J Korean Orthop Assoc.
2019 Jun;54(3):244-253. 10.4055/jkoa.2019.54.3.244.
Comparison of the Outcomes after Primary Total Hip Arthroplasty Using a Short Stem between the Modified Anterolateral Approach and Direct Anterior Approach with a Standard Operation Table
- Affiliations
-
- 1Department of Orthopedic Surgery, Hoseung Hospital, Jeonju, Korea.
- 2Department of Orthopaedic Surgery, Chonbuk National University Medical School, Jeonju, Korea.
- 3Department of Orthopedic Surgery, Gwangju Veterans Hospital, Gwangju, Korea. chm1228@hanmail.net
- 4Department of Orthopedic Surgery, St. Carollo Hospital, Suncheon, Korea.
- KMID: 2450144
- DOI: http://doi.org/10.4055/jkoa.2019.54.3.244
Abstract
- PURPOSE
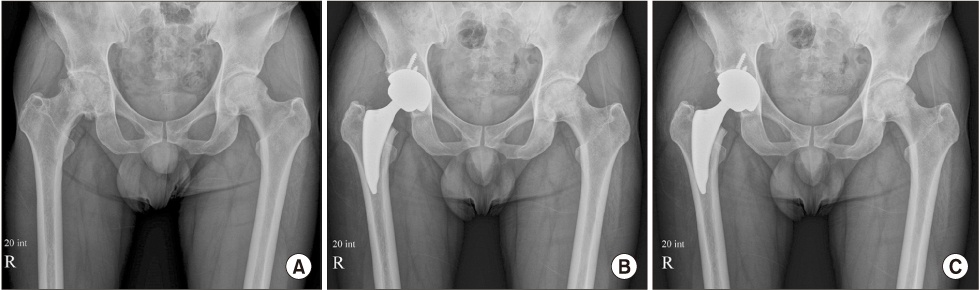
Total hip arthroplasty was performed using a direct anterior approach (DAA) on an ordinary operation table and a short femoral stem. The clinical radiographic results were evaluated by a comparison with those performed using the modified hardinge (anterolateral approach, ALA) method.
MATERIALS AND METHODS
From January 2013 to November 2015, 102 patients who underwent total hip arthroplasty using DAA (DAA group) and the same number of patients using ALA (ALA group), both performed by a single surgeon, were compared and analyzed retrospectively. The operation time and amounts of bleeding were compared, and the improvement in post-operative pain, ambulatory capacity and functional recovery of the hip joint were checked. The location of insertion of the acetabular cup and femoral stem were evaluated radiologically, and the complications that occurred in the two groups were investigated.
RESULTS
The amount of bleeding was significantly smaller in the DAA group (p=0.018). Up to 3 weeks postoperatively, recovery of hip muscle strength was significantly higher in the DAA group (flexion/extension strength p=0.023, abduction strength p=0.031). The Harris hip score was significantly better in the DAA group for up to 3 months (p<0.001) and the Koval score showed significantly better results in the DAA group up to 6 weeks (p≤0.001). The visual analogue scale score improvement was significantly higher in the DAA group by day 7 (p=0.035). The inclination angle (p<0.001) and anteversion angle (p<0.001) of the acetabular cup were located in the safe zone of the DAA group more than in the ALA group, and there was no statistically significant difference in the position of the femur stem and leg length difference. During surgery, two cases of greater trochanter fracture occurred in the DAA group (p=0.155).
CONCLUSION
The DAA performed in the ordinary operation table using a short femoral stem showed post-operative early functional recovery. Because a simple to use fluoroscope was used during surgery with an anatomical position familiar to the surgeon, it is considered to be useful for the insertion of implants into the desired position and for an approach that is useful for the prevention of leg length differences.
Keyword
MeSH Terms
Figure
Reference
-
1. Smith-Petersen MN. A new supra-articular subperiosteal approach to the hip joint. J Bone Joint Surg. 1917; 2:592–595.2. Burwell HN, Scott D. A lateral intermuscular approach to the hip joint for replacement of the femoral head by a prosthesis. J Bone Joint Surg Br. 1954; 36:104–108.
