Yonsei Med J.
2019 Jul;60(7):626-632. 10.3349/ymj.2019.60.7.626.
Comparison of Apixaban and Low Molecular Weight Heparin in Preventing Deep Venous Thrombosis after Total Knee Arthroplasty in Older Adults
- Affiliations
-
- 1Department of Orthopedics, Jinling Hospital, Nanjing Clinical School of the Second Military Medical University, Nanjing, Jiangsu, China. guoting439h@163.com, zhaojianning578h@163.com
- KMID: 2450402
- DOI: http://doi.org/10.3349/ymj.2019.60.7.626
Abstract
- PURPOSE
To compare the effect of apixaban and low molecular weight heparin (LMWH) in the prevention and treatment of deep venous thrombosis (DVT) after total knee arthroplasty in older adult patients.
MATERIALS AND METHODS
A total of 220 patients (average age of 67.8±6.4 years) undergoing total knee arthroplasty were randomly selected as research subjects and were divided into apixaban and LMWH groups (110 in each group).
RESULTS
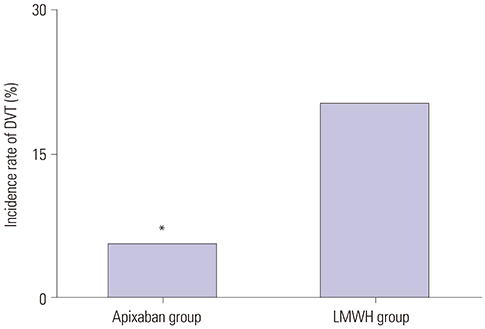
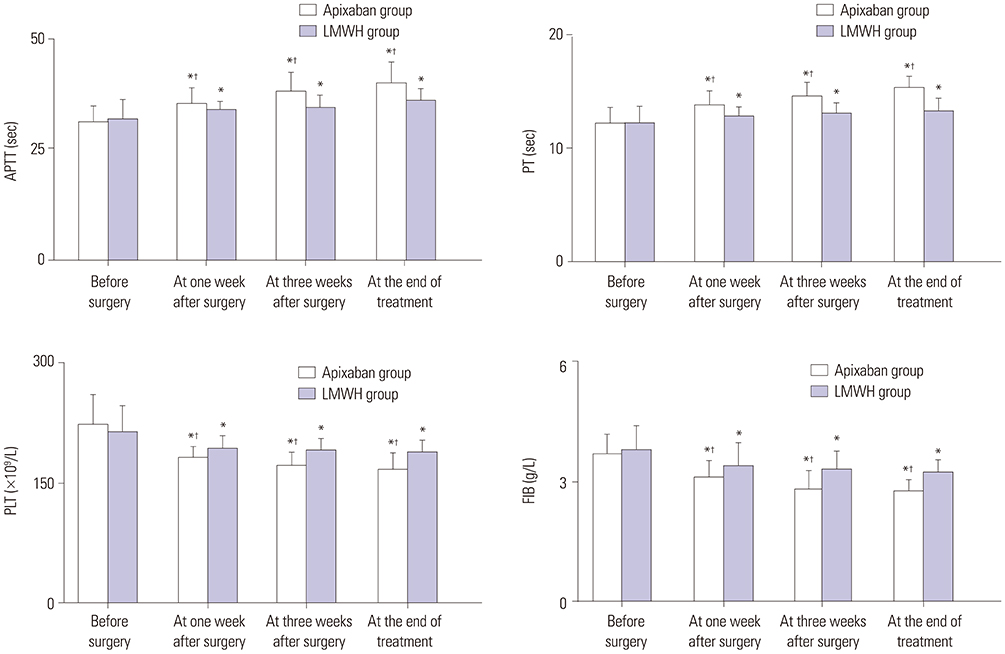
The incidence of DVT was lower in the apixaban group than in the LMWH group (5.5% vs. 20.0%, p=0.001). Activated partial thromboplastin times (35.2±3.6 sec vs. 33.7±2.2 sec, p=0.010; 37.8±4.6 sec vs. 34.1±3.2 sec, p<0.001; 39.6±5.1 sec vs. 35.7±3.0 sec, p=0.032) and prothrombin times (14.0±1.0 sec vs. 12.8±0.9 sec, p<0.001; 14.5±1.2 sec vs. 13.0±1.1 sec, p<0.001; 15.3±1.4 sec vs. 13.2±1.3 sec, p=0.009) in the apixaban group at 1 week after surgery, 3 weeks after surgery, and the end of treatment were higher than those in the LMWH group. Platelet and fibrinogen levels in the apixaban group were lower than those of the LMWH group. Also, capillary plasma viscosity and erythrocyte aggregation in the apixaban group at 1 week after surgery, 3 weeks after surgery, and the end of treatment were lower than those in the LMWH group.
