Infect Chemother.
2019 Jun;51(2):217-243. 10.3947/ic.2019.51.2.217.
Guideline for the Antibiotic Use in Acute Gastroenteritis
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 2Division of Infectious Diseases, Department of Internal Medicine, Kyung Hee University Hospital, Kyung Hee University School of Medicine, Seoul, Korea.
- 3Division of Healthcare Technology Assessment Research, National Evidence-Based Healthcare Collaborating Agency, Seoul, Korea.
- 4Department of Laboratory Medicine, Daejeon St. Mary's hospital, College of Medicine, The Catholic University of Korea, Daejeon, Korea.
- 5Division of Gastroenterology, Department of Internal Medicine, Inha University College of Medicine, Incheon, Korea.
- 6Division of Infectious Diseases, Department of Internal Medicine, Hallym University Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea.
- 7Division of Infectious Diseases, Department of Internal Medicine, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea.
- 8Division of Infectious Diseases, Department of Internal Medicine, Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea. yrkim@catholic.ac.kr
- 9Division of Infectious Diseases, Department of Internal Medicine, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- KMID: 2450880
- DOI: http://doi.org/10.3947/ic.2019.51.2.217
Abstract
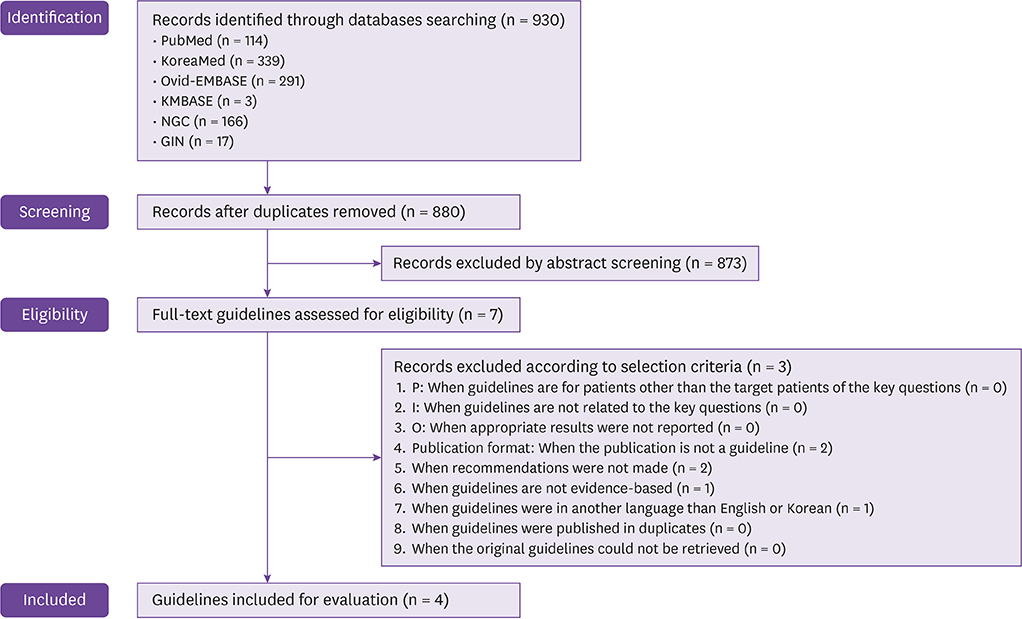
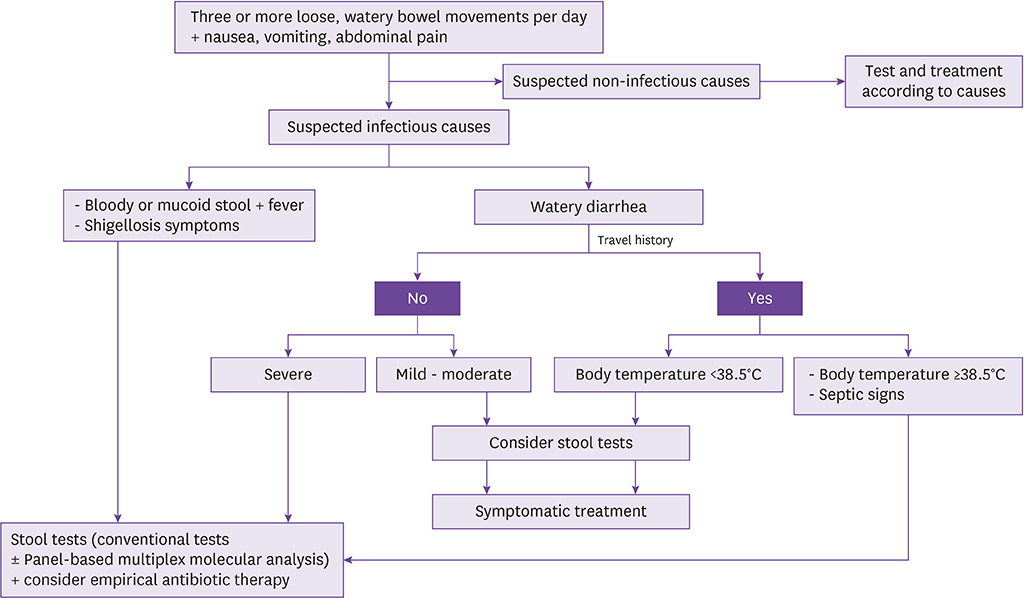
- Acute gastroenteritis is common infectious disease in community in adults. This work represents an update of "˜Clinical guideline for the diagnosis and treatment of gastrointestinal infections' that was developed domestically in 2010. The recommendation of this guideline was developed regarding the following; epidemiological factors, test for diagnosis, the indications of empirical antibiotics, and modification of antibiotics after confirming pathogen. Ultimately, it is expected to decrease antibiotic misuse and prevent antibiotic resistance.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Prescription of Antibiotics for Adults with Acute Infectious Diarrhea in Korea: A Population-based Study
Hyo-Jin Lee, Ki-Ho Park, Dong-Ah Park, Joonhong Park, Byoung Wook Bang, Seung Soon Lee, Eun Jung Lee, Youn Jeong Kim, Sung Kwan Hong, Yang Ree Kim
