J Gastric Cancer.
2019 Jun;19(2):139-147. 10.5230/jgc.2019.19.e18.
History of Esophagogastric Junction Cancer Treatment and Current Surgical Management in Western Countries
- Affiliations
-
- 1Department of Surgery, Division of Gastrointestinal Surgery, Seoul National University Hospital, Seoul, Korea.
- 2Center of Esophageal and Gastric Surgery, Agaplesion Markus Hospital, Frankfurt, Germany. Arnulf.Hoelscher@fdk.info
- KMID: 2449934
- DOI: http://doi.org/10.5230/jgc.2019.19.e18
Abstract
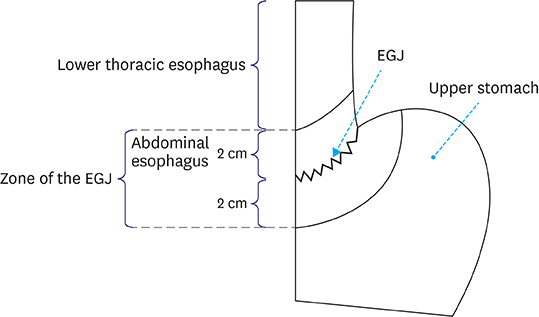
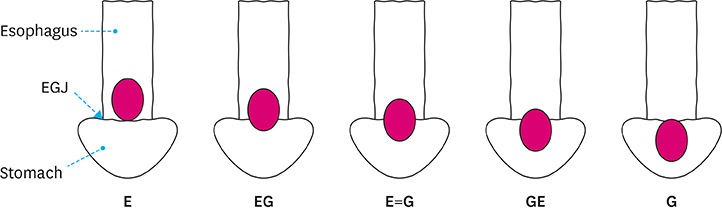
- The incidence of esophagogastric junction (EGJ) cancer has been significantly increasing in Western countries. Appropriate planning for surgical therapy requires a reliable classification of EGJ cancers with respect to their exact location. Clinically, the most accepted classification of EGJ cancers is "adenocarcinoma of the EGJ" (AEG or "Siewert"), which divides tumor center localization into AEG type I (distal esophagus), AEG type II ("true junction"), and AEG type III (subcardial stomach). Treatment strategies in western countries routinely employ perioperative chemotherapy or neoadjuvant chemoradiation for cases of locally advanced cancers. The standard surgical treatment strategies are esophagectomy for AEG type I and gastrectomy for AEG type III cancers. For "true junctional cancers," i.e., AEG type II, whether the extension of resection in the oral or aboral direction represents the most effective surgical therapy remains debatable. This article reviews the history of surgical EGJ cancer treatment and current surgical strategies from a Western perspective.
Figure
Reference
-
1. Global Burden of Disease Cancer Collaboration. Fitzmaurice C, Dicker D, Pain A, Hamavid H, Moradi-Lakeh M, et al. The global burden of cancer 2013. JAMA Oncol. 2015; 1:505–527.2. Buas MF, Vaughan TL. Epidemiology and risk factors for gastroesophageal junction tumors: understanding the rising incidence of this disease. Semin Radiat Oncol. 2013; 23:3–9.
Article3. Sonnenberg A. Time trends of mortality from gastric cancer in Europe. Dig Dis Sci. 2011; 56:1112–1118.
Article4. Siewert JR, Hölscher AH, Becker K, Gössner W. Cardia cancer: attempt at a therapeutically relevant classification. Chirurg. 1987; 58:25–32.5. Siewert JR, Stein HJ. Classification of adenocarcinoma of the oesophagogastric junction. Br J Surg. 1998; 85:1457–1459.
Article6. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011; 14:101–112.7. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017; 20:1–19.8. Hulscher JB, van Sandick JW, de Boer AG, Wijnhoven BP, Tijssen JG, Fockens P, et al. Extended transthoracic resection compared with limited transhiatal resection for adenocarcinoma of the esophagus. N Engl J Med. 2002; 347:1662–1669.
Article9. Briez N, Piessen G, Torres F, Lebuffe G, Triboulet JP, Mariette C. Effects of hybrid minimally invasive oesophagectomy on major postoperative pulmonary complications. Br J Surg. 2012; 99:1547–1553.10. Berlth F, Plum PS, Chon SH, Gutschow CA, Bollschweiler E, Hölscher AH. Total minimally invasive esophagectomy for esophageal adenocarcinoma reduces postoperative pain and pneumonia compared to hybrid esophagectomy. Surg Endosc. 2018; 32:4957–4965.
Article11. Bonavina L, Scolari F, Aiolfi A, Bonitta G, Sironi A, Saino G, et al. Early outcome of thoracoscopic and hybrid esophagectomy: propensity-matched comparative analysis. Surgery. 2016; 159:1073–1081.
