Korean Circ J.
2019 Jul;49(7):602-611. 10.4070/kcj.2018.0290.
Prognostic Implication of Ventricular Conduction Disturbance Pattern in Hospitalized Patients with Acute Heart Failure Syndrome
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 2Department of Cardiology, Cardiovascular Center, Seoul National University Bundang Hospital, Seongnam, Korea. djchoi@snubh.org
- 3Division of Cardiology, Heart Institute, Asan Medical Center, University of Ulsan, Seoul, Korea.
- 4Department of Internal Medicine, Heart Research Center of Chonnam National University, Gwangju, Korea.
- 5Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 6Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 7Department of Internal Medicine, Sungkyunkwan University College of Medicine, Seoul, Korea.
- 8Department of Internal Medicine, Chungbuk National University College of Medicine, Cheongju, Korea.
- 9Department of Internal Medicine, Kyungpook National University College of Medicine, Daegu, Korea.
- 10Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea.
- KMID: 2450391
- DOI: http://doi.org/10.4070/kcj.2018.0290
Abstract
- BACKGROUND AND OBJECTIVES
Conflicting data exist regarding the prognostic implication of ventricular conduction disturbance pattern in patients with heart failure (HF). This study investigated the prognostic impact of ventricular conduction pattern in hospitalized patients with acute HF.
METHODS
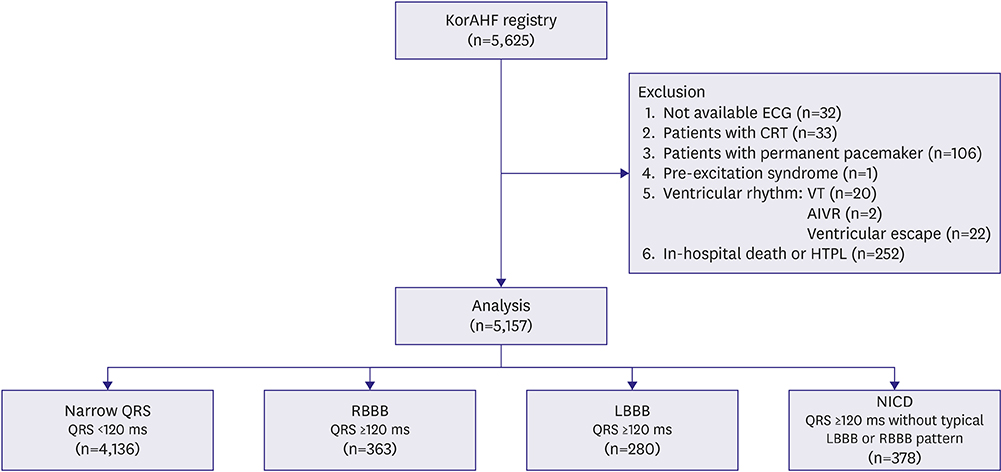
Data from the Korean Acute Heart Failure registry were used. Patients were categorized into four groups: narrow QRS (<120 ms), right bundle branch block (RBBB), left bundle branch block (LBBB), and nonspecific intraventricular conduction delay (NICD). The NICD was defined as prolonged QRS (≥120 ms) without typical features of LBBB or RBBB. The primary endpoint was the composite of all-cause mortality or rehospitalization for HF aggravation within 1 year after discharge.