Infect Chemother. 2019;51(3):295-304. doi: 10.3947/ic.2019.51.3.295.Diagnostic value of serum procalcitonin and C-reactive protein in discriminating between bacterial and nonbacterial colitis: a retrospective study
Jae Yong Lee, So Yeon Lee, Yoo Jin Lee, Jin Wook Lee, Jeong Seok Kim, Ju Yup Lee, Byoung Kuk Jang, Woo Jin Chung, Kwang Bum Cho, Jae Seok Hwang
J Yeungnam Med Sci. 2023;40(4):388-393. doi: 10.12701/jyms.2023.00059.
Reference
-
1. Korea Centers for Disease Control and Prevention (KCDC). Infectious diseases surveillance yearbook, 2017. Accessed 20 December 2018. Available at: http://www.cdc.go.kr/npt/biz/npp/portal/nppPblctDtaMain.do? pblctDtaSeAt=1.2. Dewey-Mattia D, Manikonda K, Hall AJ, Wise ME, Crowe SJ. Surveillance for foodborne disease outbreaks-United States, 2009-2015. MMWR Surveill Summ. 2018; 67:1–11.3. Crump JA, Luby SP, Mintz ED. The global burden of typhoid fever. Bull World Health Organ. 2004; 82:346–353.4. Kim S. Salmonella serovars from foodborne and waterborne diseases in Korea, 1998-2007: total isolates decreasing versus rare serovars emerging. J Korean Med Sci. 2010; 25:1693–1699.
Article5. Yoo S, Pai H, Byeon JH, Kang YH, Kim S, Lee BK. Epidemiology of Salmonella enterica serotype typhi infections in Korea for recent 9 years: trends of antimicrobial resistance. J Korean Med Sci. 2004; 19:15–20.
Article6. Koh SJ, Cho HG, Kim BH, Choi BY. An outbreak of gastroenteritis caused by norovirus-contaminated groundwater at a waterpark in Korea. J Korean Med Sci. 2011; 26:28–32.
Article7. The Korean Society of Infectious Diseases, Korean Society for Chemotherapy, The Korean Society of Clinical Microbiology. Clinical guideline for the diagnosis and treatment of gastrointestinal infections. Infect Chemother. 2010; 42:323–361.8. DuPont HL. Clinical practice. Bacterial diarrhea. N Engl J Med. 2009; 361:1560–1569.9. Korea Centers for Disease Control and Prevention (KCDC). Infectious disease portal. Accessed 20 December 2018. Available at: http://www.cdc.go.kr/npt/biz/npp/ist/bass/bassDissStatsMain.do.10. Wu CJ, Hsueh PR, Ko WC. A new health threat in Europe: Shiga toxin-producing Escherichia coli O104:H4 infections. J Microbiol Immunol Infect. 2011; 44:390–393.
