Neurointervention.
2019 Mar;14(1):27-34. 10.5469/neuroint.2018.01074.
Efficiency of Air Bubble Removal in Preparation of Low-Profile Angioplasty Balloon Catheter: Bench-Top Comparison of Six Methods
- Affiliations
-
- 1Department of Radiology, Research Institute of Radiology, Asan Medical Center, Seoul, Korea. dhlee@amc.seoul.kr
- 2Department of Medical Science, Graduate School of Soonchunhyang University, Ansan, Korea.
- 3Departmet of Radiology, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2446779
- DOI: http://doi.org/10.5469/neuroint.2018.01074
Abstract
- PURPOSE
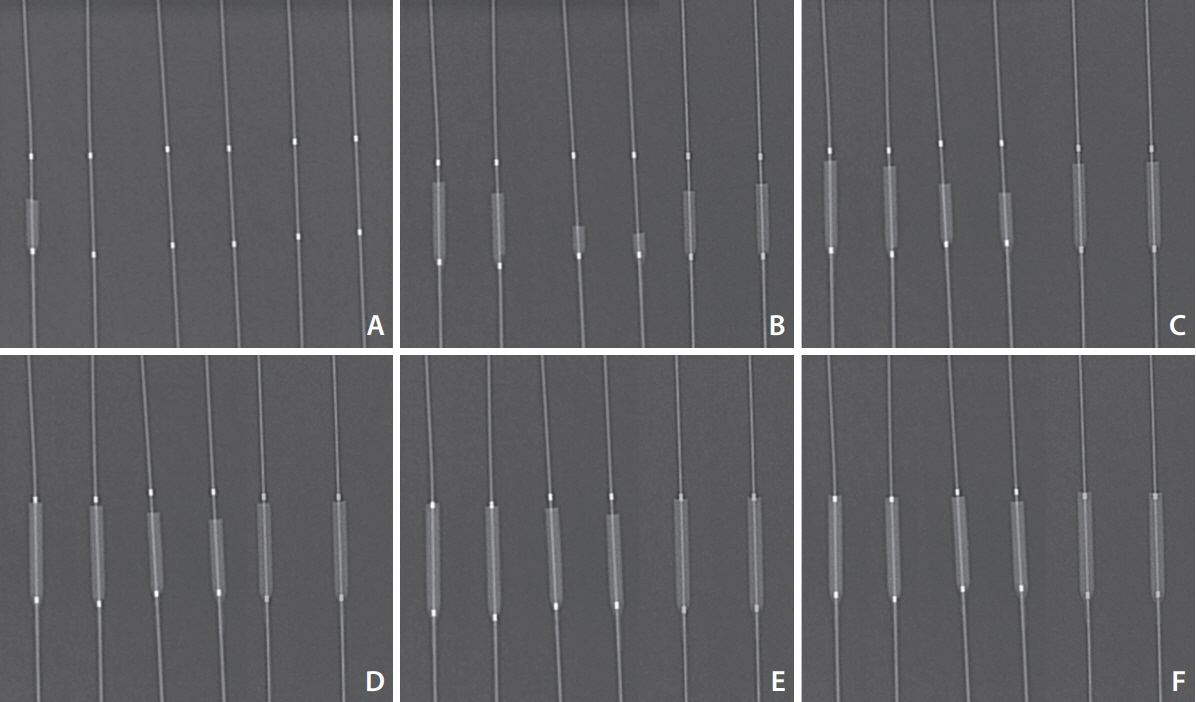
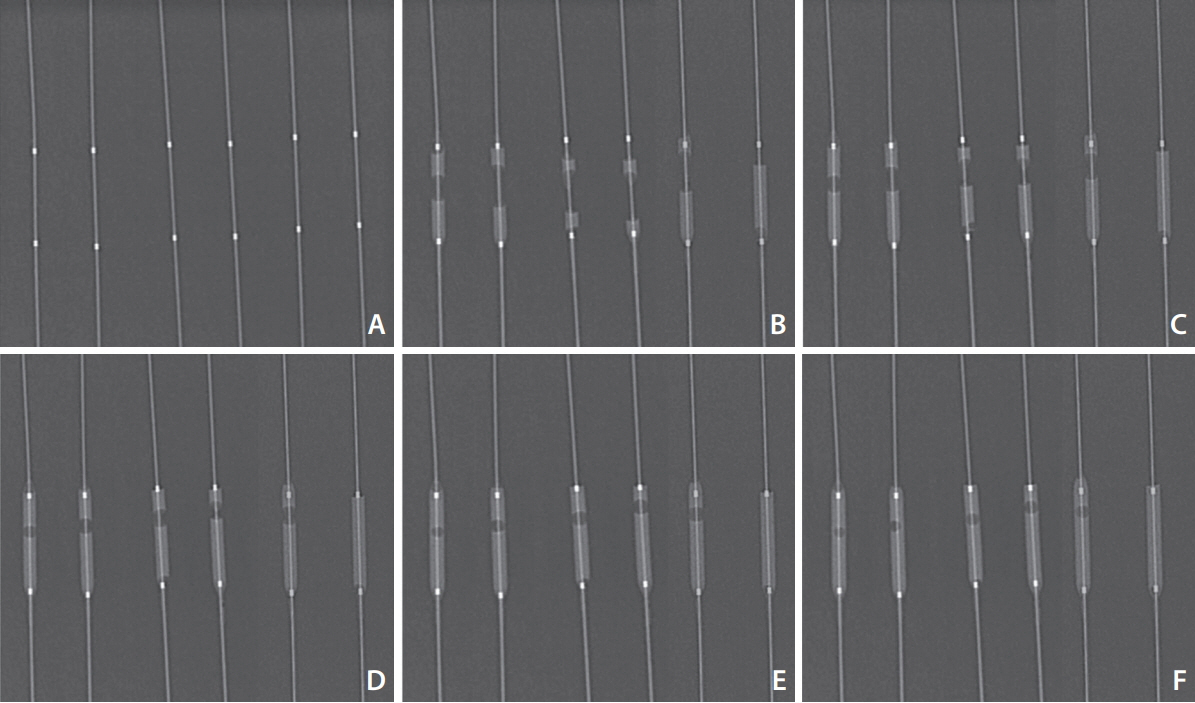
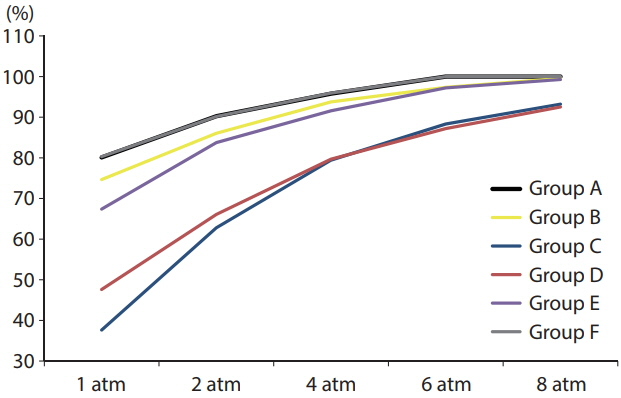
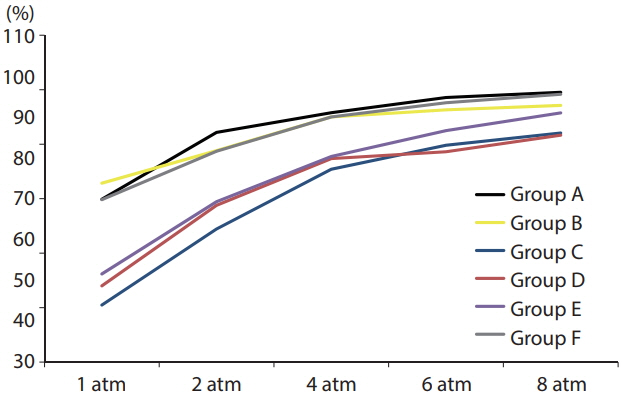
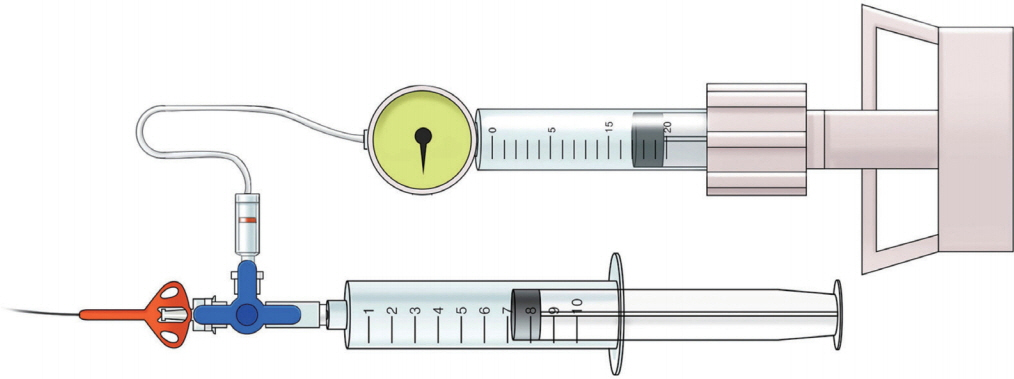
Complete removal of air bubbles from balloons for neurovascular angioplasty is cumbersome. We compared the preparation difficulty, air removal efficiency, and air collection pattern of six different balloon catheter preparation methods to propose a better preparation method for both initial and second balloon uses, especially for small-profile angioplasty balloon catheters. MATERIALS AND METHODS: A total of 18 neurovascular angioplasty balloon catheters with nominal diameters of 2 mm were prepared to test six different preparation methods: the instruction for use method (method A), simplified method using a syringe (method B) and four newly devised preparation methods using inflating devices (methods C-F). Serial radiographs were obtained while the balloons were gradually inflated. We measured the time for each preparation and the bubble number, analyzed their distribution in the balloon, and calculated the contrast filling ratio (contrast filling area/total balloon area) for initial and second ballooning. The whole process was repeated three times.
