Yonsei Med J.
2015 May;56(3):838-844. 10.3349/ymj.2015.56.3.838.
Comparison of Ultrasound-Guided Axillary Brachial Plexus Block Techniques: Perineural Injection versus Single or Double Perivascular Infiltration
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, School of Medicine, Ewha Womans University, Seoul, Korea. ankyj@ewha.ac.kr
- KMID: 2450362
- DOI: http://doi.org/10.3349/ymj.2015.56.3.838
Abstract
- PURPOSE
We compared three methods of ultrasound-guided axillary brachial plexus block, which were single, and double perivascular (PV) infiltration techniques, and a perineural (PN) injection technique.
MATERIALS AND METHODS
78 patients of American Society of Anesthesiologists physical status I-II undergoing surgery of the forearm, wrist, or hand were randomly allocated to three groups. 2% lidocaine with epinephrine 5 microg/mL was used. The PN group (n=26) received injections at the median, ulnar, and radial nerve with 8 mL for each nerve. The PV1 group (n=26) received a single injection of 24 mL at 12-o'clock position of the axillary artery. The PV2 group (n=26) received two injections of 12 mL each at 12-o'clock and 6-o'clock position. For all groups, musculocutaneous nerve was blocked separately.
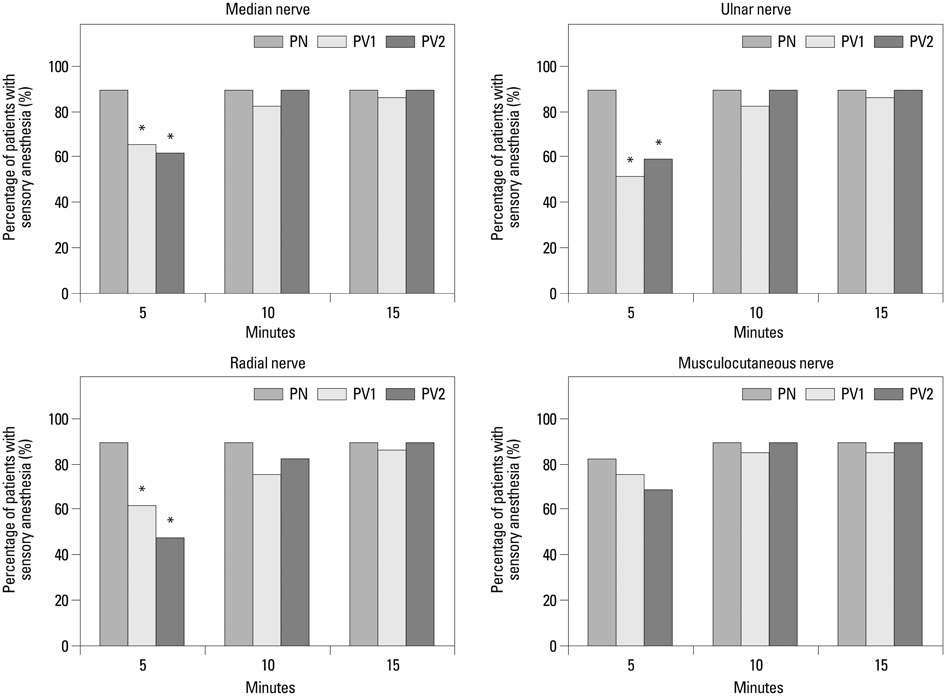
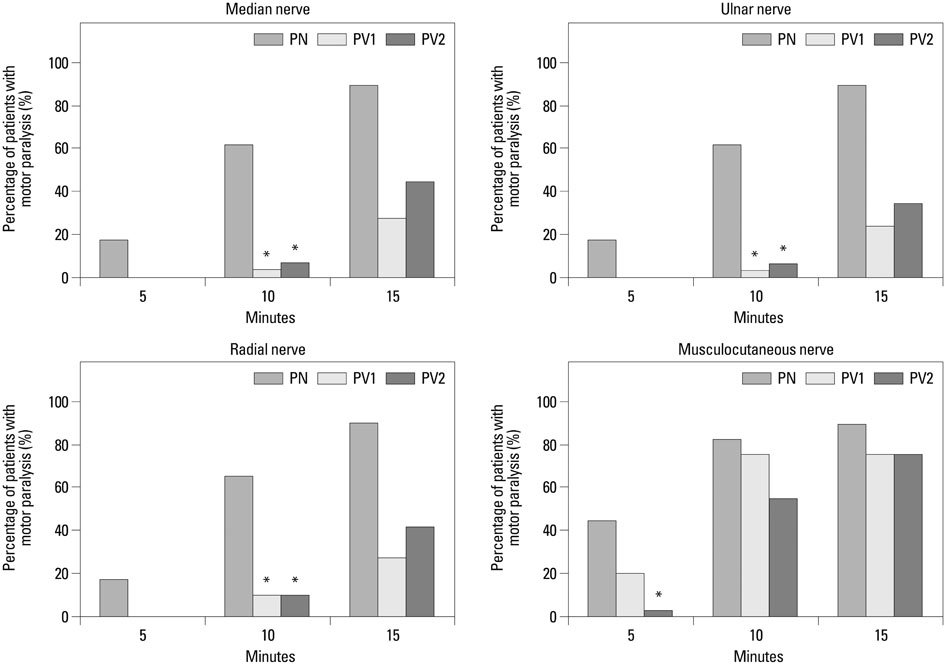
RESULTS
The PN group (391.2+/-171.6 sec) had the longest anesthetic procedure duration than PV1 (192.8+/-59.0 sec) and PV2 (211.4+/-58.6 sec). There were no differences in onset time. The average induction time was longer in PN group (673.4+/-149.6 sec) than PV1 (557.6+/-194.9 sec) and PV2 (561.5+/-129.8 sec). There were no differences in the success rate (89.7% vs. 86.2% vs. 89.7%).