Article12. Schmidt HM, Gisbertz SS, Moons J, Rouvelas I, Kauppi J, Brown A, et al. Defining benchmarks for transthoracic esophagectomy: a multicenter analysis of total minimally invasive esophagectomy in low risk patients. Ann Surg. 2017; 266:814–821.13. Low DE, Kuppusamy MK, Alderson D, Cecconello I, Chang AC, Darling G, et al. Benchmarking complications associated with esophagectomy. Ann Surg. 2019; 269:291–298.
Article14. Seesing MF, Gisbertz SS, Goense L, van Hillegersberg R, Kroon HM, Lagarde SM, et al. A propensity score matched analysis of open versus minimally invasive transthoracic esophagectomy in the Netherlands. Ann Surg. 2017; 266:839–846.
Article15. Sasako M, Sano T, Yamamoto S, Sairenji M, Arai K, Kinoshita T, et al. Left thoracoabdominal approach versus abdominal-transhiatal approach for gastric cancer of the cardia or subcardia: a randomised controlled trial. Lancet Oncol. 2006; 7:644–651.
Article16. Siewert JR, Stein HJ. Carcinoma of the cardia: carcinoma of the gastroesophageal junction - classification, pathology and extent of resection. Dis Esophagus. 1996; 9:173–182.17. Kim HH, Han SU, Kim MC, Kim W, Lee HJ, Ryu SW, et al. Effect of laparoscopic distal gastrectomy vs open distal gastrectomy on long-term survival among patients with stage I gastric cancer: the KLASS-01 randomized clinical trial. JAMA Oncol. 2019; 5:506–513.18. Katai H, Mizusawa J, Katayama H, Takagi M, Yoshikawa T, Fukagawa T, et al. Short-term surgical outcomes from a phase III study of laparoscopy-assisted versus open distal gastrectomy with nodal dissection for clinical stage IA/IB gastric cancer: Japan Clinical Oncology Group Study JCOG0912. Gastric Cancer. 2017; 20:699–708.
Article19. Takiguchi S, Miyazaki Y, Shinno N, Makino T, Takahashi T, Kurokawa Y, et al. Laparoscopic mediastinal dissection via an open left diaphragm approach for advanced Siewert type II adenocarcinoma. Surg Today. 2016; 46:129–134.
Article20. Rüdiger Siewert J, Feith M, Werner M, Stein HJ. Adenocarcinoma of the esophagogastric junction: results of surgical therapy based on anatomical/topographic classification in 1,002 consecutive patients. Ann Surg. 2000; 232:353–361.21. Lerut T, Nafteux P, Moons J, Coosemans W, Decker G, De Leyn P, et al. Three-field lymphadenectomy for carcinoma of the esophagus and gastroesophageal junction in 174 R0 resections: impact on staging, disease-free survival, and outcome: a plea for adaptation of TNM classification in upper-half esophageal carcinoma. Ann Surg. 2004; 240:962–972.22. Yamashita H, Seto Y, Sano T, Makuuchi H, Ando N, Sasako M, et al. Results of a nation-wide retrospective study of lymphadenectomy for esophagogastric junction carcinoma. Gastric Cancer. 2017; 20:69–83.
Article23. Al-Batran SE, Goetze TO, Mueller DW, Vogel A, Winkler M, Lorenzen S, et al. The RENAISSANCE (AIO-FLOT5) trial: effect of chemotherapy alone vs. chemotherapy followed by surgical resection on survival and quality of life in patients with limited-metastatic adenocarcinoma of the stomach or esophagogastric junction - a phase III trial of the German AIO/CAO-V/CAOGI. BMC Cancer. 2017; 17:893.
Article24. Moehler M, Al-Batran SE, Andus T, Anthuber M, Arends J, Arnold D, et al. German S3-guideline "diagnosis and treatment of esophagogastric cancer". Z Gastroenterol. 2011; 49:461–531.25. Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006; 355:11–20.
Article26. Ychou M, Boige V, Pignon JP, Conroy T, Bouché O, Lebreton G, et al. Perioperative chemotherapy compared with surgery alone for resectable gastroesophageal adenocarcinoma: an FNCLCC and FFCD multicenter phase III trial. J Clin Oncol. 2011; 29:1715–1721.
Article27. van Hagen P, Hulshof MC, van Lanschot JJ, Steyerberg EW, van Berge Henegouwen MI, Wijnhoven BP, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 2012; 366:2074–2084.
Article28. Japan Esophageal Society. Japanese classification of esophageal cancer, 11th edition: part II and III. Esophagus. 2017; 14:37–65.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adenocarcinoma of the Esophagogastric Junction: Clinicopathological Characteristics
- Treatment of Adenocarcinoma of the Esophagogastric Junction
- Mediastinal Lymph Node Dissection in Gastroesophageal Junction Adenocarcinoma
- Multimodal Treatment Strategies in Esophagogastric Junction Cancer: a Western Perspective
- A Case of Early Adenocarcinoma at Esophagogastric Junction Treated with Cap-pitted Endoscopic Mucosal Resection