RESULTS
The preparation time varied widely (11.5 seconds [method D] to 73.3 seconds [method A]). On initial inflation, the contrast filling ratio at 8 atm was the highest (100%) with methods A and F. On second inflation, the ratio was again highest with method A (99.5%), followed by method F (99.2%). Initial ballooning tended to show a uniform pattern of single bubble in the distal segment of the balloon; in contrast, second ballooning showed varying patterns in which the bubbles were multiple and randomly distributed.
CONCLUSION
None of the six methods were able to completely exclude air bubbles from the balloon catheters including the second ballooning; however, the method of repeating aspiration with high-volume inflating device (method F) could be a practical option considering the simplicity and efficiency of preparation.
MeSH Terms
Figure
Reference
-
1. Fiorella D, Chow MM, Anderson M, Woo H, Rasmussen PA, Masaryk TJ. A 7-year experience with balloon-mounted coronary stents for the treatment of symptomatic vertebrobasilar intracranial atheromatous disease. Neurosurgery. 2007; 61:236–242. ; discussion 242-243.
Article2. Karanam LSP, Sharma M, Alurkar A, Baddam SR, Pamidimukkala V, Polavarapu R. Balloon angioplasty for intracranial atherosclerotic disease: a multicenter study. J Vasc Interv Neurol. 2017; 9:29–34.3. Suh DC, Kim JK, Choi JW, Choi BS, Pyun HW, Choi YJ, et al. Intracranial stenting of severe symptomatic intracranial stenosis: results of 100 consecutive patients. AJNR Am J Neuroradiol. 2008; 29:781–785.
Article4. Kim KS, Hwang DH, Ko YH, Kang IW, Lee ES, Han YM, et al. Usefulness of stent implantation for treatment of intracranial atherosclerotic stenoses. Neurointervention. 2012; 7:27–33.
Article5. Chang HW, Shin SH, Suh SI, Jeong HW, Suh DC. Recommendations for carotid stenting in Korea. Neurointervention. 2015; 10:7–13.
Article6. Connors JJ 3rd, Wojak JC, Hoppe BH. The technique of endovascular intracranial revascularization. Front Neurol. 2014; 5:246.
Article7. Chaudhry NS, Orning JL, Shakur SF, Amin-Hanjani S, Aletich VA, Charbel FT, et al. Safety and efficacy of balloon angioplasty of the anterior cerebral artery for vasospasm treatment after subarachnoid hemorrhage. Interv Neuroradiol. 2017; 23:372–377.
Article8. Bartolini B, Blanc R, Pistocchi S, Redjem H, Ciccio G, Piotin M. TransForm occlusion balloon catheter for the treatment of intracranial aneurysms, initial experience. Interv Neuroradiol. 2015; 21:155–160.
Article9. Okamura A, Kuroki K, Shinagawa K, Yamada N. Simple aspiration with balloon catheter technique (simple ABC technique) against proximal internal carotid artery occlusion in cases of cardiogenic cerebral embolism. Interv Neuroradiol. 2018; 24:317–321.
Article10. Rigatelli G, Dell’Avvocata F, Giordan M, Cardaioli P. Air embolism caused by balloon rupture resolved by manual thrombectomy catheter aspiration. Cardiovasc Revasc Med. 2011; 12:129–130.
Article11. Kahn JK, Hartzler GO. The spectrum of symptomatic coronary air embolism during balloon angioplasty: causes, consequences, and management. Am Heart J. 1990; 119:1374–1377.
Article12. O’Neill L, Sowbhaga V, Owens P. Fracture, inflation and floatation embolisation of PTCA balloon. BMJ Case Rep. 2015; 2015:bcr2014205307.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Coarctation of the Aorta Treated with Balloon Angioplasty
- Rupture, Breakdown, and Pulmonary Artery Embolism of a Balloon Catheter Tip during Percutaneous Transluminal Angioplasty of Arteriovenous Fistula
- Air Bubble in Acute Extradural Hematomas
- Catheter Interventions for Kawasaki Disease: Current Concepts and Future Directions
- Clinical Experience with a Hybrid Procedure Using the Adherent Clot Catheter for Salvage of Thrombosed Hemodialysis Access: A Comparison with the Standard Fogarty Balloon Catheter