Article11. Frank C, Werber D, Cramer JP, Askar M, Faber M, an der Heiden M, Bernard H, Fruth A, Prager R, Spode A, Wadl M, Zoufaly A, Jordan S, Kemper MJ, Follin P, Müller L, King LA, Rosner B, Buchholz U, Stark K, Krause G. HUS Investigation Team. Epidemic profile of Shiga-toxin-producing Escherichia coli O104:H4 outbreak in Germany. N Engl J Med. 2011; 365:1771–1780.
Article12. Rangel JM, Sparling PH, Crowe C, Griffin PM, Swerdlow DL. Epidemiology of Escherichia coli O157:H7 outbreaks, United States, 1982-2002. Emerg Infect Dis. 2005; 11:603–609.
Article13. Kim MJ, Kim SH, Kim TS, Kee HY, Seo JJ, Kim ES, Park JT, Chung JK, Lee J. Identification of shiga toxin-producing E. coli isolated from diarrhea patients and cattle in Gwangju area, Korea. J Bacteriol Virol. 2009; 39:29–39.
Article14. Mody RK, Luna-Gierke RE, Jones TF, Comstock N, Hurd S, Scheftel J, Lathrop S, Smith G, Palmer A, Strockbine N, Talkington D, Mahon BE, Hoekstra RM, Griffin PM. Infections in pediatric postdiarrheal hemolytic uremic syndrome: factors associated with identifying shiga toxin-producing Escherichia coli . Arch Pediatr Adolesc Med. 2012; 166:902–909.
Article15. Croxen MA, Law RJ, Scholz R, Keeney KM, Wlodarska M, Finlay BB. Recent advances in understanding enteric pathogenic Escherichia coli . Clin Microbiol Rev. 2013; 26:822–880.
Article16. Tarr PI, Gordon CA, Chandler WL. Shiga-toxin-producing Escherichia coli and haemolytic uraemic syndrome. Lancet. 2005; 365:1073–1086.17. Centers for Disease Control and Prevention (CDC). Traveler's health: travelers' diarrhea. Accessed 20 December 2018. Available at: https://wwwnc.cdc.gov/travel/yellowbook/2018/the-pre-travel-consultation/travelers-diarrhea.18. Slutsker L, Ries AA, Greene KD, Wells JG, Hutwagner L, Griffin PM. Escherichia coli O157:H7 diarrhea in the United States: clinical and epidemiologic features. Ann Intern Med. 1997; 126:505–513.
Article19. Mutsch M, Pitzurra R, Hatz C, Steffen R. Post-infectious sequelae of travelers' diarrhea: irritable bowel syndrome. J Travel Med. 2014; 21:141–143.
Article20. Connor BA. Sequelae of traveler's diarrhea: focus on postinfectious irritable bowel syndrome. Clin Infect Dis. 2005; 41:Suppl 8. S577–S586.
Article21. Koh SJ, Lee DH, Lee SH, Park YS, Hwang JH, Kim JW, Jeong SH, Kim N, Im JP, Kim JS, Jung HC. Incidence and risk factors of irritable bowel syndrome in community subjects with culture-proven bacterial gastroenteritis. Korean J Gastroenterol. 2012; 60:13–18.
Article22. McAuliffe GN, Anderson TP, Stevens M, Adams J, Coleman R, Mahagamasekera P, Young S, Henderson T, Hofmann M, Jennings LC, Murdoch DR. Systematic application of multiplex PCR enhances the detection of bacteria, parasites, and viruses in stool samples. J Infect. 2013; 67:122–129.
Article23. Amrud K, Slinger R, Sant N, Desjardins M, Toye B. A comparison of the Allplex™ bacterial and viral assays to conventional methods for detection of gastroenteritis agents. BMC Res Notes. 2018; 11:514.
Article24. Cybulski RJ Jr, Bateman AC, Bourassa L, Bryan A, Beail B, Matsumoto J, Cookson BT, Fang FC. Clinical impact of a multiplex gastrointestinal polymerase chain reaction panel in patients with acute gastroenteritis. Clin Infect Dis. 2018; 67:1688–1696.
Article25. Zhou Y, Zhu X, Hou H, Lu Y, Yu J, Mao L, Mao L, Sun Z. Characteristics of diarrheagenic Escherichia coli among children under 5 years of age with acute diarrhea: a hospital based study. BMC Infect Dis. 2018; 18:63.