RESULTS
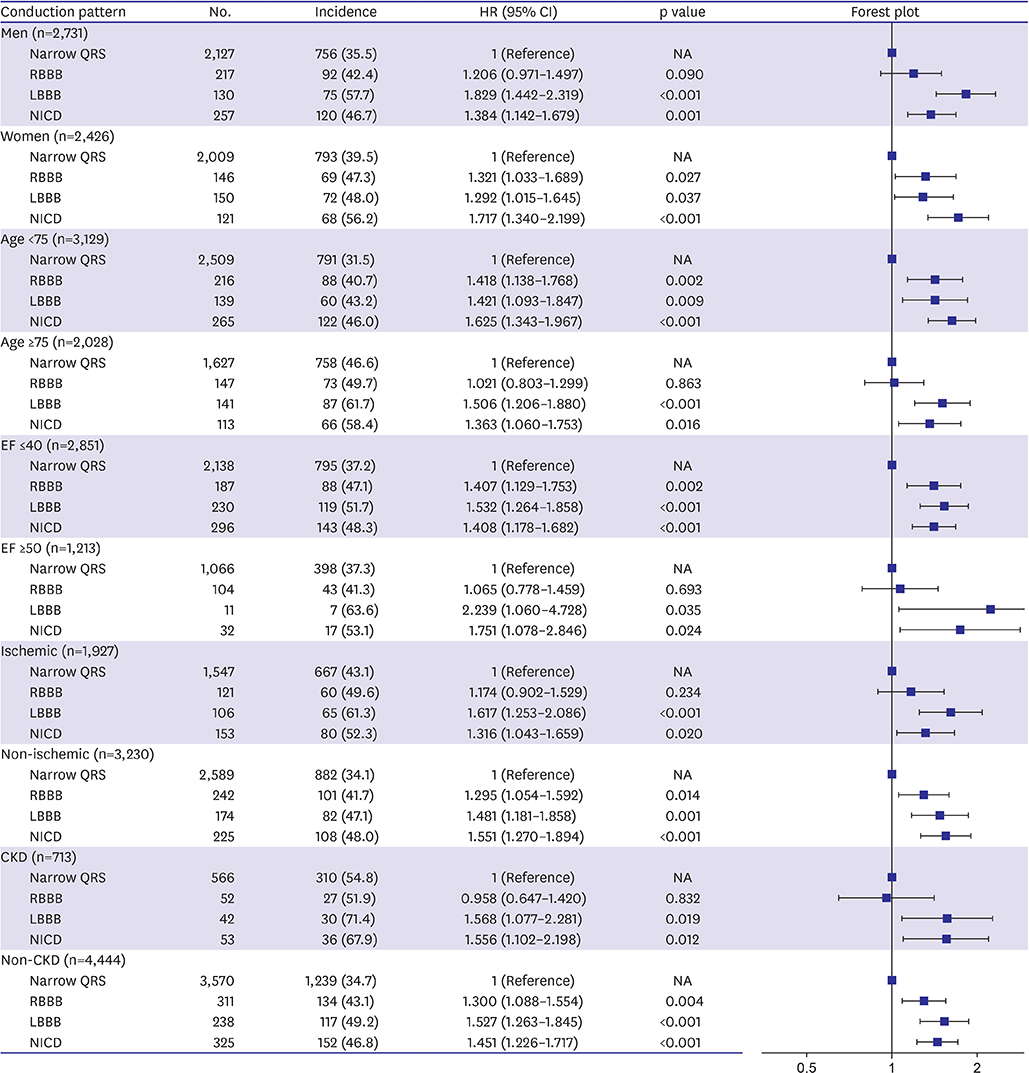
This study included 5,157 patients. The primary endpoint occurred in 39.7% of study population. The LBBB group showed the highest incidence of primary endpoint followed by NICD, RBBB, and narrow QRS groups (52.5% vs. 49.7% vs. 44.4% vs. 37.5%, p<0.001). In a multivariable Cox-proportional hazards regression analysis, LBBB and NICD were associated with 39% and 28% increased risk for primary endpoint (LBBB hazard ratio [HR], 1.392; 95% confidence interval [CI], 1.152-1.681; NICD HR, 1.278; 95% CI, 1.074-1.520) compared with narrow QRS group. The HR of RBBB for the primary endpoint was 1.103 (95% CI, 0.915-1.329).
