Acute Crit Care.
2019 Feb;34(1):46-52. 10.4266/acc.2018.00388.
Characteristics and Outcomes of Potentially Inappropriate Admissions to the Intensive Care Unit
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. realrain7@gmail.com
- KMID: 2449379
- DOI: http://doi.org/10.4266/acc.2018.00388
Abstract
- BACKGROUND
Admission of patients perceived as potentially inappropriate for intensive care is a very sensitive and controversial issue. We aimed to evaluate the use of medical resources in the intensive care unit (ICU) and outcomes of patients according to a physician's judgment of appropriateness.
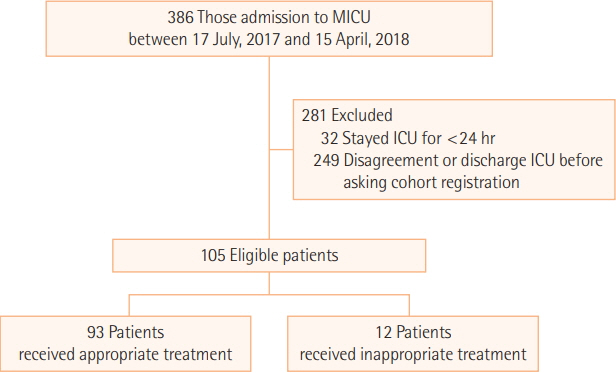
METHODS
ICU physicians classified patients who were admitted to the medical ICU of a tertiary hospital as appropriate or inappropriate for intensive care within 24 hours of admission. Patient outcomes including mortality were analyzed according to appropriateness. Additionally, the usage and duration of mechanical ventilation (MV), renal replacement therapy (RRT), and extracorporeal membrane oxygenation (ECMO) were analyzed according to appropriateness.
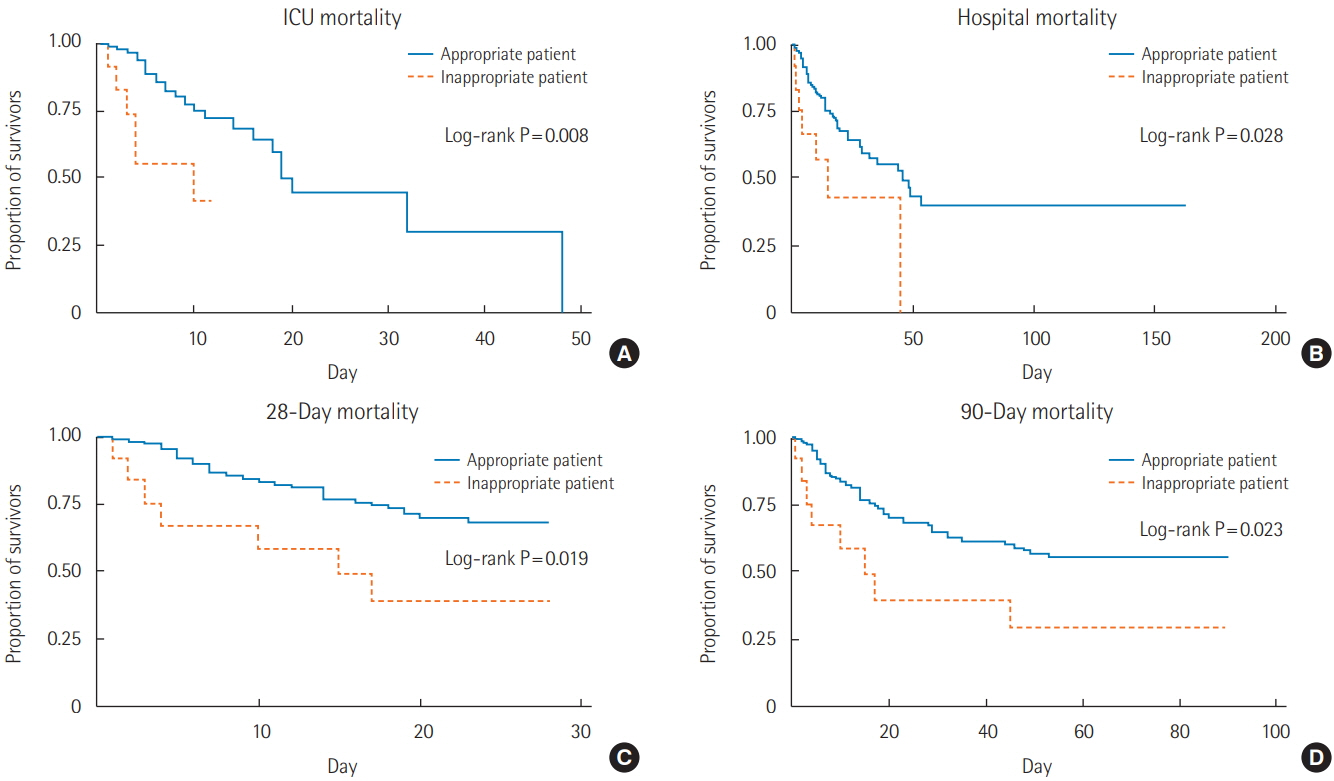
RESULTS
In total, 105 patients (male, 55.4%; mean age, 62 years) were included. Twelve (11.4%) patients were considered inappropriate for intensive care based on guidance published by the Society of Critical Care Medicine through a questionnaire survey of physicians. There was no significant difference between patients considered inappropriate or appropriate for ICU admission regarding the use and duration of MV, RRT, and ECMO. In contrast, the ICU, in-hospital, 28-day, 90-day, and total mortality rates were significantly higher among patients with inappropriate admission than among patients with appropriate admission (ICU mortality: 50.0% vs. 25.8%, P=0.008; in-hospital mortality: 58.3% vs. 43.0%, P=0.028; 28-day mortality: 58.3% vs. 33.3%, P=0.019; 90-day mortality: 66.7% vs. 44.1%, P=0.023).