Article3. Harris WH. A new lateral approach to the hip joint. J Bone Joint Surg Am. 1967; 49:891–898.
Article4. Iyer KM. A new posterior approach to the hip joint. Injury. 1981; 13:76–80.
Article5. Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg Br. 1982; 64:17–19.
Article6. Berend KR, Lombardi AV Jr, Seng BE, Adams JB. Enhanced early outcomes with the anterior supine intermuscular approach in primary total hip arthroplasty. J Bone Joint Surg Am. 2009; 91:Suppl 6. 107–120.
Article7. Kennon RE, Keggi JM, Wetmore RS, Zatorski LE, Huo MH, Keggi KJ. Total hip arthroplasty through a minimally invasive anterior surgical approach. J Bone Joint Surg Am. 2003; 85:Suppl 4. 39–48.
Article8. Parratte S, Pagnano MW. Muscle damage during minimally invasive total hip arthroplasty: cadaver-based evidence that it is significant. Instr Course Lect. 2008; 57:231–234.9. Lovell TP. Single-incision direct anterior approach for total hip arthroplasty using a standard operating table. J Arthroplasty. 2008; 23:64–68.
Article10. Barrett WP, Turner SE, Leopold JP. Prospective randomized study of direct anterior vs postero-lateral approach for total hip arthroplasty. J Arthroplasty. 2013; 28:1634–1638.
Article11. de Steiger RN, Lorimer M, Solomon M. What is the learning curve for the anterior approach for total hip arthroplasty? Clin Orthop Relat Res. 2015; 473:3860–3866.
Article12. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969; 51:737–755.13. Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture. A prospective study in geriatric patients. Clin Orthop Relat Res. 1995; 310:150–159.14. Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978; 60:217–220.
Article15. Chechik O, Khashan M, Lador R, Salai M, Amar E. Surgical approach and prosthesis fixation in hip arthroplasty world wide. Arch Orthop Trauma Surg. 2013; 133:1595–1600.
Article16. Post ZD, Orozco F, Diaz-Ledezma C, Hozack WJ, Ong A. Direct anterior approach for total hip arthroplasty: indications, technique, and results. J Am Acad Orthop Surg. 2014; 22:595–603.17. Matta JM, Shahrdar C, Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res. 2005; 441:115–124.
Article18. Keršič M, Dolinar D, Antolič V, Mavčič B. The impact of leg length discrepancy on clinical outcome of total hip arthroplasty: comparison of four measurement methods. J Arthroplasty. 2014; 29:137–141.
Article19. Berend KR, Mirza AJ, Morris MJ, Lombardi AV Jr. Risk of periprosthetic fractures with direct anterior primary total hip arthroplasty. J Arthroplasty. 2016; 31:2295–2298.
Article20. Yu H, Liu H, Jia M, Hu Y, Zhang Y. A comparison of a short versus a conventional femoral cementless stem in total hip arthroplasty in patients 70 years and older. J Orthop Surg Res. 2016; 11:33.
Article21. Dietrich M, Kabelitz M, Dora C, Zingg PO. Perioperative fractures in cementless total hip arthroplasty using the direct anterior minimally invasive approach: reduced risk with short stems. J Arthroplasty. 2018; 33:548–554.
Article22. Learmonth ID. Conservative stems in total hip replacement. Hip Int. 2009; 19:195–200.
Article23. Hartford JM, Knowles SB. Risk factors for perioperative femoral fractures: cementless femoral implants and the direct anterior approach using a fracture table. J Arthroplasty. 2016; 31:2013–2018.
Article24. van Dijk CM, Bimmel R, Haddad FS. (iv) Surgical approaches in primary total hip arthroplasty – pros and cons. Orthop Trauma. 2009; 23:27–34.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Modified Posterior Approach to Total Hip Arthroplasty
- Posterior Approach to Total Hip Joint Replacement Arthroplasty
- Anterior Approaches in Hip Surgery
- Disadvantage during Perioperative Period of Total Hip Arthroplasty Using the Direct Anterior Approach:a Network Meta-Analysis
- Perioperative Comparison of Hip Arthroplasty Using the Direct Anterior Approach with the Posterolateral Approach