Article26. Thakur N, Jain S, Changotra H, Shrivastava R, Kumar Y, Grover N, Vashistt J. Molecular characterization of diarrheagenic Escherichia coli pathotypes: association of virulent genes, serogroups, and antibiotic resistance among moderate-to-severe diarrhea patients. J Clin Lab Anal. 2018; 32:e22388.27. Kim SH, Shin JH. Point-of-care diagnostics for infectious diseases: present and future. Korean J Med. 2018; 93:181–187.
Article28. Ramanan P, Bryson AL, Binnicker MJ, Pritt BS, Patel R. Syndromic panel-based testing in clinical microbiology. Clin Microbiol Rev. 2018; 31:pii:e00024–17.
Article29. Shane AL, Mody RK, Crump JA, Tarr PI, Steiner TS, Kotloff K, Langley JM, Wanke C, Warren CA, Cheng AC, Cantey J, Pickering LK. 2017 Infectious Diseases Society of America clinical practice guidelines for the diagnosis and management of infectious diarrhea. Clin Infect Dis. 2017; 65:e45–80.
Article30. Parry CM, Hien TT, Dougan G, White NJ, Farrar JJ. Typhoid fever. N Engl J Med. 2002; 347:1770–1782.
Article31. Bhan MK, Bahl R, Bhatnagar S. Typhoid and paratyphoid fever. Lancet. 2005; 366:749–762.
Article32. Crump JA, Medalla FM, Joyce KW, Krueger AL, Hoekstra RM, Whichard JM, Barzilay EJ. Emerging Infections Program NARMS Working Group. Antimicrobial resistance among invasive nontyphoidal Salmonella enterica isolates in the United States: National Antimicrobial Resistance Monitoring System, 1996 to 2007. Antimicrob Agents Chemother. 2011; 55:1148–1154.
Article33. Angulo FJ, Swerdlow DL. Bacterial enteric infections in persons infected with human immunodeficiency virus. Clin Infect Dis. 1995; 21:Suppl 1. S84–S93.
Article34. Keddy KH, Sooka A, Crowther-Gibson P, Quan V, Meiring S, Cohen C, Nana T, Sriruttan C, Seetharam S, Hoosen A, Naicker P, Elliott E, Haffejee S, Whitelaw A, Klugman KP. Group for Enteric, Respiratory, and Meningeal Disease Surveillance in South Africa (GERMS-SA). Systemic shigellosis in South Africa. Clin Infect Dis. 2012; 54:1448–1454.
Article35. Cover TL, Aber RC. Yersinia enterocolitica. N Engl J Med. 1989; 321:16–24.
Article36. Haq SM, Dayal HH. Chronic liver disease and consumption of raw oysters: a potentially lethal combination--a review of Vibrio vulnificus septicemia. Am J Gastroenterol. 2005; 100:1195–1199.
Article37. Lee A, Mirrett S, Reller LB, Weinstein MP. Detection of bloodstream infections in adults: how many blood cultures are needed? J Clin Microbiol. 2007; 45:3546–3548.
Article38. Olopoenia LA, King AL. Widal agglutination test - 100 years later: still plagued by controversy. Postgrad Med J. 2000; 76:80–84.39. House D, Wain J, Ho VA, Diep TS, Chinh NT, Bay PV, Vinh H, Duc M, Parry CM, Dougan G, White NJ, Hien TT, Farrar JJ. Serology of typhoid fever in an area of endemicity and its relevance to diagnosis. J Clin Microbiol. 2001; 39:1002–1007.
Article40. Waddington CS, Darton TC, Pollard AJ. The challenge of enteric fever. J Infect. 2014; 68:Suppl 1. S38–S50.
Article41. Holtz LR, Neill MA, Tarr PI. Acute bloody diarrhea: a medical emergency for patients of all ages. Gastroenterology. 2009; 136:1887–1898.
Article42. Lopes RJ, Almeida J, Dias PJ, Pinho P, Maciel MJ. Infectious thoracic aortitis: a literature review. Clin Cardiol. 2009; 32:488–490.
Article43. Karachalios G, Bablekos G, Karachaliou G, Charalabopoulos AK, Charalabopoulos K. Infectious endocarditis due to Yersinia enterocolitica. Chemotherapy. 2002; 48:158–159.
Article44. Hagiya H, Matsumoto M, Furukawa H, Murase T, Otsuka F. Mycotic abdominal aortic aneurysm caused by Campylobacter fetus: a case report and literature review. Ann Vasc Surg. 2014; 28:1933.e7–1933.14.45. Plastaras L, Vuitton L, Badet N, Koch S, Di Martino V, Delabrousse E. Acute colitis: differential diagnosis using multidetector CT. Clin Radiol. 2015; 70:262–269.