CONCLUSIONS
Despite higher mortality, the amount of medical resources used for patients considered potentially inappropriate for intensive care did not differ from the resources used for patients considered suitable for ICU care.
MeSH Terms
Figure
Reference
-
1. Huynh TN, Kleerup EC, Raj PP, Wenger NS. The opportunity cost of futile treatment in the ICU. Crit Care Med. 2014; 42:1977–82.
Article2. Angus DC, Barnato AE, Linde-Zwirble WT, Weissfeld LA, Watson RS, Rickert T, et al. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med. 2004; 32:638–43.
Article3. Riley GF, Lubitz JD. Long-term trends in Medicare payments in the last year of life. Health Serv Res. 2010; 45:565–76.
Article4. Neville TH, Ziman A, Wenger NS. Blood products provided to patients receiving futile critical care. J Hosp Med. 2017; 12:739–42.
Article5. Huynh TN, Kleerup EC, Wiley JF, Savitsky TD, Guse D, Garber BJ, et al. The frequency and cost of treatment perceived to be futile in critical care. JAMA Intern Med. 2013; 173:1887–94.
Article6. Palda VA, Bowman KW, McLean RF, Chapman MG. “Futile” care: do we provide it? Why? A semistructured, Canada-wide survey of intensive care unit doctors and nurses. J Crit Care. 2005; 20:207–13.
Article7. Kim J, Choi SM, Park YS, Lee CH, Lee SM, Yim JJ, et al. Factors influencing the initiation of intensive care in elderly patients and their families: a retrospective cohort study. Palliat Med. 2016; 30:789–99.
Article8. Phua J, Joynt GM, Nishimura M, Deng Y, Myatra SN, Chan YH, et al. Withholding and withdrawal of life-sustaining treatments in intensive care units in Asia. JAMA Intern Med. 2015; 175:363–71.
Article9. Lee SJ, Kim HY. Experience of life-sustaining treatment in patient care among intensive care unit nurses: phenomenological approach. J Korean Acad Fundam Nurs. 2016; 23:172–83.
Article10. Ministry of the Interior and Safety. Resident registration statistics. Seoul: Ministry of the Interior and Safety;2018.11. Korean act on hospice-palliative care and life-sustaining treatment decision-making, Act No. 14013 (February 3, 2016).12. Kon AA, Shepard EK, Sederstrom NO, Swoboda SM, Marshall MF, Birriel B, et al. Defining futile and potentially inappropriate interventions: a policy statement from the Society of Critical Care Medicine Ethics Committee. Crit Care Med. 2016; 44:1769–74.13. Neville TH, Wiley JF, Yamamoto MC, Flitcraft M, Anderson B, Curtis JR, et al. Concordance of nurses and physicians on whether critical care patients are receiving futile treatment. Am J Crit Care. 2015; 24:403–10.
Article14. Garrouste-Orgeas M, Montuclard L, Timsit JF, Misset B, Christias M, Carlet J. Triaging patients to the ICU: a pilot study of factors influencing admission decisions and patient outcomes. Intensive Care Med. 2003; 29:774–81.
Article15. Chang DW, Dacosta D, Shapiro MF. Priority levels in medical intensive care at an academic public hospital. JAMA Intern Med. 2017; 177:280–1.
Article16. Makino J, Fujitani S, Twohig B, Krasnica S, Oropello J. End-oflife considerations in the ICU in Japan: ethical and legal perspectives. J Intensive Care. 2014; 2:9.
Article17. Koh Y. Current status of end-of-life care in Korean hospitals. J Korean Med Assoc. 2012; 55:1171–7.
Article18. Ho A, Tsai DF. Making good death more accessible: end-of-life care in the intensive care unit. Intensive Care Med. 2016; 42:1258–60.
Article19. Joynt GM, Gomersall CD, Tan P, Lee A, Cheng CA, Wong EL. Prospective evaluation of patients refused admission to an intensive care unit: triage, futility and outcome. Intensive Care Med. 2001; 27:1459–65.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unanticipated Post-anesthesia Admission to the Pediatric Intensive Care Unit
- Can the intensivists predict the outcomes of critically ill patients on the appropriateness of intensive care unit admission for limited intensive care unit resources ?
- A Clinical Analysis of Intensive Care Unit Admissions Using APACHE II Scoring System
- Predictive Factors of Intensive Care Unit Readmission among Older Patients: A Retrospective Study
- Cardiac Complications in Patients Admitted to the Neuro-Intensive Care Unit