Anesth Pain Med.
2019 Apr;14(2):216-221. 10.17085/apm.2019.14.2.216.
Painless cervical motor radiculopathy relieved by cervical epidural steroid injection: A case report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Kangdong Sacred Heart Hospital, Seoul, Korea. kssege@naver.com
- KMID: 2447973
- DOI: http://doi.org/10.17085/apm.2019.14.2.216
Abstract
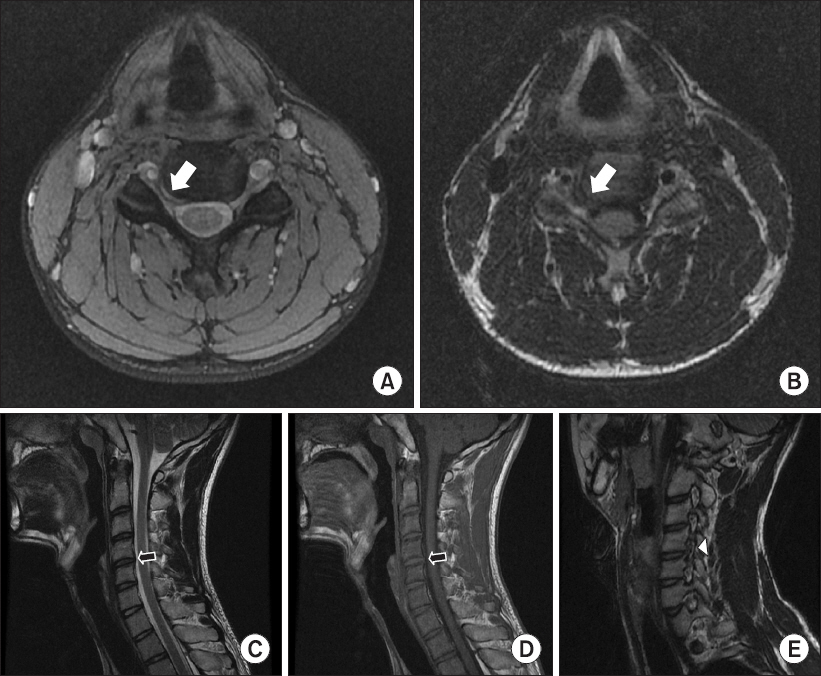
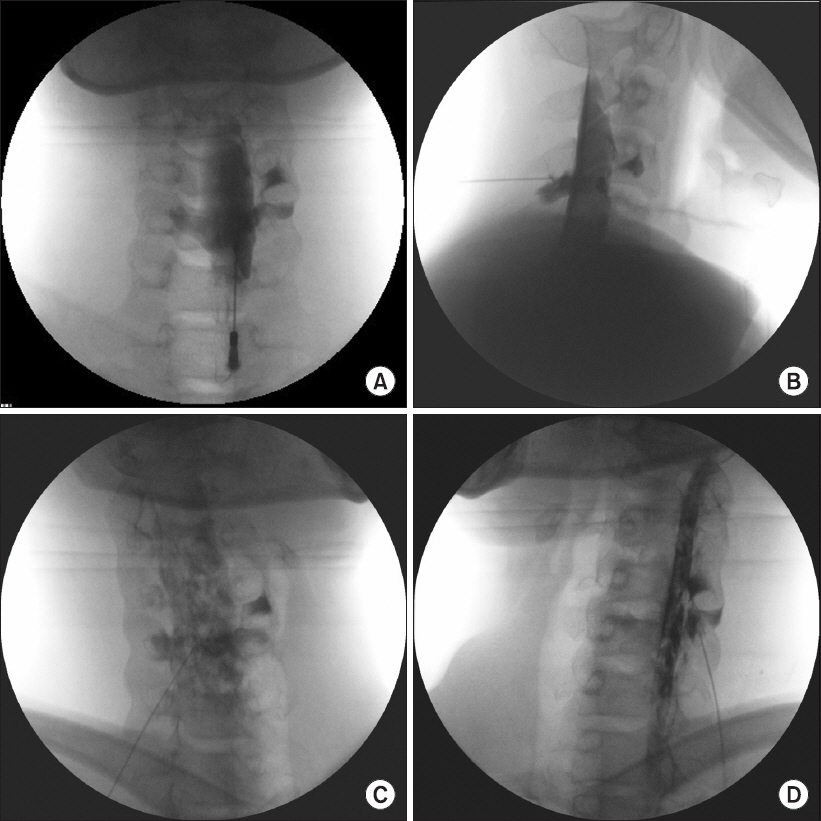
- A 15-year-old male patient presented with a slow progression of painless right shoulder weakness over the previous six weeks. The magnetic resonance imaging revealed right C4-5 foraminal stenosis caused by right foraminal disc protrusion. The needle electromyography and nerve conduction studies revealed acute C5 and/or C6 radiculopathy. Instead of the initial surgical management modalities, we performed a cervical epidural steroid injection at the C4-5 level. From the day after the patient received the cervical epidural steroid injection, his right shoulder motor weakness improved progressively. Two weeks after the procedure, his right shoulder motor function had fully recovered.
