Korean Circ J.
2019 Jul;49(7):586-599. 10.4070/kcj.2018.0415.
Rationale and Design of the High Platelet Inhibition with Ticagrelor to Improve Left Ventricular Remodeling in Patients with ST-Segment Elevation Myocardial Infarction (HEALING-AMI) Trial
- Affiliations
-
- 1Department of Internal Medicine, Gyeongsang National University Changwon Hospital, Changwon, Korea. goodoctor@naver.com
- 2Division of Cardiology, Department of Internal Medicine, Chungnam National University Hospital, Daejeon, Korea.
- 3Department of Internal Medicine, Changwon Samsung Medical Center, Changwon, Korea.
- 4Division of Cardiology, Department of Internal Medicine, Ulsan University Hospital, Ulsan, Korea.
- 5Division of Cardiology, Department of Internal Medicine, Chungbuk National University Hospital, Cheongju, Korea.
- 6Division of Cardiology, Department of Internal Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea.
- 7Division of Cardiology, Department of Internal Medicine, Kyung Hee University Hospital, Seoul, Korea.
- 8Division of Cardiology, Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- 9Division of Cardiology, Department of Internal Medicine, Kyungpook National University Hospital, Daegu, Korea.
- 10Division of Cardiology, Department of Internal Medicine, Chonnam National University Hospital, Gwangju, Korea.
- 11Department of Cardiology, Singapore National University Heart Centre, Singapore.
- 12Department of Internal Medicine, Gyeongsang National University Hospital, Jinju, Korea.
- KMID: 2450389
- DOI: http://doi.org/10.4070/kcj.2018.0415
Abstract
- BACKGROUND AND OBJECTIVES
Impaired recovery from left ventricular (LV) dysfunction is a major prognostic factor after myocardial infarction (MI). Because P2Y12 receptor blockade inhibits myocardial injury, ticagrelor with off-target properties may have myocardial protection over clopidogrel. In animal models, ticagrelor vs. clopidogrel protects myocardium against reperfusion injury and improves remodeling after MI. We aimed to investigate the effect of ticagrelor on sequential myocardial remodeling process after MI.
METHODS
High platelet inhibition with ticagrelor to improve LV remodeling in patients with ST-segment elevation MI (HEALING-AMI) is an investigator-initiated, randomized, open-label, assessor-blinded, multi-center trial done at 10 sites in Korea. Patients will be enrolled if they have ST-segment elevation MI (STEMI) treated with primary percutaneous coronary intervention and a planned duration of dual antiplatelet treatment of at least 6 months. Screened patients will be randomly assigned (1:1) using an internet-based randomization with a computer-generated blocking with stratification across study sites to either ticagrelor or clopidogrel treatment. The co-primary primary endpoints are LV remodeling index with three-dimensional echocardiography and the level of N-terminal prohormone B-type natriuretic peptide (NT-proBNP) at 6 months representing post-MI remodeling processes. Changes of LV end-systolic/diastolic volume indices and LV ejection fraction between baseline and 6-month follow-up will be also evaluated. Analysis is per protocol.
CONCLUSIONS
HEALING-AMI is testing the effect of ticagrelor in reducing adverse LV remodeling following STEMI. Our trial would show the benefit of ticagrelor vs. clopidogrel related to the recovery of post-MI LV dysfunction beyond potent platelet inhibition. TRIAL REGISTRATION: ClinicalTrials.gov Identifier: NCT02224534
MeSH Terms
Figure
Reference
-
1. Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation. 2018; 137:e67–492.
Article2. Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018; 39:119–177.3. Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines and the Heart Failure Society of America. Circulation. 2017; 136:e137–61.
Article4. Burchfield JS, Xie M, Hill JA. Pathological ventricular remodeling: mechanisms: part 1 of 2. Circulation. 2013; 128:388–400.5. Liehn EA, Postea O, Curaj A, Marx N. Repair after myocardial infarction, between fantasy and reality: the role of chemokines. J Am Coll Cardiol. 2011; 58:2357–2362.6. Anzai T. Post-infarction inflammation and left ventricular remodeling: a double-edged sword. Circ J. 2013; 77:580–587.7. Ziegler-Heitbrock L. The CD14+ CD16+ blood monocytes: their role in infection and inflammation. J Leukoc Biol. 2007; 81:584–592.8. Tapp LD, Shantsila E, Wrigley BJ, Pamukcu B, Lip GY. The CD14++CD16+ monocyte subset and monocyte-platelet interactions in patients with ST-elevation myocardial infarction. J Thromb Haemost. 2012; 10:1231–1241.9. Nurden AT. Platelets, inflammation and tissue regeneration. Thromb Haemost. 2011; 105:Suppl 1. S13–S33.
Article10. Rondina MT, Weyrich AS, Zimmerman GA. Platelets as cellular effectors of inflammation in vascular diseases. Circ Res. 2013; 112:1506–1519.
Article11. Semple JW, Italiano JE Jr, Freedman J. Platelets and the immune continuum. Nat Rev Immunol. 2011; 11:264–274.
Article12. Opie LH, Commerford PJ, Gersh BJ, Pfeffer MA. Controversies in ventricular remodelling. Lancet. 2006; 367:356–367.
Article13. Italiano JE Jr, Richardson JL, Patel-Hett S, et al. Angiogenesis is regulated by a novel mechanism: pro- and antiangiogenic proteins are organized into separate platelet α granules and differentially released. Blood. 2008; 111:1227–1233.
