Acute Crit Care.
2019 May;34(2):126-132. 10.4266/acc.2018.00283.
Utility of the early lactate area score as a prognostic marker for septic shock patients in the emergency department
- Affiliations
-
- 1Department of Emergency Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. chrisryoo@amc.seoul.kr
- KMID: 2449366
- DOI: http://doi.org/10.4266/acc.2018.00283
Abstract
- BACKGROUND
The current Surviving Sepsis Campaign guidelines recommend the remeasurement of lactate levels if the initial lactate level is elevated; however, the prognostic value of lactate kinetics is limited and inconsistent. We attempted to determine the efficacy of the lactate area score (calculated from repeated lactate measurements during initial resuscitation) as a prognostic marker of septic shock in the emergency department (ED).
METHODS
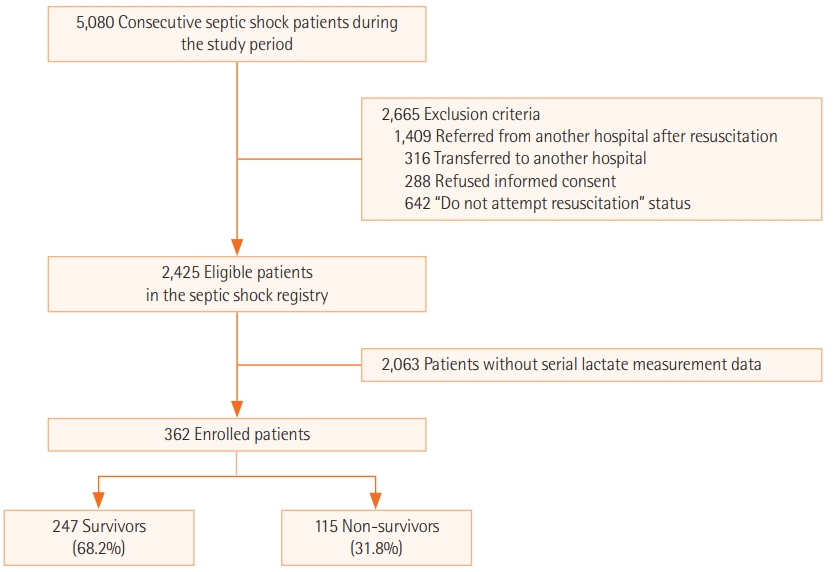
We performed a retrospective study of adult patients with septic shock in the ED of a single tertiary medical center. Serial lactate levels were measured five times within 12 hours. We also compared the initial lactate level, maximum lactate level, and lactate area score. The lactate area score was defined as the sum of the area under the curve measured at 2, 4, 6, and 12 hours following the initial measurement.
RESULTS
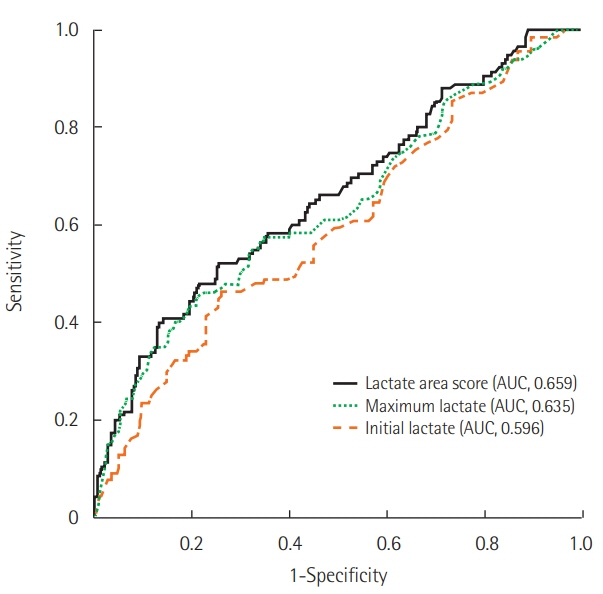
A total of 362 patients were enrolled in this study, and the overall 28-day mortality was 31.8%. The lactate area score of serial lactate levels as well as the initial (median [interquartile range], 4.9 [3.4 to 10.5]; P=0.003) and maximum (7.3 [4.2 to 13.2]; P<0.001) lactate levels were significantly higher in the non-survivor group. However, in multivariate analysis, only the lactate area score (odds ratio, 1.013; 95% confidence interval, 1.007 to 1.019) was significantly associated with 28-day mortality.
CONCLUSIONS
The early lactate area score may be a possible prognostic marker for predicting the 28-day mortality of adult septic shock patients. Further prospective interventional studies should be conducted to validate our results.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Recent lactate findings: is repeated serum lactate testing necessary in septic shock patients?
Moo Suk Park
Acute Crit Care. 2019;34(2):155-157. doi: 10.4266/acc.2019.00528.Usefulness of presepsin in predicting the prognosis of patients with sepsis or septic shock: a retrospective cohort study
Jeong Suk Koh, Yoon Joo Kim, Da Hyun Kang, Jeong Eun Lee, Song-I Lee
Yeungnam Univ J Med. 2021;38(4):318-325. doi: 10.12701/yujm.2021.01018.
Reference
-
1. Shankar-Hari M, Phillips GS, Levy ML, Seymour CW, Liu VX, Deutschman CS, et al. Developing a new definition and assessing new clinical criteria for septic shock: for the third international consensus definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016; 315:775–87.2. Levy MM, Evans LE, Rhodes A. The surviving sepsis campaign bundle: 2018 update. Crit Care Med. 2018; 46:997–1000.