Keyword
MeSH Terms
Figure
Reference
-
1. Carette S, Fehlings MG. Clinical practice. Cervical radiculopathy. N Engl J Med. 2005; 353:392–9. DOI: 10.1056/NEJMcp043887. PMID: 16049211.2. Cooper RG, Freemont AJ, Hoyland JA, Jenkins JP, West CG, Il- lingworth KJ, et al. Herniated intervertebral disc-associated periradicular fibrosis and vascular abnormalities occur without inflammatory cell infiltration. Spine (Phila Pa 1976). 1995; 20:591–8. DOI: 10.1097/00007632-199503010-00016.3. Chabot MC, Montgomery DM. The pathophysiology of axial and radicular neck pain. Semin Spine Surg. 1995; 7:2–8.4. Rao R. Neck pain, cervical radiculopathy, and cervical myelopathy: pathophysiology, natural history, and clinical evaluation. Instr Course Lect. 2003; 52:479–88. PMID: 12690874.5. Woods BI, Hilibrand AS. Cervical radiculopathy: epidemiology, etiology, diagnosis, and treatment. J Spinal Disord Tech. 2015; 28:E251–9. DOI: 10.1097/BSD.0000000000000284. PMID: 25985461.6. Siller S, Kasem R, Witt TN, Tonn JC, Zausinger S. Painless motor radiculopathy of the cervical spine: clinical and radiological characteristics and long-term outcomes after operative decompression. J Neurosurg Spine. 2018; 28:621–9. DOI: 10.3171/2017.10.SPINE17821. PMID: 29570047.7. Honet JC, Ellenberg MR. What you always wanted to know about the history and physical examination of neck pain but were afraid to ask. Phys Med Rehabil Clin N Am. 2003; 14:473–91. DOI: 10.1016/S1047-9651(03)00039-1.8. Henderson CM, Hennessy RG, Shuey HM Jr, Shackelford EG. Posterior-lateral foraminotomy as an exclusive operative technique for cervical radiculopathy: a review of 846 consecutively operated cases. Neurosurgery. 1983; 13:504–12. DOI: 10.1227/00006123-198311000-00004. PMID: 6316196.9. Pyhtinen J, Laitinen J. Cervical intervertebral foramen narrowing and myelographic nerve root sleeve deformities. Neuroradiology. 1993; 35:596–7. DOI: 10.1007/BF00588403. PMID: 8278040.10. Han JJ, Kraft GH. Electrodiagnosis of neck pain. Phys Med Rehabil Clin N Am. 2003; 14:549–67. DOI: 10.1016/S1047-9651(03)00036-6.11. Partanen J, Partanen K, Oikarinen H, Niemitukia L, Hernesniemi J. Preoperative electroneuromyography and myelography in cervical root compression. Electromyogr Clin Neurophysiol. 1991; 31:21–6. PMID: 2009821.12. Wong JJ, Côté P, Quesnele JJ, Stern PJ, Mior SA. The course and prognostic factors of symptomatic cervical disc herniation with radiculopathy: a systematic review of the literature. Spine J. 2014; 14:1781–9. DOI: 10.1016/j.spinee.2014.02.032. PMID: 24614255.13. Byeon GJ, Choi EJ, Choi YM, Chang EJ, Kim HJ, Kim KH. Oblique interlaminar lumbar epidural steroid injection for management of low back pain with lumbosacral radicular pain: a case report. Anesth Pain Med. 2017; 12:375–80. DOI: 10.17085/apm.2017.12.4.375.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of Cervical Radiculopathy with Epidural Steroid Injection
- Epidural Steroid Injection in the Treatment of Cervical Radiculopathy
- Treatment of Cervical Perineural Cyst by the Transforaminal Epidural Steroid Injection
- Acute Cervical Subdural Hematoma with Quadriparesis after Cervical Transforaminal Epidural Block
- Intramedullary Spinal Cord Hemorrhage Associated with Monoparesis after Transforaminal Cervical Epidural Steroid Injection