Article46. Horiki N, Maruyama M, Fujita Y, Suzuki Y, Tanaka T, Imoto I, Adachi Y. CT evaluation of infectious colitis. Nihon Shokakibyo Gakkai Zasshi. 2002; 99:925–934.47. Macari M, Balthazar EJ. CT of bowel wall thickening: significance and pitfalls of interpretation. AJR Am J Roentgenol. 2001; 176:1105–1116.48. Thoeni RF, Cello JP. CT imaging of colitis. Radiology. 2006; 240:623–638.
Article49. Riddle MS, DuPont HL, Connor BA. ACG clinical guideline: diagnosis, treatment, and prevention of acute diarrheal infections in adults. Am J Gastroenterol. 2016; 111:602–622.
Article50. DuPont HL. Acute infectious diarrhea in immunocompetent adults. N Engl J Med. 2014; 370:1532–1540.
Article51. Surawicz CM, Belic L. Rectal biopsy helps to distinguish acute self-limited colitis from idiopathic inflammatory bowel disease. Gastroenterology. 1984; 86:104–113.
Article52. Waye JD. Differentiation of inflammatory bowel conditions by endoscopy and biopsy. Endoscopy. 1992; 24:551–554.
Article53. ASGE Standards of Practice Committee. Shen B, Khan K, Ikenberry SO, Anderson MA, Banerjee S, Baron T, Ben-Menachem T, Cash BD, Fanelli RD, Fisher L, Fukami N, Gan SI, Harrison ME, Jagannath S, Lee Krinsky M, Levy M, Maple JT, Lichtenstein D, Stewart L, Strohmeyer L, Dominitz JA. The role of endoscopy in the management of patients with diarrhea. Gastrointest Endosc. 2010; 71:887–892.
Article54. Barbut F, Beaugerie L, Delas N, Fossati-Marchal S, Aygalenq P, Petit JC. Infectious Colitis Study Group. Comparative value of colonic biopsy and intraluminal fluid culture for diagnosis of bacterial acute colitis in immunocompetent patients. Clin Infect Dis. 1999; 29:356–360.
Article55. Goka AK, Rolston DD, Mathan VI, Farthing MJ. The relative merits of faecal and duodenal juice microscopy in the diagnosis of giardiasis. Trans R Soc Trop Med Hyg. 1990; 84:66–67.
Article56. Wahnschaffe U, Ignatius R, Loddenkemper C, Liesenfeld O, Muehlen M, Jelinek T, Burchard GD, Weinke T, Harms G, Stein H, Zeitz M, Ullrich R, Schneider T. Diagnostic value of endoscopy for the diagnosis of giardiasis and other intestinal diseases in patients with persistent diarrhea from tropical or subtropical areas. Scand J Gastroenterol. 2007; 42:391–396.
Article57. Goka AK, Rolston DD, Mathan VI, Farthing MJ. Diagnosis of Strongyloides and hookworm infections: comparison of faecal and duodenal fluid microscopy. Trans R Soc Trop Med Hyg. 1990; 84:829–831.
Article58. De Bruyn G, Hahn S, Borwick A. Antibiotic treatment for travellers' diarrhoea. Cochrane Database Syst Rev. 2000; CD002242.
Article59. Riddle MS, Connor BA, Beeching NJ, DuPont HL, Hamer DH, Kozarsky P, Libman M, Steffen R, Taylor D, Tribble DR, Vila J, Zanger P, Ericsson CD. Guidelines for the prevention and treatment of travelers' diarrhea: a graded expert panel report. J Travel Med. 2017; 24:suppl_1. S57–S74.
Article60. Libman M. CATMAT. Summary of the Committee to Advise on Tropical Medicine and Travel (CATMAT) statement on travellers' diarrhea. Can Commun Dis Rep. 2015; 41:272–284.
Article61. DuPont HL, Ericsson CD, Farthing MJ, Gorbach S, Pickering LK, Rombo L, Steffen R, Weinke T. Expert review of the evidence base for self-therapy of travelers' diarrhea. J Travel Med. 2009; 16:161–171.
