Clin Endosc.
2019 May;52(3):288-292. 10.5946/ce.2018.128.
Pneumoperitoneum after Endoscopic Duodenal Stent Insertion in a Patient with Percutaneous Transhepatic Biliary Drainage and Biliary Stent: A Case Report
- Affiliations
-
- 1Department of Internal Medicine, Chungbuk National University Hospital, Cheongju, Korea. smpark@chungbuk.ac.kr
- 2Department of Radiology, Chungbuk National University Hospital, Cheongju, Korea.
- 3Department of Internal Medicine, Chungbuk National University College of Medicine, Cheongju, Korea.
- KMID: 2449772
- DOI: http://doi.org/10.5946/ce.2018.128
Abstract
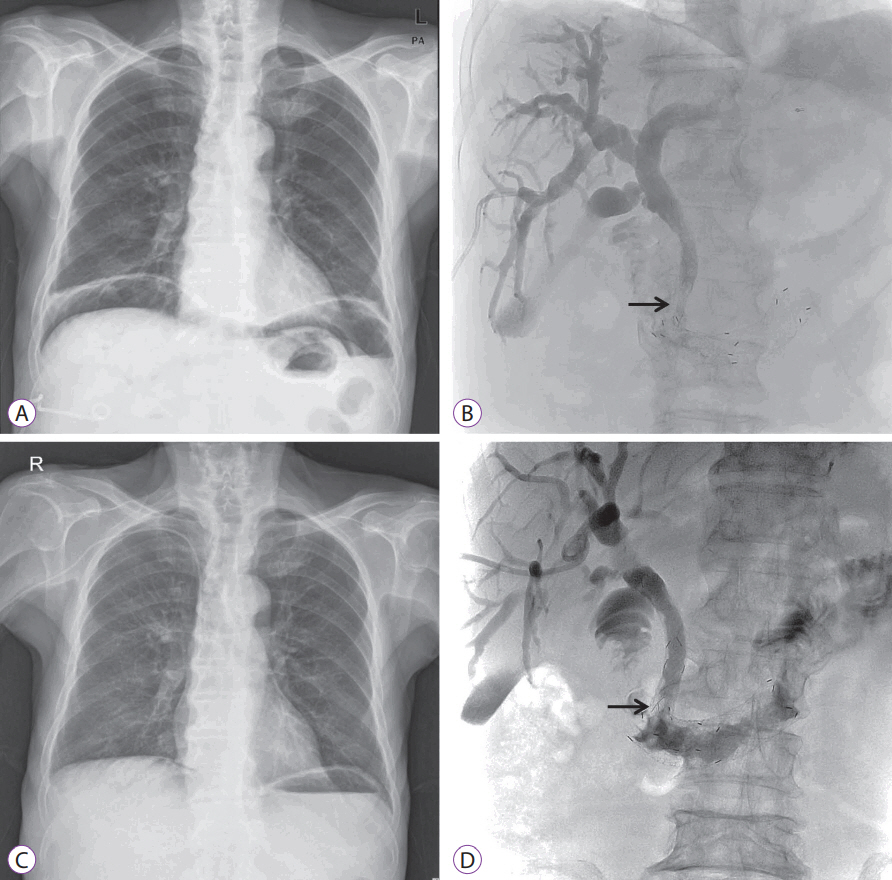
- Early removal of a percutaneous transhepatic biliary drainage (PTBD) tube commonly causes pneumoperitoneum. However, we encountered a patient who developed pneumoperitoneum even with an indwelling PTBD tube. An 84-year-old man was admitted with type III combined duodenal and biliary obstruction secondary to metastatic bladder cancer. A biliary stent was placed using a percutaneous approach, and a duodenal stent was placed endoscopically. A large amount of subphrenic free air was detected after the procedures. Laboratory tests indicated intestinal perforation; however, peritoneal signs were absent. The patient was treated conservatively using an indwelling Levin tube. Seven days later, the massive amount of subphrenic free air disappeared. Follow-up tubography revealed unrestricted bile flow into the small intestine, and the PTBD tube was removed. Prolonged endoscopic procedures in patients with a PTBD tract communicating with the gastrointestinal tract can precipitate pneumoperitoneum. Clinicians should be careful to avoid misdiagnosing this condition as intestinal perforation.
Keyword
MeSH Terms
Figure
Reference
-
1. Lee JH, Lee DH, Yu JS, Lee SJ, Kwon WC, Kim KW. Pneumoperitoneum caused by transhepatic air leak after metallic biliary stent placement. Cardiovasc Intervent Radiol. 2000; 23:482–484.
Article2. Amonkar SJ, Laasch HU, Valle JW. Pneumoperitoneum following percutaneous biliary intervention: not necessarily a cause for alarm. Cardiovasc Intervent Radiol. 2008; 31:439–443.
Article3. Hui YT, Lam WM, Lam TW, Cheung WC, Sze SF, Wong CT. Benign pneumoperitoneum developed after endoscopic biliary metallic stent placement with the rendezvous procedure. Gastrointest Endosc. 2008; 67:179–180.
Article4. Chuang CH, Chen CY, Tsai HM. Pneumoperitoneum caused by air leakage through the percutaneous puncture tract as a complication of rendezvous technique: a case report. Kaohsiung J Med Sci. 2008; 24:614–617.
Article5. Virgilio E, Chieco PA, Salaj A, et al. Conservative management of pneumoperitonitis after percutaneous transhepatic insertion of metallic biliary stents. Am Surg. 2015; 81:E418–E419.
Article6. Jonnalagadda S, Azar R. Avoiding pneumomediastinum during ERCP after percutaneous transhepatic biliary drainage. Gastrointest Endosc. 2008; 68:809. author reply 809-810.
Article7. Baron TH. Management of simultaneous biliary and duodenal obstruction: the endoscopic perspective. Gut Liver. 2010; 4 Suppl 1:S50–S56.
Article8. Lisle DA, Hunter JC, Pollard CW, Borrowdale RC. Percutaneous gelfoam embolization of chronic enterocutaneous fistulas: report of three cases. Dis Colon Rectum. 2007; 50:251–256.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous transhepatic access to allow per-oral enteric stent insertion for malignant duodenal obstruction following failed endoscopic attempt
- Endoscopic Reintervention for Recurrence of Malignant Biliary Obstruction: Developing the Best Strategy
- Two Double Stents Insertion for Commen Bile Duct and Duodenal Obstruction Caused by Pancreatic Cancer
- Endoscopic Stent Placement in the Palliation of Malignant Biliary Obstruction
- Percutaneous Endoscopic Biliary Stent (PEBS): A case report