Hip Pelvis.
2019 Mar;31(1):40-47. 10.5371/hp.2019.31.1.40.
The Majority of Corona Mortis Are Small Calibre Venous Blood Vessels: A Cadaveric Study of North Indians
- Affiliations
-
- 1Department of Orthopaedics, Indira Gandhi Medical College, Shimla, India. drsk73@rediffmail.com
- 2Department of Anatomy, Indira Gandhi Medical College, Shimla, India.
- 3Department of Anaesthesia and Intensive Care, Indira Gandhi Medical College, Shimla, India.
- KMID: 2448040
- DOI: http://doi.org/10.5371/hp.2019.31.1.40
Abstract
- PURPOSE
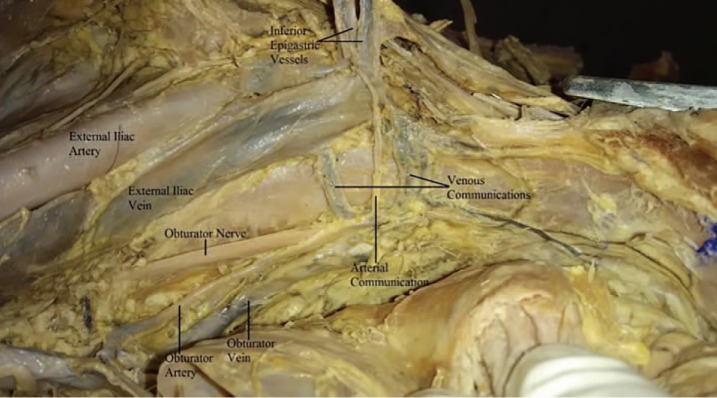
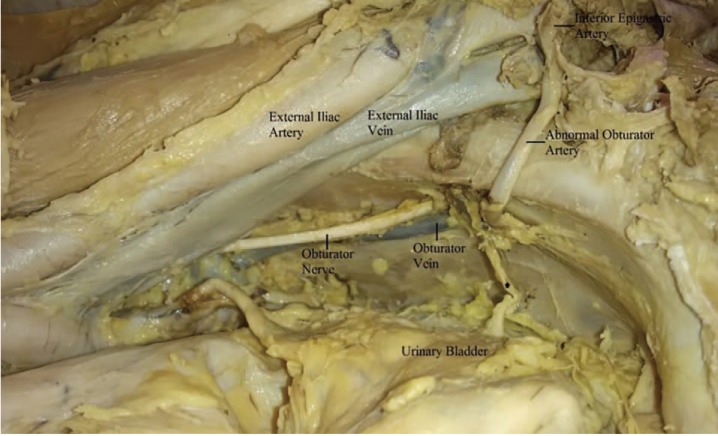
Corona mortis is an abnormal arterial or venous anastomosis between the external iliac and the obturator system of vessels and may cause significant hemorrhage during pelvi-acetabular fracture surgeries, hernia repair and laparoscopic gynecological procedures. Previous studies have estimated a prevalence of corona mortis between 34% and 70%. This cadaveric study was conducted to estimate the prevalence of corona mortis in the North Indian population.
MATERIALS AND METHODS
Twelve cadavers (24 hemipelvises; 11 males and 1 female) with a mean age of 68 (range, 54-82) years were included in this study.
RESULTS
Corona mortis was observed in 14 hemipelvises (58.3%). A total of 19 (79.2%) vascular anastomoses of diameter greater than 1 mm were observed; 5 hemipelvises (20.8%) had corona mortis on the right side, 9 hemipelvises (37.5%) on the left side and bilateral in 5 (41.7%) cases. Two hemipelvises (8.3%) had an arterial connection. An aberrant obturator artery was observed in 1 (4.2%) hemipelvis. A venous connection was found in 14 specimens (58.3% of hemipelvises). The average distance of the connecting vein from the symphysis pubis was 41 (35-70) mm. A vessel diameter of greater than 4 mm was observed in 4/24 (16.7%) of hemipelvises.
CONCLUSION
The frequency of venous corona mortis was higher than arterial corona mortis and the majority (83.3%) were small calibre ( < 4 mm). The presentation pattern and the number of arterial or venous anastomoses were different in the majority of hemipelvises and dissimilar in both hemipelvises of the same cadaver in the majority of cases.
Keyword
MeSH Terms
Figure
Reference
-
1. Sarikcioglu L, Sindel M, Akyildiz F, Gur S. Anastomotic vessels in the retropubic region: corona mortis. Folia Morphol (Warsz). 2003; 62:179–182. PMID: 14507043.2. Teague DC, Graney DO, Routt ML Jr. Retropubic vascular hazards of the ilioinguinal exposure: a cadaveric and clinical study. J Orthop Trauma. 1996; 10:156–159. PMID: 8667106.
