Obstet Gynecol Sci.
2019 May;62(3):194-198. 10.5468/ogs.2019.62.3.194.
Diagnosis of an indistinct Leydig cell tumor by positron emission tomography-computed tomography
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. beanpearl@yuhs.ac
- 2Department of Obstetrics and Gynecology, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2445080
- DOI: http://doi.org/10.5468/ogs.2019.62.3.194
Abstract
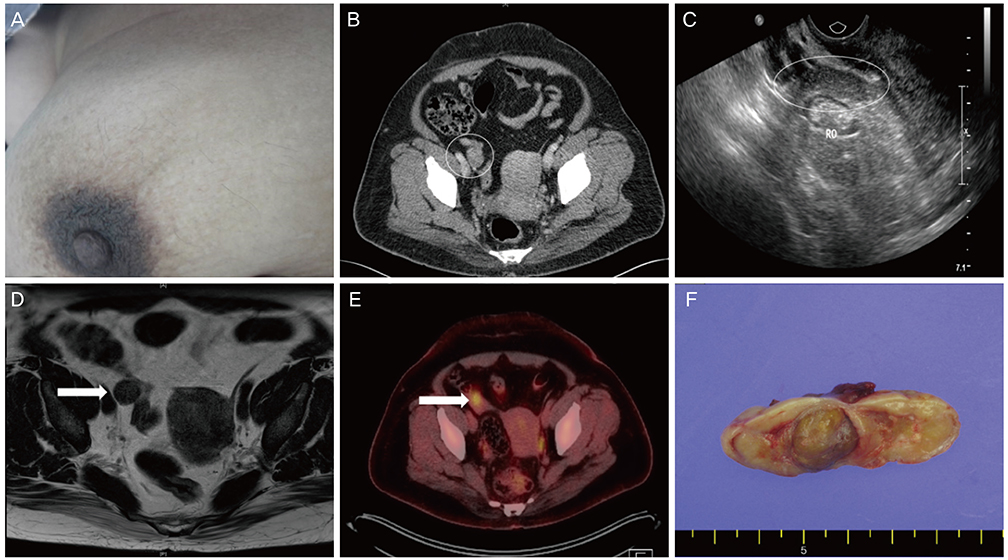
- A 51-year-old perimenopausal female patient presented with hirsutism and voice thickening which was started approximately one and a half years ago. Her initial hormone assay revealed elevated plasma testosterone, 5a-dihydrotestosterone, and dehydroepiandrosterone (DHEA) levels and therefore androgen-secreting tumor was first suspected. However, the lesion was inconspicuous on transvaginal sonography, abdominal-pelvic computed tomography (CT) scan, and pelvic magnetic resonance (MRI) imaging. Consequently, 18F-fluorodeoxyglucose (FDG) positron emission tomography-CT was performed, which localized the lesion as a focal FDG uptake within the right adnexa. Total laparoscopic hysterectomy with bilateral salpingo-oophorectomy was performed, and although visible gross mass lesions were not observed intraoperatively, pure Leydig cell tumor was pathologically confirmed within the right ovary. Plasma testosterone, 5a-dihydrotestosterone, and DHEA levels were normalized postoperatively. Clinical signs of virilization were also significantly resolved after 3-months of follow-up.
Keyword
MeSH Terms
Figure
Reference
-
1. Gui T, Cao D, Shen K, Yang J, Zhang Y, Yu Q, et al. A clinicopathological analysis of 40 cases of ovarian Sertoli-Leydig cell tumors. Gynecol Oncol. 2012; 127:384–389.
Article2. Young RH, Scully RE. Ovarian Sertoli-Leydig cell tumors. A clinicopathological analysis of 207 cases. Am J Surg Pathol. 1985; 9:543–569.3. Tekin O, Avci Z, Isik B, Ozkara A, Uraldi C, Catal F, et al. Hirsutism: common clinical problem or index of serious disease? MedGenMed. 2004; 6:56.4. Brojeni NR, Salehian B. Androgen secreting ovarian tumors. MOJ Women's Health. 2017; 5:327–330.
Article5. Demidov VN, Lipatenkova J, Vikhareva O, Van Holsbeke C, Timmerman D, Valentin L. Imaging of gynecological disease (2): clinical and ultrasound characteristics of Sertoli cell tumors, Sertoli-Leydig cell tumors and Leydig cell tumors. Ultrasound Obstet Gynecol. 2008; 31:85–91.
Article6. Tsuzuki Y, Kikuchi I, Nojima M, Yoshida K, Hashizume A, Tomita S. A case report: ovarian Sertoli-Leydig cell tumor with hyperestrogenism and endometrial hyperplasia in a postmenopausal woman. Jpn Clin Med. 2017; 8:1179066017695239.
Article7. Baiocchi G, Manci N, Angeletti G, Celleno R, Fratini D, Gilardi G. Pure Leydig cell tumour (hilus cell) of the ovary: a rare cause of virilization after menopause. Gynecol Obstet Invest. 1997; 44:141–144.
Article8. Levens ED, Whitcomb BW, Csokmay JM, Nieman LK. Selective venous sampling for androgen-producing ovarian pathology. Clin Endocrinol (Oxf). 2009; 70:606–614.
Article9. McCarthy-Keith DM, Hill M, Norian JM, Millo C, McKeeby J, Armstrong AY. Use of F 18-fluoro-D-glucose-positron emission tomography-computed tomography to localize a hilar cell tumor of the ovary. Fertil Steril. 2010; 94:753.e11–753.e14.
Article10. Matuszczyk A, Petersenn S, Lahner H, Haude M, Veit P, Becker JU, et al. Androgenproduzierender Leydig-zell-tumor des ovars als ursache von hirsutismus bei einer postmenopausalen frau. Med Klin Intensivmed Notfmed. 2007; 102:259–262.
Article11. Short S, Hoskin P, Wong W. Ovulation and increased FDG uptake on PET: potential for a false-positive result. Clin Nucl Med. 2005; 30:707.
Article12. Ho KC, Ng KK, Yen TC, Chou HH. An ovary in luteal phase mimicking common iliac lymph node metastasis from a primary cutaneous peripheral primitive neuroectodermal tumour as revealed by 18-fluoro-2-deoxyglucose positron emission tomography. Br J Radiol. 2005; 78:343–345.
Article13. Zhang HY, Zhu JE, Huang W, Zhu J. Clinicopathologic features of ovarian Sertoli-Leydig cell tumors. Int J Clin Exp Pathol. 2014; 7:6956–6964.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- 18F-2-Deoxy-2-Fluoro-D-Glucose Positron Emission Tomography: Computed Tomography for Preoperative Staging in Gastric Cancer Patients
- Oral cancer diagnosed using PET/CT: A case report
- Positron Emission Tomography-CT, CT, and MR Imaging Findings of Tumor-Mimicking Organized Hematoma in the Maxillary Sinus: Two Case Reports
- CT and Positron Emission Tomography/CT Findings of Mediastinal Extraskeletal Ewing's Sarcoma with Extensive Distant Metastasis: A Case Report
- Adult granulosa cell tumor presenting with massive ascites, elevated CA-125 level, and low 18F-fluorodeoxyglucose uptake on positron emission tomography/computed tomography