Article62. Bartels C, Beaute J, Fraser G, de Jong B, Urtaza J, Nicols G, Niskanen T, Palm D, Robesyn E, Severi E, Tavoschi L, Varela Santos C, Van Walle I, Warns-Petit E, Westrell T, Whittaker R. Annual epidemiological report 2014: food- and waterborne diseases and zoonoses. Stockholm: ECDC;2014.63. Eurosurveillance editorial team. European Union Summary Report on antimicrobial resistance in zoonotic and indicator bacteria from humans, animals and food 2012 published. Euro Surveill. 2014; 19:20748.64. Zaidi MB, McDermott PF, Campos FD, Chim R, Leon M, Vazquez G, Figueroa G, Lopez E, Contreras J, Estrada-Garcia T. Antimicrobial-resistant Campylobacter in the food chain in Mexico. Foodborne Pathog Dis. 2012; 9:841–847.65. Serichantalergs O, Pootong P, Dalsgaard A, Bodhidatta L, Guerry P, Tribble DR, Anuras S, Mason CJ. PFGE, Lior serotype, and antimicrobial resistance patterns among Campylobacter jejuni isolated from travelers and US military personnel with acute diarrhea in Thailand, 1998-2003. Gut Pathog. 2010; 2:15.
Article66. Kim NO, Jung SM, Na HY, Chung GT, Yoo CK, Seong WK, Hong S. Enteric bacteria isolated from diarrheal patients in Korea in 2014. Osong Public Health Res Perspect. 2015; 6:233–240.
Article67. Cho IJ, Yim J, Lee Y, Kim MS, Seo Y, Chung HS, Yong D, Jeong SH, Lee K, Chong Y. Trends in isolation and antimicrobial susceptibility of enteropathogenic bacteria in 2001-2010 at a Korean tertiary care hospital. Ann Clin Microbiol. 2013; 16:45–51.
Article68. Infante RM, Ericsson CD, Jiang ZD, Ke S, Steffen R, Riopel L, Sack DA, DuPont HL. Enteroaggregative Escherichia coli diarrhea in travelers: response to rifaximin therapy. Clin Gastroenterol Hepatol. 2004; 2:135–138.
Article69. Riddle MS, Connor P, Fraser J, Porter CK, Swierczewski B, Hutley EJ, Danboise B, Simons MP, Hulseberg C, Lalani T, Gutierrez RL, Tribble DR. TrEAT TD Study Team. Trial Evaluating Ambulatory Therapy of Travelers' Diarrhea (TrEAT TD) study: a randomized controlled trial comparing 3 single-dose antibiotic regimens with loperamide. Clin Infect Dis. 2017; 65:2008–2017.
Article70. DuPont HL, Jiang ZD, Ericsson CD, Adachi JA, Mathewson JJ, DuPont MW, Palazzini E, Riopel LM, Ashley D, Martinez-Sandoval F. Rifaximin versus ciprofloxacin for the treatment of traveler's diarrhea: a randomized, double-blind clinical trial. Clin Infect Dis. 2001; 33:1807–1815.
Article71. Ochoa TJ, Chen J, Walker CM, Gonzales E, Cleary TG. Rifaximin does not induce toxin production or phage-mediated lysis of shiga toxin-producing Escherichia coli . Antimicrob Agents Chemother. 2007; 51:2837–2841.
Article72. Ohara T, Kojio S, Taneike I, Nakagawa S, Gondaira F, Tamura Y, Gejyo F, Zhang HM, Yamamoto T. Effects of azithromycin on shiga toxin production by Escherichia coli and subsequent host inflammatory response. Antimicrob Agents Chemother. 2002; 46:3478–3483.
Article73. Zhang X, McDaniel AD, Wolf LE, Keusch GT, Waldor MK, Acheson DW. Quinolone antibiotics induce Shiga toxin-encoding bacteriophages, toxin production, and death in mice. J Infect Dis. 2000; 181:664–670.
Article74. Safdar N, Said A, Gangnon RE, Maki DG. Risk of hemolytic uremic syndrome after antibiotic treatment of Escherichia coli O157:H7 enteritis: a meta-analysis. JAMA. 2002; 288:996–1001.
Article75. Freedman SB, Xie J, Neufeld MS, Hamilton WL, Hartling L, Tarr PI. Alberta Provincial Pediatric Enteric Infection Team (APPETITE). Nettel-Aguirre A, Chuck A, Lee B, Johnson D, Currie G, Talbot J, Jiang J, Dickinson J, Kellner J, MacDonald J, Svenson L, Chui L, Louie M, Lavoie M, Eltorki M, Vanderkooi O, Tellier R, Ali S, Drews S, Graham T, Pang XL. Shiga toxin-producing Escherichia coli infection, antibiotics, and risk of developing hemolytic uremic syndrome: A meta-analysis. Clin Infect Dis. 2016; 62:1251–1258.