CONCLUSION
The PV injection technique consisting of a single injection in 12-o'clock position above the axillary artery in addition to a musculocutaneous nerve block is equally effective and less time consuming than the PN technique. Therefore, the PV technique is an alternative method that may be used in busy clinics or for difficult cases.
Keyword
MeSH Terms
-
Adult
Anesthetics, Local/*administration & dosage/adverse effects
Brachial Plexus/*drug effects/*ultrasonography
Brachial Plexus Block/adverse effects/*methods
Female
Forearm/surgery
Hand/surgery
Humans
Injections
Male
Middle Aged
Peripheral Nerves/ultrasonography
Prospective Studies
Single-Blind Method
Treatment Outcome
*Ultrasonography, Interventional
Upper Extremity/innervation/*surgery
Vascular System Injuries/etiology
Wrist/surgery
Anesthetics, Local
Figure
Reference
-
1. Chan VW, Peng PW, Kaszas Z, Middleton WJ, Muni R, Anastakis DG, et al. A comparative study of general anesthesia, intravenous regional anesthesia, and axillary block for outpatient hand surgery: clinical outcome and cost analysis. Anesth Analg. 2001; 93:1181–1184.
Article2. Casati A, Danelli G, Baciarello M, Corradi M, Leone S, Di Cianni S, et al. A prospective, randomized comparison between ultrasound and nerve stimulation guidance for multiple injection axillary brachial plexus block. Anesthesiology. 2007; 106:992–996.
Article3. Chan VW, Perlas A, McCartney CJ, Brull R, Xu D, Abbas S. Ultrasound guidance improves success rate of axillary brachial plexus block. Can J Anaesth. 2007; 54:176–182.
Article4. Imasogie N, Ganapathy S, Singh S, Armstrong K, Armstrong P. A prospective, randomized, double-blind comparison of ultrasound-guided axillary brachial plexus blocks using 2 versus 4 injections. Anesth Analg. 2010; 110:1222–1226.
Article5. Bernucci F, Gonzalez AP, Finlayson RJ, Tran DQ. A prospective, randomized comparison between perivascular and perineural ultrasound-guided axillary brachial plexus block. Reg Anesth Pain Med. 2012; 37:473–477.
Article6. Tran DQ, Pham K, Dugani S, Finlayson RJ. A prospective, randomized comparison between double-, triple-, and quadruple-injection ultrasound-guided axillary brachial plexus block. Reg Anesth Pain Med. 2012; 37:248–253.
Article7. Edgcombe H, Hocking G. Sonographic identification of needle tip by specialists and novices: a blinded comparison of 5 regional block needles in fresh human cadavers. Reg Anesth Pain Med. 2010; 35:207–211.8. Hocking G, Mitchell CH. Optimizing the safety and practice of ultrasound-guided regional anesthesia: the role of echogenic technology. Curr Opin Anaesthesiol. 2012; 25:603–609.
Article9. Cho S, Kim YJ, Kim JH, Baik HJ. Double-injection perivascular ultrasound-guided axillary brachial plexus block according to needle positioning: 12 versus 6 o'clock position of the axillary artery. Korean J Anesthesiol. 2014; 66:112–119.
Article10. Porter JM, McCartney CJ, Chan VW. Needle placement and injection posterior to the axillary artery may predict successful infraclavicular brachial plexus block: a report of three cases. Can J Anaesth. 2005; 52:69–73.
Article11. Lévesque S, Dion N, Desgagné MC. Endpoint for successful, ultrasound-guided infraclavicular brachial plexus block. Can J Anaesth. 2008; 55:308.
Article12. Orebaugh SL, Williams BA. Brachial plexus anatomy: normal and variant. ScientificWorldJournal. 2009; 9:300–312.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Double-injection perivascular ultrasound-guided axillary brachial plexus block according to needle positioning: 12 versus 6 o'clock position of the axillary artery
- Comparison of Two Methods of Axillary Brachial Plexus Block
- Bilateral variant locations of the musculocutaneous nerve during ultrasound-guided bilateral axillary brachial plexus block: A case report
- Comparison of Axillary and Supraclavicular Approach in Ultrasound-Guided Brachial Plexus Block
- Axillary Block of Brachial Plexus : A Review of 808 Cases