinger M, Saller E, Harteveld CL, et al. A rare case of coinheritance of Hemoglobin H disease and sickle cell trait combined with severe iron deficiency. Hematol Rep. 2011; 3:e30.
Article11. Wambua S, Mwacharo J, Uyoga S, Macharia A, Williams TN. Co-inheritance of alpha+-thalassaemia and sickle trait results in specific effects on haematological parameters. Br J Haematol. 2006; 133:206–209.
Article12. World Health Organization. WHO child growth standards. Geneva, Switzerland: World Health Organization;2006. Accessed March 22, 2016. at https://www.who.int/childgrowth/publications/technical_report_pub/en/.13. Cole TJ, Flegal KM, Nicholls D, Jackson AA. Body mass index cut offs to define thinness in children and adolescents: international survey. BMJ. 2007; 335:194.
Article14. Lewis SM. Reference ranges and normal values. In : Lewis SM, Bain BJ, Bates I, editors. Dacie and Lewis practical haematology. 10th ed. Philadelphia, PA: Churchill Livingstone;2006. p. 11–24.15. Lo SF. Reference intervals for laboratory tests and procedures. In : Kliegman RM, Stanton BF, St Geme JW, Schor N, editors. Nelson textbook of pediatrics. 20th ed. Philadelphia, PA: Elsevier;2016. p. 3464–3473.16. Castel R, Tax MG, Droogendijk J, et al. The transferrin/log(ferritin) ratio: a new tool for the diagnosis of iron deficiency anemia. Clin Chem Lab Med. 2012; 50:1343–1349.
Article17. Obaid AJ, Hassan MK, AL-Naama LM. Sickle cell and glucose-6-phosphate dehydrogenase deficiency gene in Abu-Alkhasib district of southern Iraq. Med J Basrah Univ. 2001; 19:12–18.18. Chikhlikar K, Wilkinson A. A study of red cell parameters in patients of sickle cell trait. IOSR J Dent Med Sci. 2014; 13:46–50.
Article19. Mustafa MH, Eltayeb EA, Elmisbah TE, Babiker HM, Ali NA, Nasir O. Frequency of the sickle cell disease and sickle cell trait in Heglig Area-Sudan. Int J Public Health Epidemiol. 2013; 3:1–6.20. Patel J, Patel A, Patel J, Kaur A, Patel V. Prevalence of haemoglobinopathies in Gujarat, India: a cross-sectional study. Internet J Hematol. 2008; 5:1–6.21. Mohanty D, Mukherjee MB, Colah RB, et al. Iron deficiency anaemia in sickle cell disorders in India. Indian J Med Res. 2008; 127:366–369.22. Khan Y, Thakur AS, Mehta R, Kundu RK, Agnihotram G. Hematological profile of sickle cell disease: a hospital based study at cims, Bilaspur, Chhattisgarh. Int J Appl Biol Pharm. 2010; 1:717–721.23. El Ariss AB, Younes M, Matar J, Berjaoui Z. Prevalence of sickle cell trait in the Southern Suburb of Beirut, Lebanon. Mediterr J Hematol Infect Dis. 2016; 8:e2016015.24. Tawfeeq U. Iraq National Micronutrient Survey 2007. Baghdad, Iraq: Iraqi Ministry of Health;2007. Accessed March 5, 2016. at https://studylib.net/doc/7795821/iraq-national-micronutrientsurvey-2007.25. Domellöf M, Lönnerdal B, Dewey KG, Cohen RJ, Rivera LL, Hernell O. Sex differences in iron status during infancy. Pediatrics. 2002; 110:545–552.
Article26. Musaiger AO, Al-Mufty BA, Al-Hazzaa HM. Eating habits, inactivity, and sedentary behavior among adolescents in Iraq: sex differences in the hidden risks of noncommunicable diseases. Food Nutr Bull. 2014; 35:12–19.
Article27. Modell B, Darlison M. Global epidemiology of haemoglobin disorders and derived service indicators. Bull World Health Organ. 2008; 86:480–487.
Article28. Sultana GS, Haque SA, Sultana T, Ahmed AN. Value of red cell distribution width (RDW) and RBC indices in the detection of iron deficiency anemia. Mymensingh Med J. 2013; 22:370–376.29. Al-Harbi T, Al-Matrafi M, Ismail A. Prevalence & etiology of microcytosis in sickle cell anemia patients. Imp J Interdiscip Res. 2016; 2:622–626.30. Taha JY, Mansour AA. Level of hemoglobin in sickle cell trait in Basrah using HPLC. Middle East J Fam Med. 2006; 4:15–16.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A challenging diagnosis of hepatosplenic T cell lymphoma in a 10-year-old child
- Pitfalls of Measuring Hemoglobin A1c in a Patient with Sickle Cell Trait in South Korea
- Translocation Renal Cell Carcinoma t(6;11)(p21;q12) and Sickle Cell Anemia: First Report and Review of the Literature
- Effective sickle hemoglobin reduction by automated red cell exchange using Spectra Optia in three Emirati patients with sickle cell disease before allogeneic hematopoietic stem cell transplantation
- Salmonella Typhi Osteomyelitis in a Non-sickle Cell Patient: Three Cases Report