Article76. Bennish ML, Salam MA, Khan WA, Khan AM. Treatment of shigellosis: III. Comparison of one- or two-dose ciprofloxacin with standard 5-day therapy. A randomized, blinded trial. Ann Intern Med. 1992; 117:727–734.
Article77. Ternhag A, Asikainen T, Giesecke J, Ekdahl K. A meta-analysis on the effects of antibiotic treatment on duration of symptoms caused by infection with Campylobacter species. Clin Infect Dis. 2007; 44:696–700.
Article78. Kuschner RA, Trofa AF, Thomas RJ, Hoge CW, Pitarangsi C, Amato S, Olafson RP, Echeverria P, Sadoff JC, Taylor DN. Use of azithromycin for the treatment of Campylobacter enteritis in travelers to Thailand, an area where ciprofloxacin resistance is prevalent. Clin Infect Dis. 1995; 21:536–541.
Article79. Nelson JD, Kusmiesz H, Jackson LH, Woodman E. Treatment of Salmonella gastroenteritis with ampicillin, amoxicillin, or placebo. Pediatrics. 1980; 65:1125–1130.
Article80. Onwuezobe IA, Oshun PO, Odigwe CC. Antimicrobials for treating symptomatic non-typhoidal Salmonella infection. Cochrane Database Syst Rev. 2012; 11:CD001167.81. Oh JY, Yu HS, Kim SK, Seol SY, Cho DT, Lee JC. Changes in patterns of antimicrobial susceptibility and integron carriage among Shigella sonnei isolates from southwestern Korea during epidemic periods. J Clin Microbiol. 2003; 41:421–423.
Article82. Spruill WJ, Wade WE. Diarrhea, constipation, and irritable bowel syndrome. 7th ed. New York: McGraw Hill Medical;2007. p. 617–623.83. DuPont HL, Sullivan P, Pickering LK, Haynes G, Ackerman PB. Symptomatic treatment of diarrhea with bismuth subsalicylate among students attending a Mexican university. Gastroenterology. 1977; 73:715–718.
Article84. DuPont HL. Bismuth subsalicylate in the treatment and prevention of diarrheal disease. Drug Intell Clin Pharm. 1987; 21:687–693.
Article85. Primi MP, Bueno L, Baumer P, Berard H, Lecomte JM. Racecadotril demonstrates intestinal antisecretory activity in vivo. Aliment Pharmacol Ther. 1999; 13:Suppl 6. 3–7.
Article86. Salazar-Lindo E, Santisteban-Ponce J, Chea-Woo E, Gutierrez M. Racecadotril in the treatment of acute watery diarrhea in children. N Engl J Med. 2000; 343:463–467.
Article87. Wang HH, Shieh MJ, Liao KF. A blind, randomized comparison of racecadotril and loperamide for stopping acute diarrhea in adults. World J Gastroenterol. 2005; 11:1540–1543.
Article88. Schiller LR, Santa Ana CA, Morawski SG, Fordtran JS. Mechanism of the antidiarrheal effect of loperamide. Gastroenterology. 1984; 86:1475–1480.
Article89. Stoll R, Ruppin H, Domschke W. Calmodulin-mediated effects of loperamide on chloride transport by brush border membrane vesicles from human ileum. Gastroenterology. 1988; 95:69–76.
Article90. Li ST, Grossman DC, Cummings P. Loperamide therapy for acute diarrhea in children: systematic review and meta-analysis. PLoS Med. 2007; 4:e98.
Article91. Riddle MS, Arnold S, Tribble DR. Effect of adjunctive loperamide in combination with antibiotics on treatment outcomes in traveler's diarrhea: a systematic review and meta-analysis. Clin Infect Dis. 2008; 47:1007–1014.
Article92. Johnson PC, Ericsson CD, DuPont HL, Morgan DR, Bitsura JA, Wood LV. Comparison of loperamide with bismuth subsalicylate for the treatment of acute travelers' diarrhea. JAMA. 1986; 255:757–760.
Article93. DuPont HL, Hornick RB. Adverse effect of lomotil therapy in shigellosis. JAMA. 1973; 226:1525–1528.
Article94. Bos J, Smithee L, McClane B, Distefano RF, Uzal F, Songer JG, Mallonee S, Crutcher JM. Fatal necrotizing colitis following a foodborne outbreak of enterotoxigenic Clostridium perfringens type A infection. Clin Infect Dis. 2005; 40:e78–e83.95. Koo HL, Koo DC, Musher DM, DuPont HL. Antimotility agents for the treatment of Clostridium difficile diarrhea and colitis. Clin Infect Dis. 2009; 48:598–605.
