Yonsei Med J.
2019 Jun;60(6):535-541. 10.3349/ymj.2019.60.6.535.
Effect of Cardiac Rehabilitation on Outcomes in Patients with ST-Elevation Myocardial Infarction
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea. byungokim@paik.ac.kr
- 2Division of Cardiology, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2446958
- DOI: http://doi.org/10.3349/ymj.2019.60.6.535
Abstract
- PURPOSE
Whether cardiac rehabilitation (CR) improves clinical outcomes in patients with ST-elevation myocardial infarction (STEMI) undergoing primary percutaneous coronary intervention (PCI) with drug-eluting stents (DESs) has not been thoroughly evaluated. Moreover, few studies have sought to identify patients who would benefit most from CR among STEMI patients.
MATERIALS AND METHODS
Consecutively, 265 STEMI patients who underwent primary PCI with implantation of DESs and follow-up angiography were examined. Seventy-six patients (30%) who received CR were assigned to the CR+ group. Another 178 patients (70%) who did not participate in CR were assigned to the CR− group. Second generation DESs were implanted in 238 (94%) patients.
RESULTS
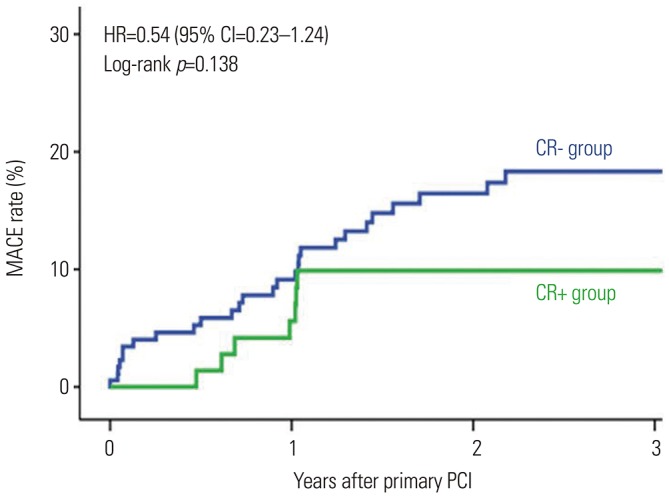
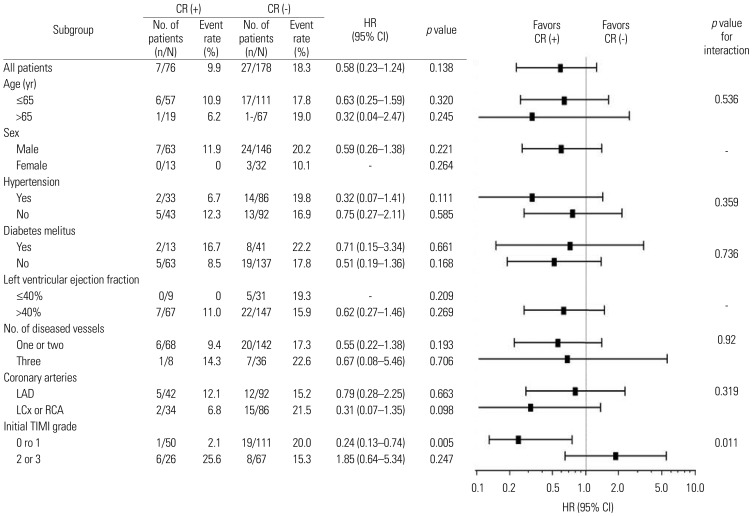
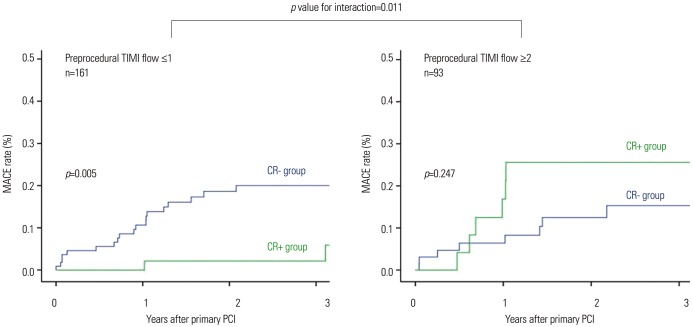
Major adverse cardiovascular events (MACEs), including death, myocardial infarction, and revascularization, were compared. The CR+ group tended to have lower MACE than the CR− group at 3 years, although the difference was not statistically significant (9.9% vs. 18.3%, hazard ratio=0.54, p=0.138). Subgroup analysis revealed a significant interaction according to CR and preprocedural thrombolysis in myocardial infarction (TIMI) flow (p value for interaction=0.011). In patients with low preprocedural TIMI flow (TIMI flow ≤1, n=161), those in the CR+ group had significantly lower MACE than those in the CR− group (p=0.005), whereas MACE was not different among patients with higher TIMI flow (TIMI flow ≥2, n=93).
CONCLUSION
CR including exercise training was associated with lower MACE, particularly in patients with lower preprocedural TIMI flow during primary PCI for STEMI in the current DES era.
MeSH Terms
Figure
Reference
-
1. Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004; 116:682–692. PMID: 15121495.