CONCLUSION
Apixaban, which elicits fewer adverse reactions and is safer than LMWH, exhibited better effects in the prevention and treatment of DVT after total knee arthroplasty in older adults.
MeSH Terms
Figure
Reference
-
1. Bonutti PM, Sodhi N, Patel YH, Sultan AA, Khlopas A, Chughtai M, et al. Novel venous thromboembolic disease (VTED) prophylaxis for total knee arthroplasty-aspirin and fish oil. Ann Transl Med. 2017; 5:Suppl 3. S30.
Article2. Zhou LY, Gu W, Liu Y, Ma ZL. Effects of inhalation anesthesia vs. total intravenous anesthesia (TIVA) vs. spinal-epidural anesthesia on deep vein thrombosis after total knee arthroplasty. Med Sci Monit. 2018; 24:67–75.
Article3. Falck-Ytter Y, Francis CW, Johanson NA, Curley C, Dahl OE, Schulman S, et al. Prevention of VTE in orthopedic surgery patients. Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141:2 Suppl. e278S–e325S.4. Wakabayashi H, Hasegawa M, Niimi R, Yamaguchi T, Naito Y, Sudo A. The risk factor of preoperative deep vein thrombosis in patients undergoing total knee arthroplasty. J Orthop Sci. 2017; 22:698–702.
Article5. Zou Y, Tian S, Wang Y, Sun K. Administering aspirin, rivaroxaban and low-molecular-weight heparin to prevent deep venous thrombosis after total knee arthroplasty. Blood Coagul Fibrinolysis. 2014; 25:660–664.
Article6. Warwick D, Friedman RJ, Agnelli G, Gil-Garay E, Johnson K, FitzGerald G, et al. Insufficient duration of venous thromboembolism prophylaxis after total hip or knee replacement when compared with the time course of thromboembolic events: findings from the Global Orthopaedic Registry. J Bone Joint Surg Br. 2007; 89:799–807.7. Beyer-Westendorf J, Lützner J, Donath L, Tittl L, Knoth H, Radke OC, et al. Efficacy and safety of thromboprophylaxis with low-molecular-weight heparin or rivaroxaban in hip and knee replacement surgery: findings from the ORTHO-TEP registry. Thromb Haemost. 2013; 109:154–163.
Article8. Aryal MR, Pandit A, Ghimire S, Pathak R, Karmacharya P, Poudel DR, et al. Thromboprophylaxis with apixaban and the risk of pulmonary embolism in patients undergoing knee replacement surgery. J Community Hosp Intern Med Perspect. 2015; 5:27889.
Article9. King DA, Pow RE, Dickison DM, Vale PR. Apixaban versus enoxaparin in the prevention of venous thromboembolism following total knee arthroplasty: a single-centre, single-surgeon, retrospective analysis. Intern Med J. 2016; 46:1030–1037.
Article10. Lassen MR, Raskob GE, Gallus A, Pineo G, Chen D, Portman RJ. Apixaban or enoxaparin for thromboprophylaxis after knee replacement. N Engl J Med. 2009; 361:594–604.