Article96. DuPont HL, Ericsson CD, DuPont MW, Cruz Luna A, Mathewson JJ. A randomized, open-label comparison of nonprescription loperamide and attapulgite in the symptomatic treatment of acute diarrhea. Am J Med. 1990; 88:20S–3S.
Article97. Portnoy BL, DuPont HL, Pruitt D, Abdo JA, Rodriguez JT. Antidiarrheal agents in the treatment of acute diarrhea in children. JAMA. 1976; 236:844–846.
Article98. Dinleyici EC. PROBAGE Study Group. Vandenplas Y. Lactobacillus reuteri DSM 17938 effectively reduces the duration of acute diarrhoea in hospitalised children. Acta Paediatr. 2014; 103:e300–5.99. Freedman SB, Ali S, Oleszczuk M, Gouin S, Hartling L. Treatment of acute gastroenteritis in children: an overview of systematic reviews of interventions commonly used in developed countries. Evid Based Child Health. 2013; 8:1123–1137.
Article100. Allen SJ, Martinez EG, Gregorio GV, Dans LF. Probiotics for treating acute infectious diarrhoea. Cochrane Database Syst Rev. 2010; CD003048.
Article101. Shane AL, Cabana MD, Vidry S, Merenstein D, Hummelen R, Ellis CL, Heimbach JT, Hempel S, Lynch SV, Sanders ME, Tancredi DJ. Guide to designing, conducting, publishing and communicating results of clinical studies involving probiotic applications in human participants. Gut Microbes. 2010; 1:243–253.
Article102. Buydens P, Debeuckelaere S. Efficacy of SF 68 in the treatment of acute diarrhea. A placebo-controlled trial. Scand J Gastroenterol. 1996; 31:887–891.
Article103. Wunderlich PF, Braun L, Fumagalli I, D'Apuzzo V, Heim F, Karly M, Lodi R, Politta G, Vonbank F, Zeltner L. Double-blind report on the efficacy of lactic acid-producing Enterococcus SF68 in the prevention of antibiotic-associated diarrhoea and in the treatment of acute diarrhoea. J Int Med Res. 1989; 17:333–338.
Article104. Mitra AK, Rabbani GH. A double-blind, controlled trial of bioflorin (Streptococcus faecium SF68) in adults with acute diarrhea due to Vibrio cholerae and enterotoxigenic Escherichia coli. Gastroenterology. 1990; 99:1149–1152.
Article105. Kochan P, Chmielarczyk A, Szymaniak L, Brykczynski M, Galant K, Zych A, Pakosz K, Giedrys-Kalemba S, Lenouvel E, Heczko PB. Lactobacillus rhamnosus administration causes sepsis in a cardiosurgical patient--is the time right to revise probiotic safety guidelines? Clin Microbiol Infect. 2011; 17:1589–1592.
Article106. Rijkers GT, Bengmark S, Enck P, Haller D, Herz U, Kalliomaki M, Kudo S, Lenoir-Wijnkoop I, Mercenier A, Myllyluoma E, Rabot S, Rafter J, Szajewska H, Watzl B, Wells J, Wolvers D, Antoine JM. Guidance for substantiating the evidence for beneficial effects of probiotics: current status and recommendations for future research. J Nutr. 2010; 140:671S–676S.
Article107. Ouwehand AC. A review of dose-responses of probiotics in human studies. Benef Microbes. 2017; 8:143–151.
Article108. Chapman CM, Gibson GR, Rowland I. Health benefits of probiotics: are mixtures more effective than single strains? Eur J Nutr. 2011; 50:1–17.
Article109. McFarland LV. Meta-analysis of probiotics for the prevention of traveler's diarrhea. Travel Med Infect Dis. 2007; 5:97–105.
Article110. Sazawal S, Hiremath G, Dhingra U, Malik P, Deb S, Black RE. Efficacy of probiotics in prevention of acute diarrhoea: a meta-analysis of masked, randomised, placebo-controlled trials. Lancet Infect Dis. 2006; 6:374–382.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Vibrio fluvialis Gastroenteritis
- The Retrospective Study on Antibiotics Treatment in Acute Gastroenteritis
- Antigen Distributions of Rotavirus and Adenovirus Detected by Enzyme Immuno Assay (EIA) from Acute Gastroenteritis Patients in Seoul
- New Viruses causing Gastroenteritis
- Causes of acute gastroenteritis in Korean children between 2004 and 2019