Article14. Swiatkiewicz I, Kozinski M, Magielski P, et al. Value of C-reactive protein in predicting left ventricular remodelling in patients with a first ST-segment elevation myocardial infarction. Mediators Inflamm. 2012; 2012:250867.
Article15. Liu Y, Gao XM, Fang L, et al. Novel role of platelets in mediating inflammatory responses and ventricular rupture or remodeling following myocardial infarction. Arterioscler Thromb Vasc Biol. 2011; 31:834–841.
Article16. Du XJ, Shan L, Gao XM, et al. Role of intramural platelet thrombus in the pathogenesis of wall rupture and intra-ventricular thrombosis following acute myocardial infarction. Thromb Haemost. 2011; 105:356–364.
Article17. Ye Y, Birnbaum GD, Perez-Polo JR, Nanhwan MK, Nylander S, Birnbaum Y. Ticagrelor protects the heart against reperfusion injury and improves remodeling after myocardial infarction. Arterioscler Thromb Vasc Biol. 2015; 35:1805–1814.
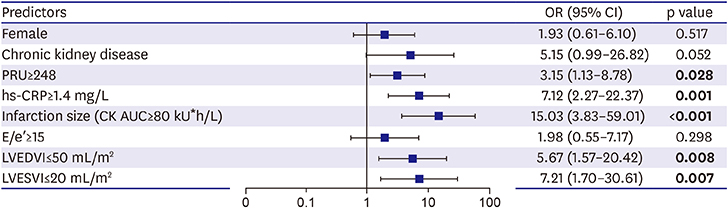
Article18. Park Y, Tantry US, Koh JS, et al. Novel role of platelet reactivity in adverse left ventricular remodelling after ST-segment elevation myocardial infarction: the REMODELING trial. Thromb Haemost. 2017; 117:911–922.
Article19. Nanhwan MK, Ling S, Kodakandla M, Nylander S, Ye Y, Birnbaum Y. Chronic treatment with ticagrelor limits myocardial infarct size: an adenosine and cyclooxygenase-2-dependent effect. Arterioscler Thromb Vasc Biol. 2014; 34:2078–2085.20. Vilahur G, Gutiérrez M, Casani L, et al. Protective effects of ticagrelor on myocardial injury after infarction. Circulation. 2016; 134:1708–1719.
Article21. Kang MG, Ahn JH, Jang JY, et al. Ticagrelor versus clopidogrel is associated with better recovery of LV function after AMI. J Am Coll Cardiol. 2017; 69:125.22. Sjöblom J, Muhrbeck J, Witt N, Alam M, Frykman-Kull V. Evolution of left ventricular ejection fraction after acute myocardial infarction: implications for implantable cardioverter-defibrillator eligibility. Circulation. 2014; 130:743–748.23. Thygesen K, Mair J, Mueller C, et al. Recommendations for the use of natriuretic peptides in acute cardiac care: a position statement from the Study Group on Biomarkers in Cardiology of the ESC Working Group on Acute Cardiac Care. Eur Heart J. 2012; 33:2001–2006.
Article24. Storey RF, Angiolillo DJ, Patil SB, et al. Inhibitory effects of ticagrelor compared with clopidogrel on platelet function in patients with acute coronary syndromes: the PLATO (PLATelet inhibition and patient Outcomes) PLATELET substudy. J Am Coll Cardiol. 2010; 56:1456–1462.25. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016; 37:2129–2200.26. Jenkins C, Moir S, Chan J, Rakhit D, Haluska B, Marwick TH. Left ventricular volume measurement with echocardiography: a comparison of left ventricular opacification, three-dimensional echocardiography, or both with magnetic resonance imaging. Eur Heart J. 2009; 30:98–106.
Article27. Gerczuk PZ, Kloner RA. An update on cardioprotection: a review of the latest adjunctive therapies to limit myocardial infarction size in clinical trials. J Am Coll Cardiol. 2012; 59:969–978.28. Gerber Y, Weston SA, Redfield MM, et al. A contemporary appraisal of the heart failure epidemic in Olmsted County, Minnesota, 2000 to 2010. JAMA Intern Med. 2015; 175:996–1004.
Article29. Gerber Y, Weston SA, Enriquez-Sarano M, et al. Mortality associated with heart failure after myocardial infarction: a contemporary community perspective. Circ Heart Fail. 2016; 9:e002460.30. Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention, 2011 ACCF/AHA guideline for coronary artery bypass graft surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease, 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction, 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes, and 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery. Circulation. 2016; 134:e123–55.
Article31. Bae JS, Ahn JH, Tantry US, Gurbel PA, Jeong YH. Should antithrombotic treatment strategies in East Asians differ from Caucasians? Curr Vasc Pharmacol. 2018; 16:459–476.32. Kang J, Kim HS. The evolving concept of dual antiplatelet therapy after percutaneous coronary intervention: focus on unique feature of East Asian and “Asian paradox”. Korean Circ J. 2018; 48:537–551.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- ST segment
- Differences in Clinical Outcomes Between Patients With ST-Elevation Versus Non-ST-Elevation Acute Myocardial Infarction in Korea
- Correlations between Serum Inflammation Factors and Left Ventricular Remodeling in Acute ST Segment Elevation Myocardial Infarction
- Coronary Angiographic Features and Clinical Significance of Inferior ST segment Elevation during Acute Anterior Myocardial Infarction
- The Eletrocardiographic Analysis of Acute Myocardial Infarction and Non-infarction Syndrome In the Patients with ST Segment Elevation and Chest Pain