Article3. Jansen TC, van Bommel J, Bakker J. Blood lactate monitoring in critically ill patients: a systematic health technology assessment. Crit Care Med. 2009; 37:2827–39.
Article4. Jansen TC, van Bommel J, Mulder PG, Rommes JH, Schieveld SJ, Bakker J. The prognostic value of blood lactate levels relative to that of vital signs in the pre-hospital setting: a pilot study. Crit Care. 2008; 12:R160.
Article5. Jansen TC, van Bommel J, Woodward R, Mulder PG, Bakker J. Association between blood lactate levels, Sequential Organ Failure Assessment subscores, and 28-day mortality during early and late intensive care unit stay: a retrospective observational study. Crit Care Med. 2009; 37:2369–74.
Article6. Suetrong B, Walley KR. Lactic acidosis in sepsis: it’s not all anaerobic: implications for diagnosis and management. Chest. 2016; 149:252–61.7. Ryoo SM, Kim WY. Clinical applications of lactate testing in patients with sepsis and septic shock. J Emerg Crit Care Med. 2018; 2:14.
Article8. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016; 315:801–10.
Article9. Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017; 43:304–77.10. Nguyen HB, Rivers EP, Knoblich BP, Jacobsen G, Muzzin A, Ressler JA, et al. Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med. 2004; 32:1637–42.
Article11. Scott HF, Brou L, Deakyne SJ, Fairclough DL, Kempe A, Bajaj L. Lactate clearance and normalization and prolonged organ dysfunction in pediatric sepsis. J Pediatr. 2016; 170:149–55. e1-4.
Article12. Sterling SA, Puskarich MA, Jones AE. The effect of liver disease on lactate normalization in severe sepsis and septic shock: a cohort study. Clin Exp Emerg Med. 2015; 2:197–202.
Article13. Wang H, Li Z, Yin M, Chen XM, Ding SF, Li C, et al. Combination of Acute Physiology and Chronic Health Evaluation II score, early lactate area, and N-terminal prohormone of brain natriuretic peptide levels as a predictor of mortality in geriatric patients with septic shock. J Crit Care. 2015; 30:304–9.
Article14. Ryoo SM, Lee J, Lee YS, Lee JH, Lim KS, Huh JW, et al. Lactate level versus lactate clearance for predicting mortality in patients with septic shock defined by Sepsis-3. Crit Care Med. 2018; 46:e489–95.
Article15. Ryoo SM, Ahn R, Lee J, Sohn CH, Seo DW, Huh JW, et al. Timing of repeated lactate measurement in patients with septic shock at the emergency department. Am J Med Sci. 2018; 356:97–102.
Article16. Shin J, Hwang SY, Jo IJ, Kim WY, Ryoo SM, Kang GH, et al. Prognostic value of the lactate/albumin ratio for predicting 28-day mortality in critically ill sepsis patients. Shock. 2018; 50:545–50.
Article17. Kim YA, Ha EJ, Jhang WK, Park SJ. Early blood lactate area as a prognostic marker in pediatric septic shock. Intensive Care Med. 2013; 39:1818–23.
Article18. Casserly B, Phillips GS, Schorr C, Dellinger RP, Townsend SR, Osborn TM, et al. Lactate measurements in sepsis-induced tissue hypoperfusion: results from the Surviving Sepsis Campaign database. Crit Care Med. 2015; 43:567–73.19. Arnold RC, Shapiro NI, Jones AE, Schorr C, Pope J, Casner E, et al. Multicenter study of early lactate clearance as a determinant of survival in patients with presumed sepsis. Shock. 2009; 32:35–9.
Article20. Bolvardi E, Malmir J, Reihani H, Hashemian AM, Bahramian M, Khademhosseini P, et al. The role of lactate clearance as a predictor of organ dysfunction and Mortality in patients with severe sepsis. Mater Sociomed. 2016; 28:57–60.
Article21. Lokhandwala S, Andersen LW, Nair S, Patel P, Cocchi MN, Donnino MW. Absolute lactate value vs relative reduction as a predictor of mortality in severe sepsis and septic shock. J Crit Care. 2017; 37:179–84.
Article22. Ryoo SM, Kim WY, Sohn CH, Seo DW, Koh JW, Oh BJ, et al. Prognostic value of timing of antibiotic administration in patients with septic shock treated with early quantitative resuscitation. Am J Med Sci. 2015; 349:328–33.
Article23. Ilias I, Apollonatou S, Vassiliadi DA, Nikitas N, Theodorakopoulou M, Diamantakis A, et al. Adipose tissue lactate clearance but not blood lactate clearance is associated with clinical outcome in sepsis or septic shock during the post-resuscitation period. Metabolites. 2018; 8:E28.
Article24. Driessen RG, van de Poll MC, Mol MF, van Mook WN, Schnabel RM. The influence of a change in septic shock definitions on intensive care epidemiology and outcome: comparison of sepsis-2 and sepsis-3 definitions. Infect Dis (Lond). 2018; 50:207–13.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lactate Clearance as a Prognostic Factor of Organ Failure in Sepsis
- Serum lactate levels in cirrhosis and non-cirrhosis patients with septic shock
- The Usefulness of Lactate Clearance Adjusted to Time as a Predictive Index in Patients with Severe Sepsis and Septic Shock
- Lactic Acidosis as a Prognostic Factor and a Therapeutic Guideline for Severe Sepsis and Septic Shock
- Lactate Clearance and Outcome in Septic Shock Patients with Low Level of Initial Lactate