Article11. Cafri G, Paxton EW, Chen Y, Cheetham CT, Gould MK, Sluggett J, et al. Comparative effectiveness and safety of drug prophylaxis for prevention of venous thromboembolism after total knee arthroplasty. J Arthroplasty. 2017; 32:3524–3528.
Article12. Bala A, Huddleston JI 3rd, Goodman SB, Maloney WJ, Amanatullah DF. Venous thromboembolism prophylaxis after TKA: aspirin, warfarin, enoxaparin, or factor Xa inhibitors? Clin Orthop Relat Res. 2017; 475:2205–2213.
Article13. Kang J, Jiang X, Wu B. Analysis of risk factors for lower-limb deep venous thrombosis in old patients after knee arthroplasty. Chin Med J (Engl). 2015; 128:1358–1362.
Article14. Kuperman EF, Schweizer M, Joy P, Gu X, Fang MM. The effects of advanced age on primary total knee arthroplasty: a meta-analysis and systematic review. BMC Geriatr. 2016; 16:41.
Article15. Pierce TP, Elmallah RK, Jauregui JJ, Cherian JJ, Mont MA. What's new in venous thromboembolic prophylaxis following total knee and total hip arthroplasty? An update. Surg Technol Int. 2015; 26:234–237.16. Lieberman JR, Hsu WK. Prevention of venous thromboembolic disease after total hip and knee arthroplasty. J Bone Joint Surg Am. 2005; 87:2097–2112.
Article17. Lazo-Langner A, Fleet JL, McArthur E, Garg AX. Rivaroxaban vs. low molecular weight heparin for the prevention of venous thromboembolism after hip or knee arthroplasty: a cohort study. J Thromb Haemost. 2014; 12:1626–1635.
Article18. O'Donnell M, Linkins LA, Kearon C, Julian J, Hirsh J. Reduction of out-of-hospital symptomatic venous thromboembolism by extended thromboprophylaxis with low-molecular-weight heparin following elective hip arthroplasty: a systematic review. Arch Intern Med. 2003; 163:1362–1366.19. Li X, Keshishian A, Hamilton M, Horblyuk R, Gupta K, Luo X, et al. Apixaban 5 and 2.5 mg twice-daily versus warfarin for stroke prevention in nonvalvular atrial fibrillation patients: comparative effectiveness and safety evaluated using a propensity-scorematched approach. PLoS One. 2018; 13:e0191722.
Article20. Venker BT, Ganti BR, Lin H, Lee ED, Nunley RM, Gage BF. Safety and efficacy of new anticoagulants for the prevention of venous thromboembolism after hip and knee arthroplasty: a meta-analysis. J Arthroplasty. 2017; 32:645–652.
Article21. Lanitis T, Leipold R, Hamilton M, Rublee D, Quon P, Browne C, et al. Cost-effectiveness of apixaban versus low molecular weight heparin/vitamin k antagonist for the treatment of venous thromboembolism and the prevention of recurrences. BMC Health Serv Res. 2017; 17:74.
Article22. Lassen MR, Davidson BL, Gallus A, Pineo G, Ansell J, Deitchman D. The efficacy and safety of apixaban, an oral, direct factor Xa inhibitor, as thromboprophylaxis in patients following total knee replacement. J Thromb Haemost. 2007; 5:2368–2375.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spinal epidural hematoma after epidural anesthesia in a patient receiving enoxaparin: A case report
- Incidences of Deep Vein Thrombosis and Pulmonary Embolism after Total Knee Arthroplasty Using a Mechanical Compression Device with and without Low-Molecular-Weight Heparin
- Successful Treatment of Aortic Thrombosis after Umbilical Catheterization with Low-Molecular-Weight Heparin
- Deep Vein Thrombosis and Neurovascular Injury after Total Hip Arthroplasty
- A Case with Upper Extremity Deep Vein Thrombosis after in vitro Fertilization