Article2. Clark AM, Hartling L, Vandermeer B, McAlister FA. Meta-analysis: secondary prevention programs for patients with coronary artery disease. Ann Intern Med. 2005; 143:659–672. PMID: 16263889.
Article3. Hambrecht R, Walther C, Möbius-Winkler S, Gielen S, Linke A, Conradi K, et al. Percutaneous coronary angioplasty compared with exercise training in patients with stable coronary artery disease: a randomized trial. Circulation. 2004; 109:1371–1378. PMID: 15007010.4. Pouche M, Ruidavets JB, Ferrières J, Iliou MC, Douard H, Lorgis L, et al. Cardiac rehabilitation and 5-year mortality after acute coronary syndromes: The 2005 French FAST-MI study. Arch Cardiovasc Dis. 2016; 109:178–187. PMID: 26711546.
Article5. Cottin Y, Cambou JP, Casillas JM, Ferrières J, Cantet C, Danchin N. Specific profile and referral bias of rehabilitated patients after an acute coronary syndrome. J Cardiopulm Rehabil. 2004; 24:38–44. PMID: 14758102.
Article6. Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, Stason WB. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007; 116:1653–1662. PMID: 17893274.
Article7. Lee HY, Kim JH, Kim BO, Byun YS, Cho S, Goh CW, et al. Regular exercise training reduces coronary restenosis after percutaneous coronary intervention in patients with acute myocardial infarction. Int J Cardiol. 2013; 167:2617–2622. PMID: 22795710.
Article8. Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, et al. Academic Research Consortium. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007; 115:2344–2351. PMID: 17470709.9. Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of myocardial infarction. Circulation. 2012; 126:2020–2035. PMID: 22923432.
Article10. Hammill BG, Curtis LH, Schulman KA, Whellan DJ. Relationship between cardiac rehabilitation and long-term risks of death and myocardial infarction among elderly Medicare beneficiaries. Circulation. 2010; 121:63–70. PMID: 20026778.
Article11. Writing Committee Members. Thomas RJ, King M, Lui K, Oldridge N, Piña IL, Spertus J. AACVPR/ACCF/AHA 2010 update: performance measures on cardiac rehabilitation for referral to cardiac rehabilitation/secondary prevention services: a report of the American Association of Cardiovascular and Pulmonary Rehabilitation and the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures (Writing Committee to Develop Clinical Performance Measures for Cardiac Rehabilitation). Circulation. 2010; 122:1342–1350. PMID: 20805435.12. Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011; 124:2458–2473. PMID: 22052934.13. Sabaté M, Brugaletta S, Cequier A, Iñiguez A, Serra A, Jiménez-Quevedo P, et al. Clinical outcomes in patients with ST-segment elevation myocardial infarction treated with everolimus-eluting stents versus bare-metal stents (EXAMINATION): 5-year results of a randomised trial. Lancet. 2016; 387:357–366. PMID: 26520230.
Article14. Sabaté M, Räber L, Heg D, Brugaletta S, Kelbaek H, Cequier A, et al. Comparison of newer-generation drug-eluting with bare-metal stents in patients with acute ST-segment elevation myocardial infarction: a pooled analysis of the EXAMINATION (clinical Evaluation of the Xience-V stent in Acute Myocardial INfArcTION) and COMFORTABLE-AMI (Comparison of Biolimus Eluted From an Erodible Stent Coating With Bare Metal Stents in Acute ST-Elevation Myocardial Infarction) trials. JACC Cardiovasc Interv. 2014; 7:55–63. PMID: 24332419.15. Palmerini T, Biondi-Zoccai G, Della Riva D, Mariani A, Sabaté M, Valgimigli M, et al. Clinical outcomes with drug-eluting and bare-metal stents in patients with ST-segment elevation myocardial infarction: evidence from a comprehensive network meta-analysis. J Am Coll Cardiol. 2013; 62:496–504. PMID: 23747778.16. Joost A, Stiermaier T, Eitel C, Fuernau G, de Waha S, Desch S, et al. Impact of initial culprit vessel flow on infarct size, microvascular obstruction, and myocardial salvage in acute reperfused ST-elevation myocardial infarction. Am J Cardiol. 2016; 118:1316–1322. PMID: 27600465.
Article17. Stone GW, Cox D, Garcia E, Brodie BR, Morice MC, Griffin J, et al. Normal flow (TIMI-3) before mechanical reperfusion therapy is an independent determinant of survival in acute myocardial infarction: analysis from the primary angioplasty in myocardial infarction trials. Circulation. 2001; 104:636–641. PMID: 11489767.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Cardiac Rehabilitation in Patients with ST Elevation Myocardial Infarction and Non-ST Elevation Myocardial Infarction
- Differences in Clinical Outcomes Between Patients With ST-Elevation Versus Non-ST-Elevation Acute Myocardial Infarction in Korea
- Coronary Slow Flow Phenomenon Leads to ST Elevation Myocardial Infarction
- A Case of Pericardial Effusion after Acute Myocardial Infarction
- A Case of Cardiac Metastasis from Lung Cancer Presented with Persistent ST Segment Elevation Simulating Acute Myocardial Infarction