CONCLUSIONS
LBBB and NICD were independently associated with an increased risk of 1-year adverse event in hospitalized patients with HF, whereas the prognostic impacts of RBBB were limited. TRIAL REGISTRATION: ClinicalTrials.gov Identifier: NCT01389843
Figure
Reference
-
1. Wang NC, Maggioni AP, Konstam MA, et al. Clinical implications of QRS duration in patients hospitalized with worsening heart failure and reduced left ventricular ejection fraction. JAMA. 2008; 299:2656–2666.2. Mueller C, Laule-Kilian K, Klima T, et al. Right bundle branch block and long-term mortality in patients with acute congestive heart failure. J Intern Med. 2006; 260:421–428.3. Hong SJ, Oh J, Kang SM, et al. Clinical implication of right bundle branch block in hospitalized patients with acute heart failure: data from the Korean Heart Failure (KorHF) Registry. Int J Cardiol. 2012; 157:416–418.4. Abdel-Qadir HM, Tu JV, Austin PC, Wang JT, Lee DS. Bundle branch block patterns and long-term outcomes in heart failure. Int J Cardiol. 2011; 146:213–218.5. Tolppanen H, Siirila-Waris K, Harjola VP, et al. Ventricular conduction abnormalities as predictors of long-term survival in acute de novo and decompensated chronic heart failure. ESC Heart Fail. 2016; 3:35–43.6. Eschalier R, Ploux S, Ritter P, Haïssaguerre M, Ellenbogen KA, Bordachar P. Nonspecific intraventricular conduction delay: definitions, prognosis, and implications for cardiac resynchronization therapy. Heart Rhythm. 2015; 12:1071–1079.7. Lee SE, Cho HJ, Lee HY, et al. A multicentre cohort study of acute heart failure syndromes in Korea: rationale, design, and interim observations of the Korean Acute Heart Failure (KorAHF) registry. Eur J Heart Fail. 2014; 16:700–708.8. Lee SE, Lee HY, Cho HJ, et al. Clinical characteristics and outcome of acute heart failure in Korea: results from the Korean Acute Heart Failure Registry (KorAHF). Korean Circ J. 2017; 47:341–353.9. Willems JL, Robles de Medina EO, Bernard R, et al. Criteria for intraventricular conduction disturbances and pre-excitation. J Am Coll Cardiol. 1985; 5:1261–1275.10. Derval N, Duchateau J, Mahida S, et al. Distinctive left ventricular activations associated with ECG pattern in heart failure patients. Circ Arrhythm Electrophysiol. 2017; 10:e005073.11. Aro AL, Anttonen O, Tikkanen JT, et al. Intraventricular conduction delay in a standard 12-lead electrocardiogram as a predictor of mortality in the general population. Circ Arrhythm Electrophysiol. 2011; 4:704–710.12. Zimetbaum PJ, Buxton AE, Batsford W, et al. Electrocardiographic predictors of arrhythmic death and total mortality in the multicenter unsustained tachycardia trial. Circulation. 2004; 110:766–769.13. Barsheshet A, Goldenberg I, Garty M, et al. Relation of bundle branch block to long-term (four-year) mortality in hospitalized patients with systolic heart failure. Am J Cardiol. 2011; 107:540–544.14. McCullough PA, Hassan SA, Pallekonda V, et al. Bundle branch block patterns, age, renal dysfunction, and heart failure mortality. Int J Cardiol. 2005; 102:303–308.15. Farwell D, Patel NR, Hall A, Ralph S, Sulke AN. How many people with heart failure are appropriate for biventricular resynchronization? Eur Heart J. 2000; 21:1246–1250.16. Tabrizi F, Englund A, Rosenqvist M, Wallentin L, Stenestrand U. Influence of left bundle branch block on long-term mortality in a population with heart failure. Eur Heart J. 2007; 28:2449–2455.17. Cinca J, Mendez A, Puig T, et al. Differential clinical characteristics and prognosis of intraventricular conduction defects in patients with chronic heart failure. Eur J Heart Fail. 2013; 15:877–884.18. Gijsberts CM, Benson L, Dahlström U, et al. Ethnic differences in the association of QRS duration with ejection fraction and outcome in heart failure. Heart. 2016; 102:1464–1471.19. Park HS, Kim H, Park JH, et al. QRS prolongation in the prediction of clinical cardiac events in patients with acute heart failure: analysis of data from the Korean Acute Heart Failure Registry. Cardiology. 2013; 125:96–103.20. Park SJ, On YK, Byeon K, et al. Short- and long-term outcomes depending on electrical dyssynchrony markers in patients presenting with acute heart failure: clinical implication of the first-degree atrioventricular block and QRS prolongation from the Korean Heart Failure registry. Am Heart J. 2013; 165:57–64.e2.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ventricular Conduction Disturbance in Acute Heart Failure Syndrome: Does It Matter for Prognosis?
- Elevating Right Ventricular Assessment: The Transformative Prognostic Power of RVGLS/PASP Ratio in Acute Heart Failure
- Clinical Implication of Mechanical Dyssynchrony in Heart Failure
- The Pathophysiology and Diagnostic Approaches for Diastolic Left Ventricular Dysfunction: A Clinical Perspective
- A Case of Pacemaker Syndrome