Article3. Hong HX, Pan ZJ, Chen X, Huang ZJ. An anatomical study of corona mortis and its clinical significance. Chin J Traumatol. 2004; 7:165–169. PMID: 15294115.4. Marsman JW, Schilstra SH, van Leeuwen H. Angiography and embolization of the corona mortis (aberrant obturator artery). A source of persistent pelvic bleeding. Rofo. 1984; 141:708–710. PMID: 6440242.5. Berberoğlu M, Uz A, Ozmen MM, et al. Corona mortis: an anatomic study in seven cadavers and an endoscopic study in 28 patients. Surg Endosc. 2001; 15:72–75. PMID: 11210207.6. Stavropoulou-Deli A, Anagnostopoulou S. Corona mortis: anatomical data and clinical considerations. Aust N Z J Obstet Gynaecol. 2013; 53:283–286. PMID: 23551084.
Article7. Letournel E. The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop Relat Res. 1993; (292):62–76.
Article8. Letournel E, Judet R. Fractures of the acetabulum. 2nd ed. Berlin: Springer;1993.9. Tornetta P 3rd, Hochwald N, Levine R. Corona mortis. Incidence and location. Clin Orthop Relat Res. 1996; (329):97–101. PMID: 8769440.10. Pungpapong SU, Thum-umnauysuk S. Incidence of corona mortis: preperitoneal anatomy for laparoscopic hernia repair. J Med Assoc Thai. 2005; 88:S51–S53.11. Darmanis S, Lewis A, Mansoor A, Bircher M. Corona mortis: an anatomical study with clinical implications in approaches to the pelvis and acetabulum. Clin Anat. 2007; 20:433–439. PMID: 16944498.
Article12. Okcu G, Erkan S, Yercan HS, Ozic U. The incidence and location of corona mortis: a study on 75 cadavers. Acta Orthop Scand. 2004; 75:53–55. PMID: 15022807.13. Rusu MC, Cergan R, Motoc AG, Folescu R, Pop E. Anatomical considerations on the corona mortis. Surg Radiol Anat. 2010; 32:17–24. PMID: 19636491.
Article14. Pellegrino A, Damiani GR, Marco S, Ciro S, Cofelice V, Rosati F. Corona mortis exposition during laparoscopic procedure for gynecological malignancies. Updates Surg. 2014; 66:65–68. PMID: 24390752.
Article15. Nayak SB, Deepthinath R, Prasad AM, Shetty SD, Aithal AP. A South Indian cadaveric study on obturator neurovascular bundle with a special emphasis on high prevalence of ‘venous corona mortis’. Injury. 2016; 47:1452–1455. PMID: 27156835.
Article16. Ates M, Kinaci E, Kose E, et al. Corona mortis: in vivo anatomical knowledge and the risk of injury in totally extraperitoneal inguinal hernia repair. Hernia. 2016; 20:659–665. PMID: 26621137.
Article17. Kacra BK, Arazi M, Cicekcibasi AE, Büyükmumcu M, Demirci S. Modified medial Stoppa approach for acetabular fractures: an anatomic study. J Trauma. 2011; 71:1340–1344. PMID: 21768909.
Article18. Missankov AA, Asvat R, Maoba KI. Variations of the pubic vascular anastomoses in black South Africans. Acta Anat (Basel). 1996; 155:212–214. PMID: 8870790.
Article19. Jakubowicz M, Czarniawska-Grzesiñska M. Variability in origin and topography of the inferior epigastric and obturator arteries. Folia Morphol (Warsz). 1996; 55:121–126. PMID: 8908792.20. Maneesha S, Tripta S, Richhpal S, et al. Variations of obturator artery in man. Anat Physiol. 2012; 2:105.
Article21. Al Talalwah W. A new concept and classification of corona mortis and its clinical significance. Chin J Traumatol. 2016; 19:251–254. PMID: 27780502.
Article22. Skandalakis LJ, Androulakis J, Colborn GL, Skandalakis JE. Obturator hernia. Embryology, anatomy, and surgical applications. Surg Clin North Am. 2000; 80:71–84. PMID: 10685145.23. Jensen KO, Sprengel K, Mica L, Somlyay L, Jentzsch T, Werner CML. Surgical relevance of corona mortis and clinical outcome in pelvic trauma. Austin J Anat. 2015; 2:1033.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Deceased Male with a Cigarette In Situ : Is This a Cadaveric Spasm?
- Massive Hemorrhage Caused by a Non-Displaced Pubic Ramus Fracture from Low-Energy Trauma
- Comparison of Gas Analysis in Arterial and Venous Blood during Inspiration of High Oxygen Concentration
- Two Cases of Venous Hemangioma
- An Experimental Evaluation of Microvascular Grafts